Chapter 12 The autonomic nervous system
Key points
 The ANS is an involuntary system that preserves a constant internal environment by innervating cardiac muscle, and smooth muscle of blood vessels and visceral structures.
The ANS is an involuntary system that preserves a constant internal environment by innervating cardiac muscle, and smooth muscle of blood vessels and visceral structures.
 The system has afferent, central and efferent components.
The system has afferent, central and efferent components.
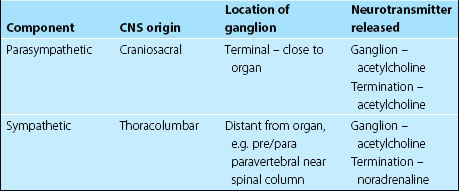
 It is subdivided into the craniosacral, parasympathetic (‘rest and digest’), and the thoracolumbar, sympathetic (‘fight or flight’) systems.
It is subdivided into the craniosacral, parasympathetic (‘rest and digest’), and the thoracolumbar, sympathetic (‘fight or flight’) systems.
 Autonomic UMN cell bodies are located in the hypothalamus.
Autonomic UMN cell bodies are located in the hypothalamus.
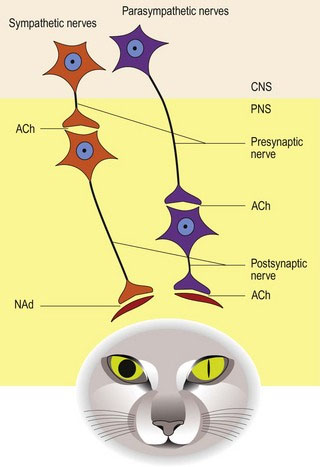
 A presynaptic and a postsynaptic neuron, in series, connect the CNS with the target organ. The presynaptic neuron has its cell body in the CNS and synapses with the postsynaptic neuron in a peripheral ganglion.
A presynaptic and a postsynaptic neuron, in series, connect the CNS with the target organ. The presynaptic neuron has its cell body in the CNS and synapses with the postsynaptic neuron in a peripheral ganglion.
 The neurotransmitter at the autonomic ganglia is acetylcholine. The neurotransmitter at the neuromuscular junction is acetylcholine for the parasympathetic system and noradrenaline for the sympathetic nervous system.
The neurotransmitter at the autonomic ganglia is acetylcholine. The neurotransmitter at the neuromuscular junction is acetylcholine for the parasympathetic system and noradrenaline for the sympathetic nervous system.
 The location of the second neuron is system specific and close to the organ (terminal/intramural) for the parasympathetic system. It is remote from the organ (pre- or paravertebral) for the sympathetic nervous system.
The location of the second neuron is system specific and close to the organ (terminal/intramural) for the parasympathetic system. It is remote from the organ (pre- or paravertebral) for the sympathetic nervous system.
 The presynaptic nerve can pass through a number of ganglia before synapsing, so the terms ‘preganglionic’ and ‘postganglionic’ can be misleading. Presynaptic and postsynaptic neurons are the preferred terms.
The presynaptic nerve can pass through a number of ganglia before synapsing, so the terms ‘preganglionic’ and ‘postganglionic’ can be misleading. Presynaptic and postsynaptic neurons are the preferred terms.
The ANS is a diffuse system that innervates visceral structures, glandular myoepithelium, fat and vasculature throughout the body. The system has afferent, central and efferent components. Afferent fibres often use the same pathways as the efferent nerves. Afferent visceral fibres may also travel via somatic spinal nerves to reach the CNS (see also Chapter 1, p4 for introduction to the ANS).
Subdivisions
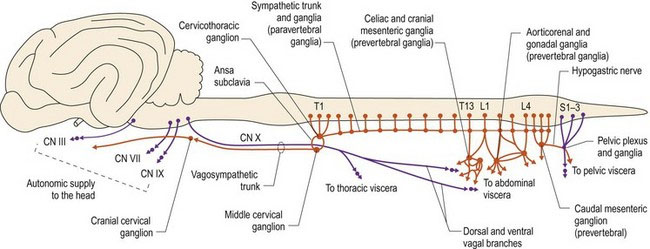
Anatomically, the two systems arise from different areas of the CNS, with the parasympathetic system arising from the brain and sacral spinal cord, and the sympathetic system from the thoracolumbar spinal cord. Hence, they are also known as the craniosacral and thoracolumbar systems, respectively (Fig. 12.1).
ANS: Central components and peripheral components
Two-neuron system in the periphery
For sympathetic fibres, the ganglion is remote from the organ being innervated. These ganglia are located ventral, or near to the vertebral column in a prevertebral or paravertebral position, respectively. Thus, the sympathetic system has a shorter presynaptic neuron and longer postsynaptic neuron (Fig. 12.2).
