Chapter 13 The neurological examination and lesion localisation
Key points
 The primary aim of the neurological examination is to localise the lesion.
The primary aim of the neurological examination is to localise the lesion.
 The neurological examination assesses behaviour and arousal, sensory systems, motor function, cranial nerve function, spinal reflexes and, particularly in companion animals spinal hyperpathia (spinal pain). Methods of examination have to be adjusted according to the species being examined.
The neurological examination assesses behaviour and arousal, sensory systems, motor function, cranial nerve function, spinal reflexes and, particularly in companion animals spinal hyperpathia (spinal pain). Methods of examination have to be adjusted according to the species being examined.
The following describes the neurological examination in a domestic cat or dog but the general principles are similar for large animals. Specific comments are given to modify the examination for large animals. This chapter represents the culmination of all the functional neuroanatomy described in chapters 1–12. Please see specific chapters for further details of structure and function.
During the examination, tests are performed that evaluate the following neural functions:
From the results of the tests, the clinician determines:
(a) Whether the animal has neurological deficits;
(b) Which parts of the nervous system are functioning normally;
For example, if the lesion is in the thoracolumbar spinal cord, then pathways passing through that part of the cord may be damaged (see Fig. 13.15), such as proprioception and UMN tracts to the pelvic limbs causing proprioceptive deficits (conscious and subconscious) and either paraparesis or paralysis. But the lesion will not affect the cranial nerves, arousal or the function of the thoracic limbs, as those neural systems are not associated with the thoracolumbar spinal cord (Fig. 13.1).
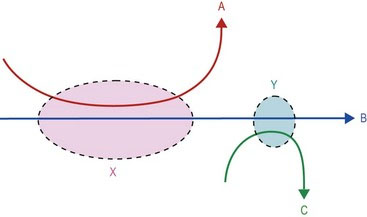
An applied example of this diagram would be the animal that has conscious proprioception deficits on the right side of the body and blindness in the right eye (see Fig. 4.10). The conscious proprioceptive pathway (e.g. ‘B’ in Fig. 13.1) begins in the sensory receptors in the forepaw, travels via spinal nerves into the spinal cord, travels cranially in the ipsilateral cervical spinal cord, into the brainstem, crosses over and passes rostrally on the contralateral side to the somatosensory cortex. The lesion could be anywhere along that long pathway. ‘A’ represents the cranial nerves that attach to the brainstem (III–XII) and the UMN centres in the brainstem and ‘C’ represents the visual pathway. As there are no other cranial nerve deficits, or paresis, then the lesion is unlikely to be in region ‘X’. But both the right-side visual pathway (C) and right side proprioception are associated with the left side of the forebrain. Thus the lesion is in region ‘Y’.
The neurological examination
Observation versus hands-on testing
The functioning of the majority of the nervous system can be assessed by close observation (Fig. 13.2). This is particularly useful if the animal cannot be handled; for example if it is fractious or wild. For animals that you can handle, then observation is still critical for getting an overall impression of neural function and is an excellent opportunity to assess arousal and behaviour. Physical contact usually stimulates the animal and subtle deficits in mental alertness may be missed. Assessing the animal’s arousal level is done best by observing its interaction with the environment. Answering the following questions provides useful information.

Fig. 13.2 What neurological deficit can be observed in this picture of a horse? (Answer on next page.)
Does it respond normally to environmental stimuli? These may include visual, auditory, olfactory, tactile and possibly gustatory stimuli. Does it seem bright, alert and responsive or dull and somnolent? (see Figs. 11.3 and 11.4)
Is the posture of its head, body, limbs and tail normal at rest and during locomotion? (See Fig. 6.2) Does it move normally or are there signs of proprioceptive deficits (stumbling, postural abnormalities), ataxia, stiffness, pain or paresis? If so, which limbs and which joints are functioning normally and which are dysfunctional? Is there any change in muscle bulk?
Observe the head closely. Is the head posture normal? Is there any asymmetry of the face (drooping, muscle wasting)? (see Fig. 10.12) Do the ears, eyelids, eyes and nose move normally? Is it blinking? Is it sniffing at objects? Is it observing things or does it bump into them? Do both eyes track in a coordinated manner? Is there any strabismus, anisocoria or nystagmus? Does it respond to auditory stimuli? Is it swallowing normally or is there any evidence of respiratory stridor or change in voice? Is it licking its lips? Does it prehend food or drink normally?
Are there any signs of autonomic dysfunction such as anisocoria, sweating, faecal or urinary incontinence? (see Fig. 12.6) Spinal reflexes are difficult to assess by observation, but the animal may show a skin twitch if an insect lands on it, or a perineal reflex after defecating or urinating. If the animal has normal posture and gait, then the spinal reflexes are likely to be normal.
The horse in Fig. 13.2 has a left-sided facial nerve paresis. This was due to accidental compression of the facial nerve by the head collar buckle while the horse was recumbent under anaesthesia (see Fig. 10.14B). What do you observe in the horse in Fig. 13.3?
Proprioception and motor function
The horse in Fig. 13.3 has proprioceptive deficits when turning in both the thoracic and the pelvic limbs. Note excessive circumduction of the left pelvic limb and the delayed movement of the left thoracic limb leaving the foot rotated inappropriately inwards.
If only conscious proprioception is compromised the animal may stand and walk with the limbs placed under the centre of gravity, but it may stand on top of the paw, or scuff the paw along the ground during the protraction phase, resulting in stumbling. Large animals, with their poorly developed corticospinal tracts, may have a remarkably normal gait with a forebrain injury; thus more complex manoeuvres are required to expose any deficit. What do you observe in the animals in Fig. 13.4?
Cranial nerve function
Testing cranial nerve function by observation is outlined in Tables 10.2 and 13.1. Note that as cranial nerves are bilaterally paired, both sides of the head need to be checked (see Chapter 10).
Table 13.1 Observing cranial nerve function. Note that blinking is a reflex action. The afferent stimulus is corneal drying stimulating CN V, ophthalmic branch to the brainstem and the efferent fibres travel in CN VII to the eyelids
| Testing by observation | CNN being evaluated |
|---|---|
| Watch as the animal interacts with its environment | Many |
| Head position – tilted, the eyes are in a different plane compared with lateral rotation (torticollis) in which the eyes are in the same plane | Tilt – CN VIII (a), Vestibular |
| (Torticollis may be due to cervical or forebrain lesions) | |
| Facial symmetry, blinking, nostril and ear movement | CN VII |
| Blinking – due to stimulus of corneal drying | Ophthalmic branch of CN V (a), blinking due to CN VII (e) |
| Pupil size | Parasympathetic CN III (e) for miosis, or sympathetic (e) for mydriasis |
| Eyeball position | CNN II or VIII (a), CNN III, IV, VI (e) |
| Olfaction, vision, hearing, | CN I, II, VIII (a) |
| Masticatory muscle bulk, chewing | CN V (e) |
| Tongue movement, e.g. licking lips or nose | CN V (a) maxillary branch |
| CN XII (e) | |
| Swallowing | CN IX, X (a) and (e) |
| Laryngeal noise – phonation and stridor | CN X, XI (e) |
The dog’s neurological deficits were readily detectable by observation. Clinically, the dog’s gait was ataxic (incoordinated) and paretic. It had marked atrophy of specific shoulder muscles, especially the supraspinatus muscle. In this particular case it was due to hypertrophied ligamentous tissue in the spinal canal compressing primarily the C6 spinal cord segment. The C6 spinal nerve arising from this segment is a key component of the suprascapular nerve innervating the supraspinatus muscle. LMNs supplying the suprascapular nerve and innervating the supraspinatus muscle (see Fig. 4.7). Functionally, loss of supraspinatus muscle function compromises shoulder extension resulting in hypometria (shortened strides) in the thoracic limbs. It also compressed sensory tracts and UMN tracts passing through the region supplying both the thoracic and pelvic limbs (see Fig. 4.8). Clinically the dog’s pelvic limb gait was ataxic (incoordinated – ‘wobbly’) and paretic, while the thoracic limb gait was short and stiff. This case was an example of ‘Wobbler syndrome’ (see Fig. 6.3).
Hands-on testing
Paw position response (knuckling)
This test is more specific than hopping for evaluating tactile receptors compared with muscle receptors, thus it is good for conscious proprioceptive testing. The animal’s weight is gently pushed to the opposite side, reducing the amount being carried on the leg being tested, then the toes are flipped under (Fig. 13.5). To test for subtle dysfunction, the clinician may just turn under a single toe. The body weight is redistributed back over the limb being tested and the animal is observed to see if it corrects the foot position. To avoid stimulating joint angle and muscle receptors in the proximal leg, the clinician tries to turn the toes under without lifting the leg.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree