Drugs Used in Skin Disorders
Learning Objectives
After studying this chapter, you should be able to
1. Exhibit a basic understanding of the anatomy and physiology of the skin.
2. List the common ingredients of topical antiseborrheics.
3. Describe the use of topical antipruritics.
4. Explain the use of fatty acid supplements.
5. Explain the use of astringents.
6. Explain the use of skin antiseptics.
Key Terms
Antiseptic
Astringent
Collagen
Comedo (pl. comedones)
Dermatitis
Dermatophyte
Dermatophytosis
Erythema
Fatty acid
Furuncle (furunculosis)
Granulation tissue
Integumentary system
Keratolytic
Keratoplastic
Pruritus
Pseudomembranous colitis
Pyoderma
Seborrhea
Seborrhea oleosa
Seborrhea sicca
Introduction
Dermatologic conditions are frequently seen in veterinary practice. From ectoparasitic problems to allergies, veterinarians are continually combating companion animal skin problems. As a veterinary technician, this is one area in which your expertise will be used because clients will ask many questions about shampoos, dips, conditioners, soaks, lotions, creams, ointments, sprays, powders, and topical products designed to have activity against fleas, ticks, and mosquitoes. Each of these products may be used to treat a full spectrum of dermatologic problems from parasites to pyoderma. Patients are often presented for examination of a skin disease when in reality they have an underlying systemic illness. Veterinarians use various diagnostic procedures (e.g., skin scrapings, allergy testing, and dermatophyte tests) to determine the cause of skin disease. Technicians play a vital role by obtaining a complete history, knowing how to perform the diagnostic procedures used in a dermatologic workup, and providing client education. Client education is essential when skin disease is treated because clients must understand the purpose of medications and how they should be properly used.
Anatomy and Physiology
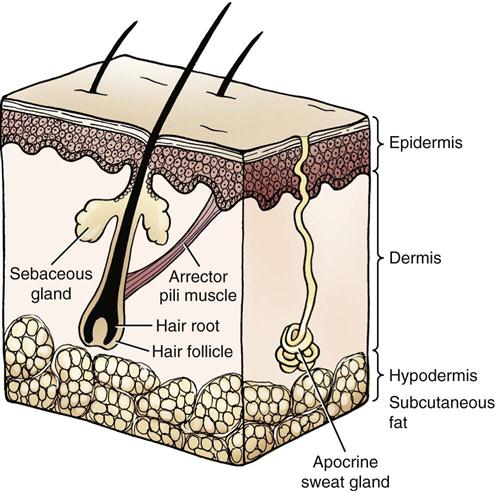
The skin is a part of the integumentary system and constitutes the largest organ in the body. It is made up of three layers (Figure 11-1) and serves multiple functions. It provides a barrier against the outside world by preventing entry of pathogenic microorganisms and by protecting against physical and chemical insults. It senses heat, cold, pain, touch, pressure, and other sensations like pruritus and helps to regulate body temperature through mechanisms related to cutaneous blood flow, sweating, and the haircoat. The skin plays a role in immunologic defense through the actions of Langerhans (dendritic or antigen-presenting) cells and keratinocytes, produces vitamin D3 from precursors in the skin, and acts as a reservoir for electrolytes and other substances. This organ may also play a limited role in the excretion of some substances from the body (Table 11-1).
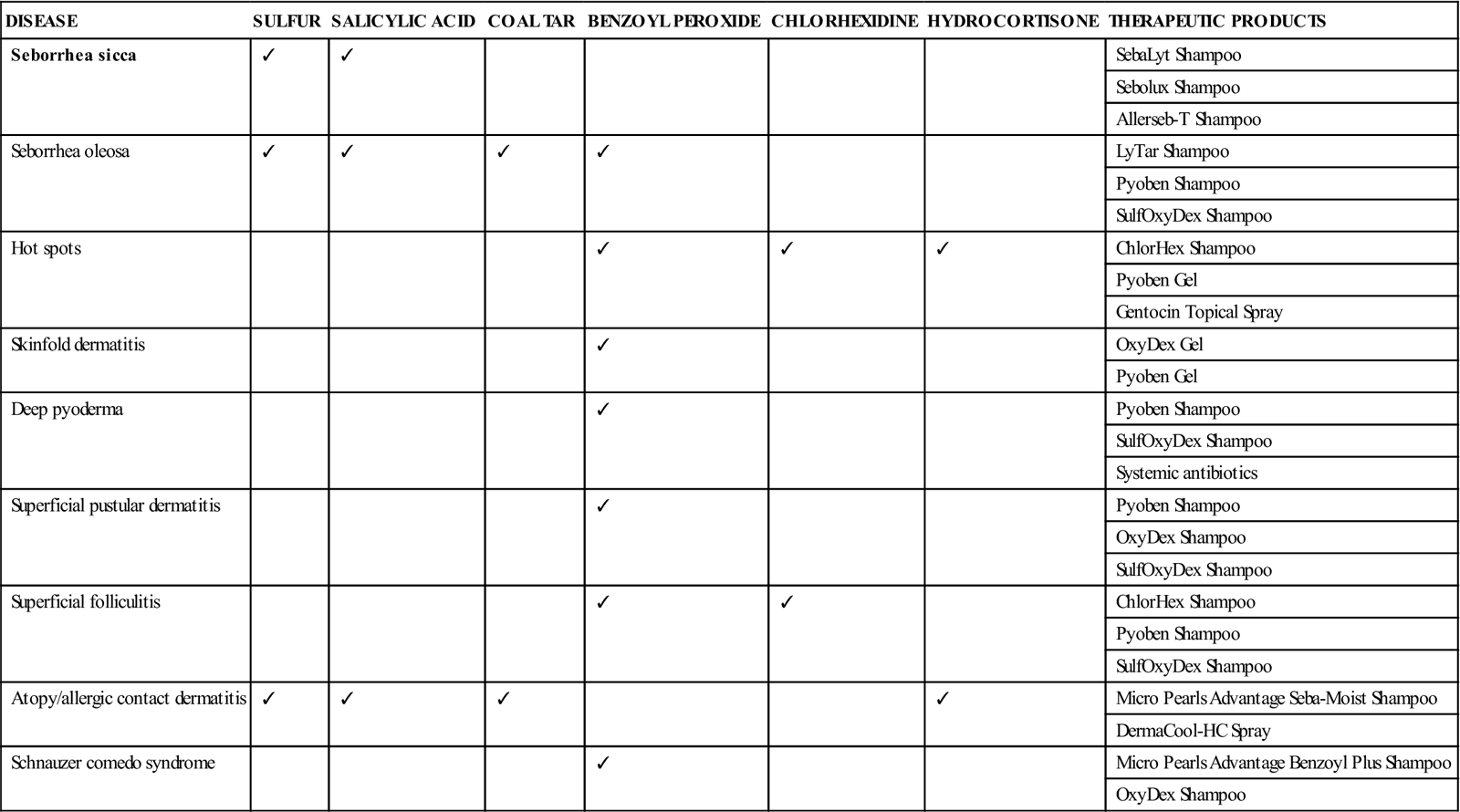
TABLE 11-1
Common Skin Disorders With Suggested Treatments and Various Products Available
| DISEASE | SULFUR | SALICYLIC ACID | COAL TAR | BENZOYL PEROXIDE | CHLORHEXIDINE | HYDROCORTISONE | THERAPEUTIC PRODUCTS |
| Seborrhea sicca | ✓ | ✓ | SebaLyt Shampoo | ||||
| Sebolux Shampoo | |||||||
| Allerseb-T Shampoo | |||||||
| Seborrhea oleosa | ✓ | ✓ | ✓ | ✓ | LyTar Shampoo | ||
| Pyoben Shampoo | |||||||
| SulfOxyDex Shampoo | |||||||
| Hot spots | ✓ | ✓ | ✓ | ChlorHex Shampoo | |||
| Pyoben Gel | |||||||
| Gentocin Topical Spray | |||||||
| Skinfold dermatitis | ✓ | OxyDex Gel | |||||
| Pyoben Gel | |||||||
| Deep pyoderma | ✓ | Pyoben Shampoo | |||||
| SulfOxyDex Shampoo | |||||||
| Systemic antibiotics | |||||||
| Superficial pustular dermatitis | ✓ | Pyoben Shampoo | |||||
| OxyDex Shampoo | |||||||
| SulfOxyDex Shampoo | |||||||
| Superficial folliculitis | ✓ | ✓ | ChlorHex Shampoo | ||||
| Pyoben Shampoo | |||||||
| SulfOxyDex Shampoo | |||||||
| Atopy/allergic contact dermatitis | ✓ | ✓ | ✓ | ✓ | Micro Pearls Advantage Seba-Moist Shampoo | ||
| DermaCool-HC Spray | |||||||
| Schnauzer comedo syndrome | ✓ | Micro Pearls Advantage Benzoyl Plus Shampoo | |||||
| OxyDex Shampoo |
The three primary layers of the skin are the epidermis, the dermis or corium, and the hypodermis or subcutis (also called the panniculus). The dermis provides most of the thickness of the skin. The epidermis comprises five distinct layers. These layers are the basal (deepest), spinous, granular, clear, and horny/cornified (superficial) layers. Epidermal cells are replenished in the basal layer and are pushed outward by newly forming layers. As these cells reach the surface, they are flattened and hardened to form a protective barrier. It normally takes 21 to 22 days for cells to reach the outer layer; this process is called the epidermal turnover rate. The epidermal turnover rate may be sped up in some disease processes. Continual shedding of these cells is called desquamation. When the process becomes excessive, scale or dandruff is seen. The epidermis includes a population of normal microorganisms that help to prevent overgrowth of pathogenic microorganisms.
The dermis or corium is located directly beneath the epidermis and is separated from and attached to it by the basement membrane. The dermis is a thick layer that comprises collagen fibers, blood vessels, nerves, lymphatics, and other structures such as hair follicles, sebaceous glands, and sweat glands. Sebaceous glands are found throughout haired skin, and their ducts empty into hair shafts. One type of sweat gland (eccrine) is found only in footpads and may play a role in body temperature regulation. The dermis gives stability and flexibility to the skin and acts to maintain and repair the skin.
The hypodermis is the deepest layer of the skin. It is made up of fat and connective tissue. Its functions are to provide padding and insulation and to serve as an energy store.