A summary of the key anatomical features of each system is given in Table 12.1.
Visceral afferent system
Key points
 Visceral receptors are stimulated by pressure, stretch and chemical changes.
Visceral receptors are stimulated by pressure, stretch and chemical changes.
 Input to the CNS is via cranial nerves (CNN VII, IX, X) and peripheral branches of autonomic and spinal nerves. Input stimulates reflex activity and conscious perception.
Input to the CNS is via cranial nerves (CNN VII, IX, X) and peripheral branches of autonomic and spinal nerves. Input stimulates reflex activity and conscious perception.
 The solitary tract and its nucleus in the medulla oblongata receives input from cranial nerves and makes connections with the reticular formation for reflex function.
The solitary tract and its nucleus in the medulla oblongata receives input from cranial nerves and makes connections with the reticular formation for reflex function.
Sympathetic/thoracolumbar division
Key points
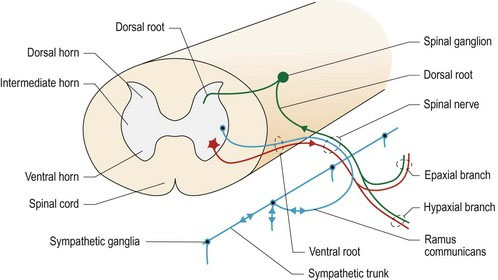
 The sympathetic nervous system originates from the lateral/intermediate horn of the thoracolumbar spinal cord.
The sympathetic nervous system originates from the lateral/intermediate horn of the thoracolumbar spinal cord.
 Peripheral ganglia are located in the paired, paravertebral sympathetic trunks, or the median, prevertebral ganglia in the dorsal aspect of the thoracic and abdominal cavities.
Peripheral ganglia are located in the paired, paravertebral sympathetic trunks, or the median, prevertebral ganglia in the dorsal aspect of the thoracic and abdominal cavities.
 Postsynaptic neurons travel via spinal nerves, or specific named nerves, to their target organ.
Postsynaptic neurons travel via spinal nerves, or specific named nerves, to their target organ.
 Visceral structures in the head are supplied by postsynaptic neurons originating in the cranial cervical ganglion.
Visceral structures in the head are supplied by postsynaptic neurons originating in the cranial cervical ganglion.
 The thoracic viscera are innervated by neurons primarily originating in the cervicothoracic and middle cervical ganglion.
The thoracic viscera are innervated by neurons primarily originating in the cervicothoracic and middle cervical ganglion.
 The abdominal and pelvic regions are supplied by branches from the thoracic and abdominal sympathetic trunks, and prevertebral ganglia located around the aorta.
The abdominal and pelvic regions are supplied by branches from the thoracic and abdominal sympathetic trunks, and prevertebral ganglia located around the aorta.
Presynaptic fibres originate in the intermediate (lateral) horn of the thoracolumbar spinal cord. Fibres may leave in the ventral root from their spinal cord segment of origin, or they may pass cranially, or caudally, a number of segments within the spinal cord before exiting it. The fibres exit the spinal cord along with the somatic motor neurons using the ventral roots of C8–L4/5 (up to L7) spinal nerves. The ventral roots fuse with the dorsal roots to form proper spinal nerve at the level of the intervertebral foramen (see Fig. 1.1). Lateral to the foramen, the proper spinal nerve splits into epaxial, hypaxial and ventral branches. The ventral branch forms the ramus communicans (ramus – L = branch). The ramus communicans conveys sympathetic efferent and visceral afferent fibres, between the spinal cord and the bilateral, sympathetic trunks that run ventrolaterally on both sides of the vertebral column (Fig. 12.3). The ramus communicans conveys both presynaptic (myelinated) sympathetic efferent fibres that are travelling to the trunk, and postsynaptic (unmyelinated) fibres that return from the trunk to rejoin the spinal nerves. This gives rise to the names of white and grey ramus communicans, respectively. These paravertebral ganglia and trunks are prominent in the thoracic region and extend into the lumbar region (see Fig. 12.4). In the caudal lumbar area, the trunks may fuse and continue caudally, ventral to the sacral and caudal vertebrae. In the abdominal region, nerves leave the paravertebral sympathetic trunks and connect to prevertebral ganglia located ventral to the vertebral column near the large abdominal arteries. Cranially, the sympathetic fibres continue into the cervical region, in conjunction with the vagus nerve forming the vagosympathetic trunk; this is located in the carotid sheath.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree