CHAPTER one The Radiograph
Competent radiologic practice presupposes the availability of good-quality radiographs. Familiarity with the basic principles underlying the production of radiographs is a prerequisite for the radiologist. Accurate positioning of the animal under investigation, correct exposure factors, the use of grids and other ancillary aids, and good processing technique all influence the quality of a radiograph. The use of a technique chart is essential for consistent results. Consistency is important, particularly when studies have to be repeated over time to assess the progress of a particular case. If the radiographs in such studies are not comparable, errors of interpretation are likely to occur. Radiographs may be of poor quality because of improper positioning, improper exposure technique, or poor darkroom technique. It is hazardous to attempt to interpret such radiographs.
A radiograph is a composite shadow of structures and objects in the path of an x-ray beam recorded on film. Because a radiograph is, in essence, a shadowgraph, the geometric rules applicable to the formation of shadows are also valid for radiographs. Thus, the nearer the object under examination is to the film, the sharper will be its outline. Distance of an object from the film causes magnification of the resulting shadow and some distortion and blurring. The nearer the object is to the source of radiation, the greater will be the degree of magnification. The area being studied, therefore, should be placed as near to the film as possible and at a standard acceptable distance from the source of radiation, usually 100 cm (36 to 40 inches). Because the radiograph (being a shadowgraph) outlines an object in only two planes, at least two views, made at right angles to one another (orthogonal views), are required to demonstrate the object in a three-dimensional representation. Shadows are cast not only of the outline of the body, but also of structures within it (Figure 1-1).
DENSITY AND OPACITY
A radiograph is an image made up of shadows of different opacities. Subject density is the weight per given volume of a body tissue or other object. Bone is more dense than muscle, and muscle is more dense than fat. The denser an object is, the more it inhibits the passage of radiation. Radiographic opacity is a measure of the capacity of a tissue or structure to block x-rays. Where x-rays readily reach the film, the film appears black after processing. If the x-rays are prevented from reaching part of the film, the unaffected area will appear white on the processed film. Between these two extremes, various combinations of light, dark, and gray areas are produced. Radiographic opacity therefore depends on subject density; the greater the subject density, the less radiation reaches the film.
Five radiographic opacities can be recognized:
Bone is not as dense as a metallic substance. It allows little radiation to pass through it compared with other body tissues. Areas of film that have been covered by bone appear almost white on a radiograph.
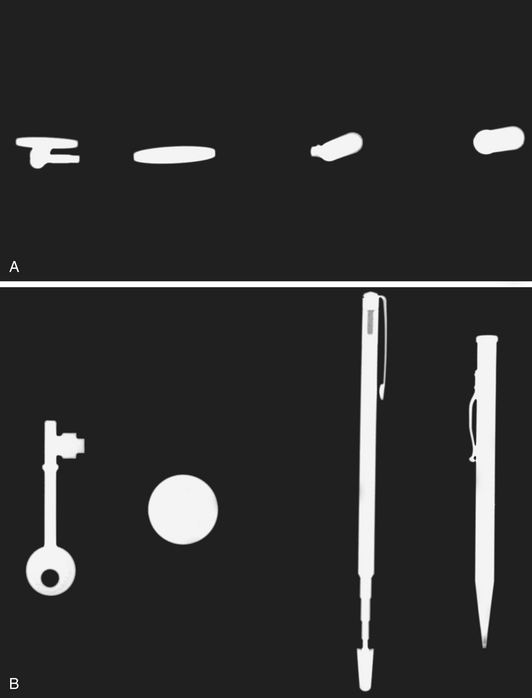
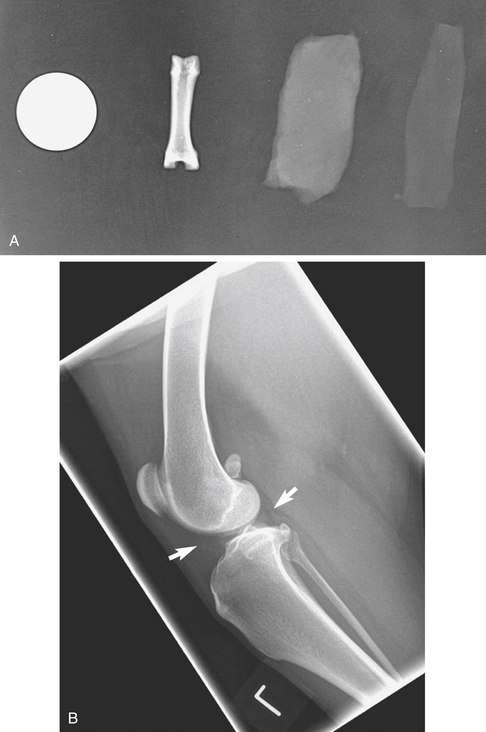
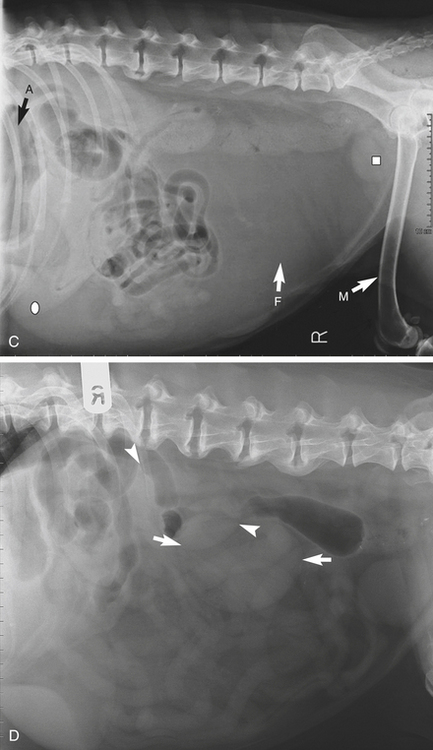
Bone, fluid, fat, and gas occur normally within the body and are said to have biologic densities. Metallic densities are introduced into the body as contrast media (explained later in this chapter), surgical implants, or foreign bodies (Figure 1-2, A to C).
FACTORS AFFECTING IMAGE QUALITY
Many factors can affect the quality of a radiographic image:
STANDARD VIEWS
Agreed terms are used to describe the standard projections. The terminology used in this book is that suggested by the Nomenclature Committee of the American College of Veterinary Radiology. The committee recommended that veterinary anatomic directional terms should be those listed in the Nomina Anatomica Veterinaria. Radiographic projections are described by the direction in which the central ray of the primary beam penetrates the body part of interest—from the point of entrance to the point of exit. The subject area of interest should be as close to the film or detector as possible. Structures within the body that are further away from the film are magnified (Figure 1-2, D).
Definitions
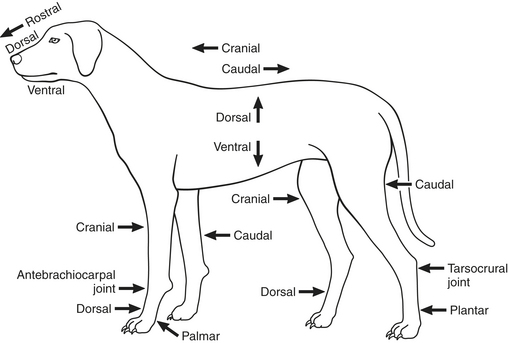
The meanings to be ascribed to the different directional terms are as discussed in the following sections (Figure 1-3).
TECHNIQUE
Standard views are views taken at right angles to one another and usually are made in the routine examination of a part of the body. The most common are the dorsoventral, ventrodorsal, lateral, mediolateral, craniocaudal, dorsopalmar, and dorsoplantar. An oblique view is made at an angle somewhere between the standard views. In the case of oblique views, in addition to stating the anatomic points of entry and exit of the x-ray beam, the angle of obliquity may be given. This information enables studies to be repeated with accuracy. Thus L50D-RVO is read as left 50 degrees dorsal-right ventral oblique. It means that an oblique study was made with the beam entering the body on the left side dorsally at an angle of 50 degrees toward the back and exiting on the right side ventrally. Lesion-oriented studies are sometimes used with tangential (skyline) or nonstandard views. A lesion-oriented oblique view is one that profiles a lesion.
Abbreviations
Common radiographic abbreviations include those listed in Box 1-1.
Box 1-1. Common Radiographic Abbreviations
| Le | Left |
| Rt | Right |
| D | Dorsal |
| V | Ventral |
| C | Cranial |
| Cd | Caudal |
| R | Rostral |
| RLR | Right lateral recumbent |
| LLR | Left lateral recumbent |
| M | Medial |
| L | Lateral |
| Pr | Proximal |
| Di | Distal |
| Pa | Palmar |
| Pl | Plantar |
| O | Oblique |
CONTRAST MEDIA
A filling defect is a space-occupying mass within a hollow organ (see Chapter 2, p.154). Contrast medium fails to fill the organ fully at the site of the mass (defect). A plain radiograph is one made without any contrast agent.
VIEWING THE RADIOGRAPH
Systematic Approach
Some radiologists prefer to examine radiographs “cold,” that is, without any knowledge of the clinical picture. After a preliminary examination, the radiograph is then evaluated in the light of the clinical and other findings. Preconceived notions about a case may militate against an objective assessment of a radiograph.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree