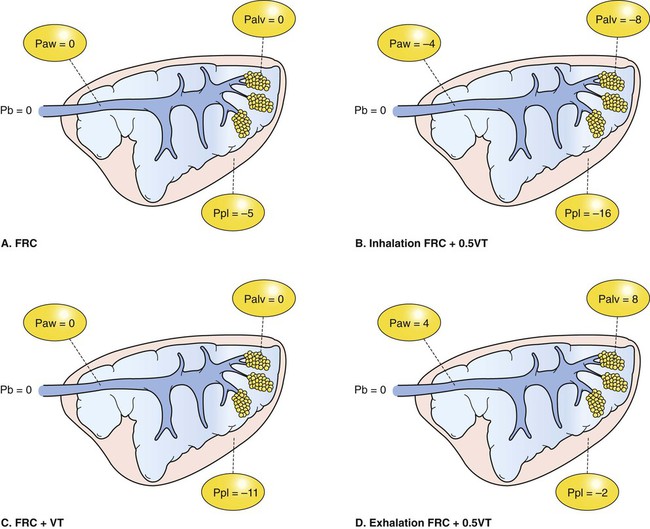
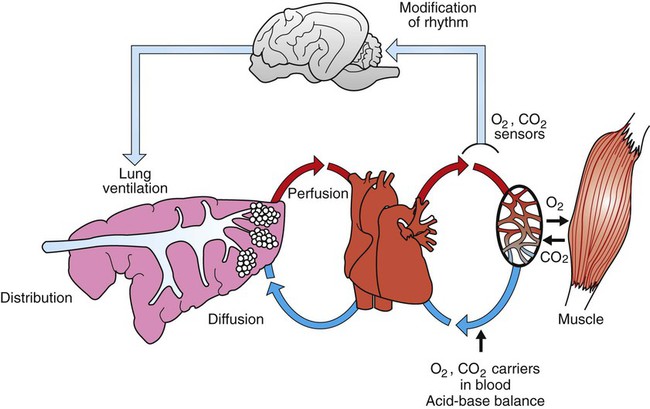
1. The respiratory system’s primary function is the transport of oxygen and carbon dioxide between the environment and the tissues. 1. Ventilation is the movement of gas into and out of the lung. 2. Ventilation requires muscular energy. 3. The respiratory muscles generate work to stretch the lung and overcome the frictional resistance to airflow provided by the airways (airway resistance). 4. Lung elasticity results from tissue and surface tension forces. 5. The lung is mechanically connected to the thoracic cage by the pleural liquid. 6. Airflow is opposed by frictional resistance in the airways. 7. Smooth muscle contraction affects the diameters of the trachea, bronchi, and bronchioles. 8. Dynamic compression can narrow the airways and limit airflow. 9. The distribution of air depends on the local mechanical properties of the lung. 10. In some species, air travels between adjacent regions of lung through collateral pathways. Gas exchange requirements vary with metabolism and may increase up to 30 times during strenuous exercise (Figure 45-1). Surprisingly, these variations are normally accomplished with only a small energy cost. In animals with respiratory disease, the energy cost of breathing can increase. This results in less energy available for exercise or weight gain, and the owner notices the animal’s poor performance. The respiratory system also is involved in communication by sound and pheromones and is important in thermoregulation; metabolism of endogenous and exogenous substances; and protection of the animal against inhaled dusts, toxic gases, and infectious agents. Additionally, the increase in abdominal pressure that facilitates urination, defecation, and parturition requires active participation of the respiratory muscles. Figure 45-2 shows the processes involved in gas exchange, including ventilation; distribution of gas within the lung; diffusion at the alveolocapillary membrane; transport of O2 in the blood from the lungs to the tissue capillaries and of CO2 in the reverse direction; and diffusion of gases between blood and tissues. Air flows into the alveoli through the nares, nasal cavity, pharynx, larynx, trachea, bronchi, and bronchioles. These structures constitute the conducting airways. Because gas exchange does not occur in these pathways, they are also known as the anatomic dead-space (Figure 45-3). Dead-space can also occur within the alveoli. This alveolar dead-space is caused by alveoli that are poorly perfused with blood, so that gas exchange cannot occur optimally (see Chapter 47). Physiologic dead-space is the sum of the anatomic and the alveolar dead-space. Let us define the portion of each VT that enters the alveoli as VA and the part that enters the dead-space as VD. Then: If each side of this equation is multiplied by respiratory frequency (f) as follows: During exercise, respiratory muscle activity increases in order to generate the increase in At the end of a normal exhalation, some air (~45 mL/kg) remains in the lung. This air volume is known as functional residual capacity (FRC). At FRC, the pressure in the pleural cavity (Ppl) that surrounds the lung is approximately 5 cm H2O below atmospheric pressure (−5 cm H2O). During inhalation, as the inspiratory muscles contract, the thorax enlarges and Ppl decreases. This decrease in Ppl stretches the elastic lung and enlarges its volume, which decreases pressure within the alveoli (Palv). The decrease in Palv causes air to flow into the lung through the tracheobronchial tree (Figure 45-5). Lung compliance is a measure of the elastic properties of the lungs, and airway resistance is a measure of the frictional resistance of the airways. The magnitude of the change in pleural pressure (ΔPpl) during each breath is determined by the tidal volume (VT), by lung compliance (C), by airflow rate (
Overview of Respiratory Function
Ventilation of the Lung
Respiratory Function
The Respiratory System’s Primary Function Is the Transport of Oxygen and Carbon Dioxide Between the Environment and the Tissues
Ventilation
Ventilation Is the Movement of Gas Into and Out of the Lung
Ventilation Requires Muscular Energy
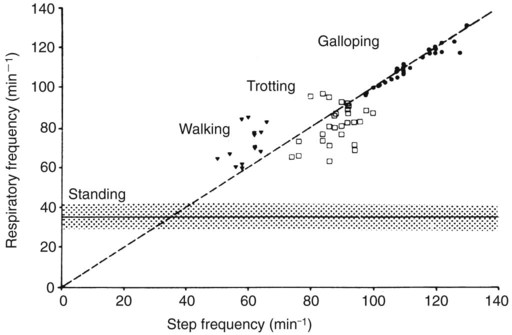
 . In cursorial (running) mammals, ventilation is synchronized with gait in the canter and gallop, but not in the walk or trot (Figure 45-4). Inhalation occurs as the forelimbs are extended and the hind limbs are accelerating the animal forward. Exhalation occurs when the forelimbs are in contact with the ground. In the galloping horse and perhaps in other galloping quadrupeds, much of the increase in size of the thorax during inhalation is a consequence of elongation of the trunk as the spine extends rather than an increase in the diameter of the thorax.
. In cursorial (running) mammals, ventilation is synchronized with gait in the canter and gallop, but not in the walk or trot (Figure 45-4). Inhalation occurs as the forelimbs are extended and the hind limbs are accelerating the animal forward. Exhalation occurs when the forelimbs are in contact with the ground. In the galloping horse and perhaps in other galloping quadrupeds, much of the increase in size of the thorax during inhalation is a consequence of elongation of the trunk as the spine extends rather than an increase in the diameter of the thorax.
The Respiratory Muscles Generate Work to Stretch the Lung and Overcome the Frictional Resistance to Airflow Provided by the Airways (Airway Resistance)
 ), and by airway resistance (R), as follows:
), and by airway resistance (R), as follows:
< div class='tao-gold-member'>
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Overview of Respiratory Function: Ventilation of the Lung
Only gold members can continue reading. Log In or Register to continue
 ) is directly related to the total mass of mitochondria within the skeletal muscles. Athletic species such as the horse and dog have greater mitochondrial density and therefore greater
) is directly related to the total mass of mitochondria within the skeletal muscles. Athletic species such as the horse and dog have greater mitochondrial density and therefore greater  than do less athletic species of similar body size such as the cow and goat.
than do less athletic species of similar body size such as the cow and goat.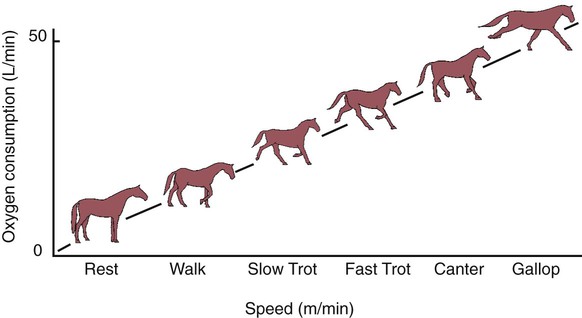
 ), is determined by the volume of each breath, known as the tidal volume (VT), and the number of breaths per minute, known as respiratory frequency (f), as clarified next from the following equation:
), is determined by the volume of each breath, known as the tidal volume (VT), and the number of breaths per minute, known as respiratory frequency (f), as clarified next from the following equation:
 , which must occur when an increase in metabolic rate demands more oxygen, can be brought about through an increase in VT, f, or both.
, which must occur when an increase in metabolic rate demands more oxygen, can be brought about through an increase in VT, f, or both.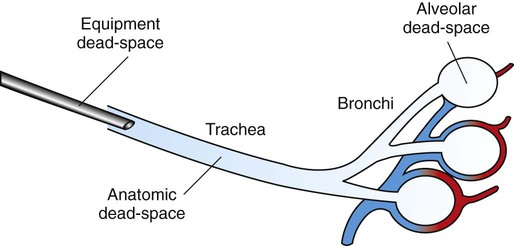
 ) ratio)], some of the air entering that alveolus is not involved in gas exchange and contributes to dead-space.
) ratio)], some of the air entering that alveolus is not involved in gas exchange and contributes to dead-space.

 ) is the sum of alveolar ventilation (
) is the sum of alveolar ventilation ( ), which is essential for gas exchange, and dead-space ventilation (
), which is essential for gas exchange, and dead-space ventilation ( ), which is wasted ventilation.
), which is wasted ventilation.