The skin produces hair and other keratinized structures like nail, horn, nasal pads, and footpads. Hair grows from follicles found in the dermis. In contrast to humans, who have one hair per follicle, dogs and cats have multiple hairs per follicle. Individual hair follicles have associated glandular structures (see earlier) and arrector pili muscles that are responsible for piloerection (hair standing on end). The hair follicle is frequently involved in bacterial, fungal, and demodectic infections. If a hair follicle loses the hair and becomes plugged with sebaceous secretions and keratin, a comedo (blackhead) results. There are three stages or phases of hair growth called anagen (growth), telogen (rest), and catagen (intermediate). Hair grows until it reaches a predetermined length, enters a resting phase, and then is shed. The hair cycle is controlled by day–night length (photoperiod), environmental temperature, hormones, and nutritional status. General illness, skin disorders, poor nutrition, overbathing, and stress are conditions that may result in excessive shedding.
Wound Healing
A wound is created when an insult—either purposeful, such as surgery, or incidental, such as trauma—disrupts the normal integrity of the tissue (McCurnin and Bassert, 2006).
However, more than one phase of wound healing usually is occurring at any time (McCurnin and Bassert, 2006). The inflammatory phase usually begins with hemorrhage and is limited by vessel contraction and constriction. Serum leakage into the wound deposits fibrinogen and other clotting elements. Later, this serum provides enzymes, proteins, antibodies, and complement. The débridement phase begins about 6 hours after injury and is facilitated by the appearance of neutrophils and monocytes that migrate to the wound. Neutrophils phagocytize bacteria and then die. Monocytes become macrophages and phagocytize necrotic debris. The repair phase is marked by the formation of a blood clot and is usually active by 3 to 5 days post injury. During the repair phase, fibroblasts produce collagen and other connective tissue proteins. Capillaries infiltrate the wound to provide blood supply and oxygen. This process forms granulation tissue. Epithelial cells proliferate beneath the scab, and the wound begins to contract. The maturation phase is the end of wound healing and is a period of remodeling. During this time, the wound consolidates and strengthens. Many factors contribute to proper wound healing. These include patient factors (e.g., the age of the patient, nutritional status, rest, environment, and general health); wound factors, including wound characteristics (i.e., contaminated wounds versus noncontaminated wounds); external factors (e.g., temperature regulation [i.e., bandage]); whether lavage is performed; and how the wound is closed (e.g., primary or secondary closure). A veterinarian must consider all these factors when determining how to treat a wound and when anticipating how well it will heal.
 Topical Antipruritics and Antiinflammatories
Topical Antipruritics and Antiinflammatories
Noncorticosteroids
Aluminum Acetate Solution
This is also known as Burow’s solution.
Clinical Uses
This is an astringent solution and an antipruritic agent that is useful for the treatment of superficial skin problems. It can be used to help with acute moist dermatitis, fold dermatitis, and contact dermatitis. Some doctors may use it to treat otitis externa. The exact manner in which this agent works is not fully known at this time.
Dosage Forms
Adverse Side Effects
Do not use anything that prevents the evaporation of this solution from the skin. Avoid contact with the eyes. Clients should wash their hands after administration and should wear gloves when applying the solution.
Colloidal Oatmeal
Clinical Uses
Colloidal oatmeal has unique properties in that it can be used topically as both an antiinflammatory and antipruritic agent. At this time, however, scientists are concerned about its mechanism of action. It is thought that perhaps it inhibits prostaglandin production.
Dosage Forms
Adverse Side Effects
Colloidal oatmeal is very safe.
Topical Essential Fatty Acids
Clinical Uses
These products are commonly used for their antipruritic and antiinflammatory properties. They tend to help skin problems such as atopic dermatitis, sebaceous adenitis, and seborrhea. Some of these products have natural oils in them, which also may help skin problems. Essential fatty acids affect arachidonic acid levels and also affect the production of prostaglandins in the body, which can reduce inflammation and pruritus. Essential oils also help to create healthy skin.
Dosage Forms
Adverse Side Effects
These are uncommon.
Topical Diphenhydramine HCl
Clinical Uses
Diphenhydramine is a first-generation antihistamine that has some local anesthetic properties. This drug can be absorbed transdermally but not enough to cause systemic effects.
Dosage Forms
Most products are human label; the exception is ResiHist Leave-On Lotion.
Adverse Side Effects
Avoid contact with eyes or mucous membranes. Diphenhydramine should not be applied to skin that is oozing. Client should wear gloves when applying.
Topical Lidocaine and Lidocaine/Prilocaine
Clinical Uses
This product can be applied topically as a skin anesthetic and also helps with pruritus. It may be used to treat acute moist dermatitis, pruritic lesions, or painful skin conditions.
Dosage Forms
Adverse Side Effects
Avoid contact with the eyes and do not use in ears. Clients should wear gloves when applying these products.
Phytosphingosine
Clinical Uses
Phytosphingosine is useful in treating localized inflammatory and pruritic cases such as atopic dermatitis. It can also be sprayed on sutures postoperatively to aid in the wound healing process.
Dosage Forms
Adverse Side Effects
This product may cause skin redness or irritation.
Pramoxine HCl
Clinical Uses
This agent has the ability to cause surface and local anesthetic characteristics, which can affect the peripheral nerves. It may be combined with other products to reduce pain or itching. At this time, scientists are unclear of this drug’s mechanism of action.
Dosage Forms
The following are all veterinary-label products.
• Micro Pearls Advantage Dermal-Soothe Anti-Itch Spray
• Micro Pearls Advantage Dermal-Soothe Anti-Itch Shampoo
• Micro Pearls Advantage Dermal-Soothe Anti-Itch Cream Rinse
• Pramoxine Anti-Itch Cream Rinse
The following are all human-label pramoxine HCl products.
Adverse Side Effects
Avoid contact with the eyes. This agent is not for ophthalmic use. Clients should wear gloves before applying these products to their pets’ bodies.
Phenol/Menthol/Camphor
Clinical Uses
These agents are used in equines for overexertion, soreness, or stiffness.
Dosage Forms
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree