CHAPTER four Bones and Joints
BONES
Bone lends itself readily to radiographic examination. Being composed primarily of calcium and phosphorus, it is relatively dense and its radiographic opacity contrasts well with surrounding tissues. As living tissue, it frequently reflects changes in general metabolism, although changes may take time to develop.
Development
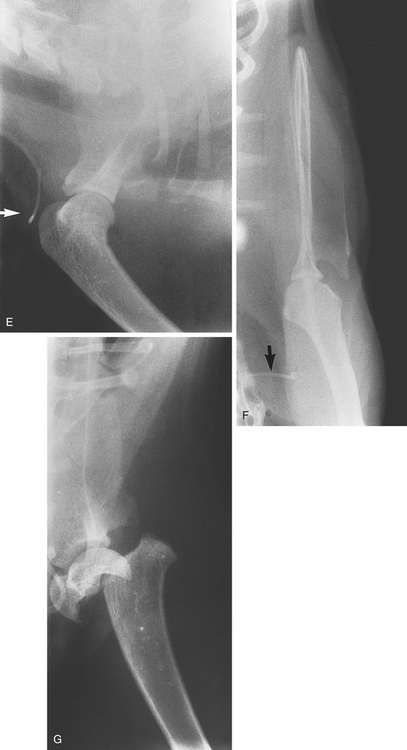
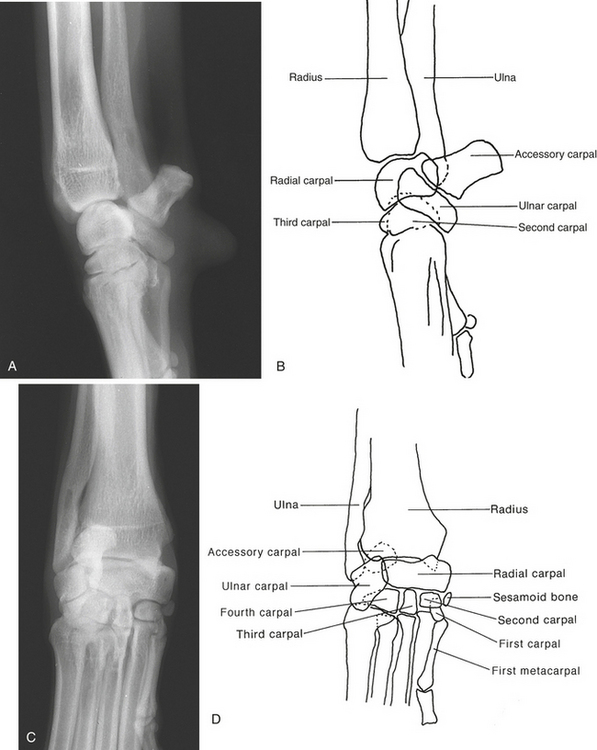
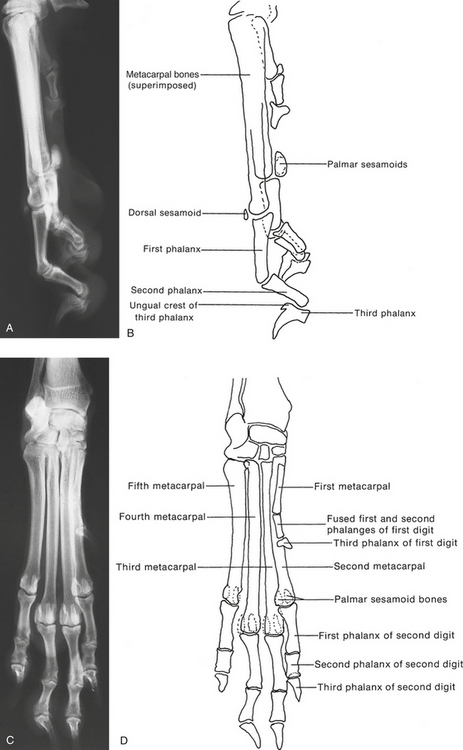
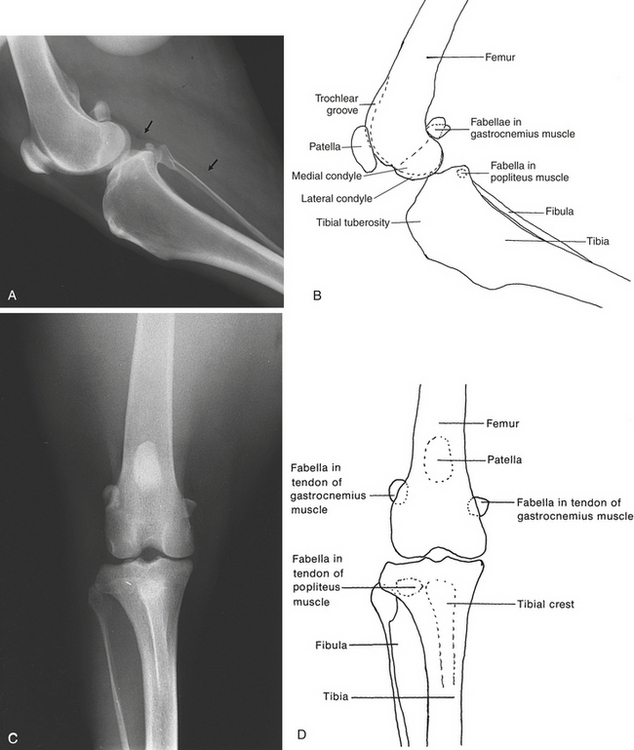
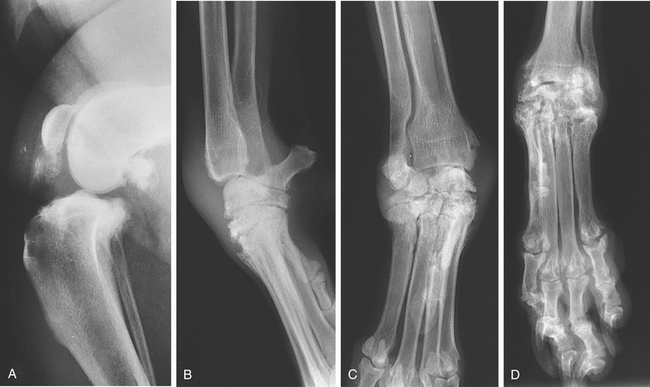
The term fabella describes a small ossification in the medial and lateral heads of the gastrocnemius muscle. Fabellae may be bipartite. There is a fabella or sesamoid bone in the popliteus muscle at the caudolateral aspect of the proximal tibia. Two sesamoid bones are present proximal to the palmar (plantar) aspect of each metacarpophalangeal and metatarsophalangeal articulation. They are numbered 1 to 8, from the medial to the lateral side. The second and seventh are often bipartite with smooth, well-defined edges. This developmental anomaly, often seen in Greyhounds, should not be mistaken for fracture. In Rottweilers, fragmented sesamoids are occasionally seen in the second and fifth digits. The fragments are irregular in outline but are often of no clinical significance (Figure 4-1, C). A single sesamoid lies at the dorsal aspect of each metacarpophalangeal and metatarsophalangeal joint.
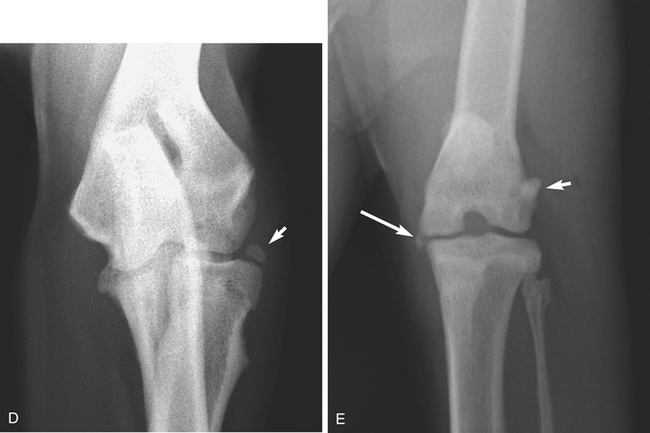
There is sometimes a small sesamoid bone on the craniolateral aspect of the proximal radius. It lies in the supinator muscle but has also been reported to lie in the lateral collateral ligament, the ulnaris lateralis, and the annular ligament (Figure 4-1, D). In the carpus a small sesamoid lies on the distomedial aspect of the radial carpal bone proximal to the first metacarpal bone. It lies in the abductor pollicis longus muscle.
Anatomic variation in the number and location of the fabellae (which are the small sesamoids in the head of the gastrocnemius muscle) at the caudal aspect of the stifle joint can occur in dogs and cats. It is often absent or occasionally displaced distally, particularly in smaller dog breeds (see Figure 4-12, I). Fracture or displacement of sesamoid bones is sometimes seen as a result of trauma (Figure 4-1, E).
Structure
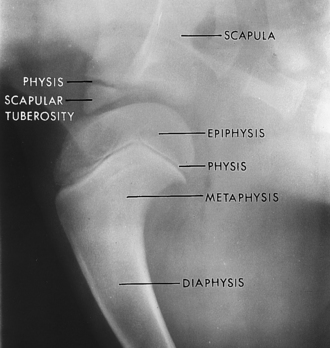
During development, each long bone consists of a shaft (diaphysis), two metaphyses, and two extremities (epiphyses). The diaphysis is composed of dense, compact bone. This dense bone surrounds the medullary cavity, which contains the bone marrow. The epiphyses are centers of growth at either end of the diaphysis. Between the epiphysis and the diaphysis is the physis, or growth plate, and the metaphysis, an area of spongy bone between the physis and the diaphysis. The physis is sometimes referred to as the physeal plate or growth plate in relation to radiographs. When a bone matures, the epiphysis fuses with the metaphysis, and the physis disappears.
Living bone is constantly undergoing remodeling. The bone-forming cells are the osteoblasts. They produce the matrix, often called osteoid, in which mineralization occurs. They elaborate alkaline phosphatase, an indicator of osteoblastic activity. Osteoclasts are responsible for bone resorption. Osteocytes are osteoblasts that have become surrounded by mineralized osteoid. They are found in lacunae within the bone, and they help maintain the calcified matrix. The normal functioning of bone therefore depends on the maintenance of a balance between the activities of these various cells.
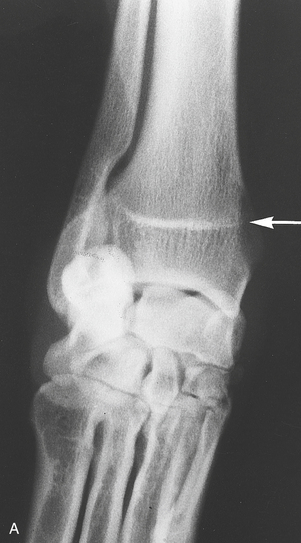
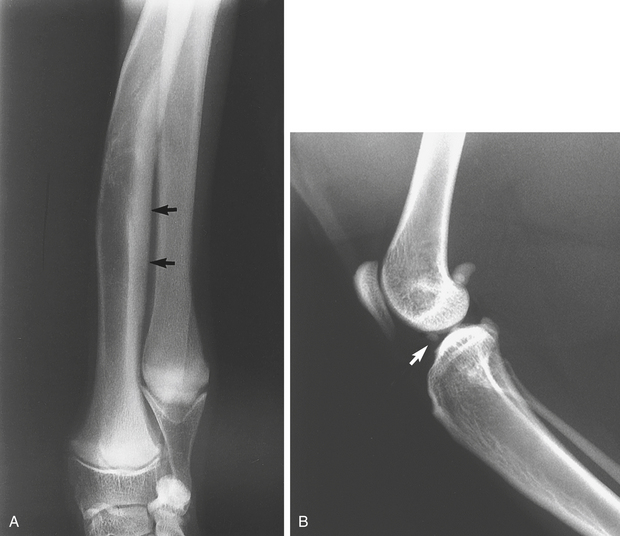
Blood vessels enter a long bone through the nutrient foramen (canal). The nutrient foramen appears as a radiolucent, sharply defined line in the caudal aspect of the cortex. It is directed obliquely cranially and distally. It is seen in the middle to proximal third of the bone diaphysis. There may be some endosteal irregularity in its vicinity. The nutrient foramen should not be mistaken for a fracture line. There is usually one in each bone (see Figure 4-1, A and B).
Normal Appearance
In normal bone, the diaphysis is seen as a band of compact, opaque bone surrounding the medullary cavity, which is more radiolucent. The epiphysis and metaphysis show trabeculations associated with cancellous bone. The trabeculations fade out at the diaphysis. In young animals, the physes (growth plates) appear as radiolucent bands or lines separating the epiphyses from the metaphyses (Figure 4-2). When growth ceases, the epiphyses fuse with the metaphyses and the physes are no longer seen. For some time a band of increased opacity is seen at the junction of the epiphysis and metaphysis, representing the closed physis. This band is sometimes referred to as an epiphyseal or physeal scar (Figure 4-3, A).
It is important to know the positions of the various centers of ossification in the young animal and the times at which the physes close. Subsidiary centers of ossification may be mistaken for abnormalities. Young animals appear to have very wide joint spaces because the cartilaginous models on which the epiphyses and the small bones of the carpus and tarsus are developing are radiolucent. The physes are wide. Growth is completed in dogs by approximately 10 to 14 months of age. However, considerable variations may occur in the times of physeal closure, even in animals of the same breed. In the long bones, the proximal humeral epiphysis is the last to mineralize. The pelvic symphysis may not fuse for several years. The physes of the cat, particularly in the neutered cat, tend to close somewhat later than those of the dog (Table 4-1). Variations occur in the appearance of bones in some breeds, such as in chondrodystrophic animals. Variations such as the irregular outline between the radius and ulna in small-breed dogs are usually of no clinical significance and are considered normal (Figure 4-3, C).
Table 4-1. Age at Appearance of Ossification Centers and of Bony Fusion in the Immature Canine
| Anatomic Site | Age of Appearance of Ossification Center | Age When Fusion Occurs |
|---|---|---|
| Scapula | ||
| Body | Birth | |
| Tuber scapulae | 7 wk | 4-7 mo |
| Humerus | ||
| Diaphysis | Birth | ? |
| Proximal epiphysis | 1-2 | 10-13 |
| Distal epiphysis | ||
| Trochlea of condyle (medial) | 2-3 wk | 6-8 mo to diaphysis |
| Capitum of condyle (lateral) | 2-3 wk | 6 wk to trochlea |
| Medial epicondyle | 6-8 wk | 6 mo to condyles |
| Radius | ||
| Diaphysis | Birth | 6-10 mo |
| Proximal ephiphysis | 8 wk | 8-12 mo |
| Distal epiphysis | 8 wk | |
| Ulna | ||
| Diaphysis | Birth | 6-10 mo |
| Proximal ephiphysis | 8 wk | 8-12 mo |
| Distal epiphysis | 8 wk | |
| Ulna | ||
| Diaphysis | ||
| Olecranon | ||
| Distal epiphysis | ||
| Carpus | ||
| Ulnar | 4 wk | 4 mo |
| Radial | 3-4 wk | |
| Central | 4-5 wk | |
| Intermediate | 3-4 wk | |
| Accessory | ||
| Body | 2 wk | |
| Epiphysis | 7 wk | |
| First | 3 wk | |
| Second | 4 wk | |
| Third | 4 wk | |
| Fourth | 3 wk | |
| Sesamoid bone | 4 mo | |
| Metacarpus | ||
| Diaphysis | Birth | |
| Distal epiphysis (2-5)∗ | 4 wk | 6 mo |
| Proximal epiphysis (1)∗ | 5 wk | 6 mo |
| Phalanges | ||
| First phalanx | ||
| Diaphysis (1-5)∗ | Birth | |
| Distal epiphysis (2-5)∗ | 4 wk | 6 mo |
| Distal epiphysis (1)∗ | 6 wk | 6 mo |
| Second phalanx | ||
| Diaphysis (2-5)∗ | Birth | |
| Proximal epiphysis (2-5)∗ | 5 wk | 6 mo |
| Second phalanx | ||
| Absent or fused with first in first digit | ||
| Third phalanx | ||
| Diaphysis | Birth | |
| Palmar sesamoids | 2 mo | |
| Dorsal sesamoids | 4 mo | |
| Pelvis | ||
| Pubis | Birth | 4-6 mo |
| Ilium | Birth | 4-6 mo |
| Ischium | Birth | 4-6 mo |
| Os acetabulum | 7 wk | 5 mo |
| Iliac crest | 4 mo | 1-2 yr |
| Tuber ischii | 3 mo | 8-10 mo |
| Ischial arch | 6 mo | 12 mo |
| Caudal symphysis pubis | 7 mo | 5 yr |
| Symphysis pubis | 5 yr | |
| Femur | ||
| Diaphysis | Birth | 7-11 mo |
| Proximal epiphysis (head) | 6-10 mo | |
| Trochanter major | 8 wk | 8-13 mo |
| Trochanter minor | 8 wk | 8-11 mo to diaphysis |
| Distal epiphysis | ||
| Trochlea | 2 wk | 3 mo condyles to trochlea |
| Medial condyle | 3 wk | |
| Lateral condyle | 3 wk | |
| Patella | 9 wk | |
| Tibia | ||
| Diaphysis | Birth | |
| Condyles | ||
| Medial | 3 wk | 6 wk to lateral |
| Lateral | 3 wk | 6-12 mo to diaphysis |
| Tuberosity | 8 wk | 6-8 mo to condyles |
| Distal epiphysis | 3 wk | 6-12 mo to diaphysis |
| Medial malleolus | 3 mo | 8-11 mo |
| 5 mo | ||
| Fibula | ||
| Diaphysis | Birth | |
| Proximal epiphysis | 9 wk | 8-12 mo |
| Distal epiphysis | 2-7 wk | 7-12 mo |
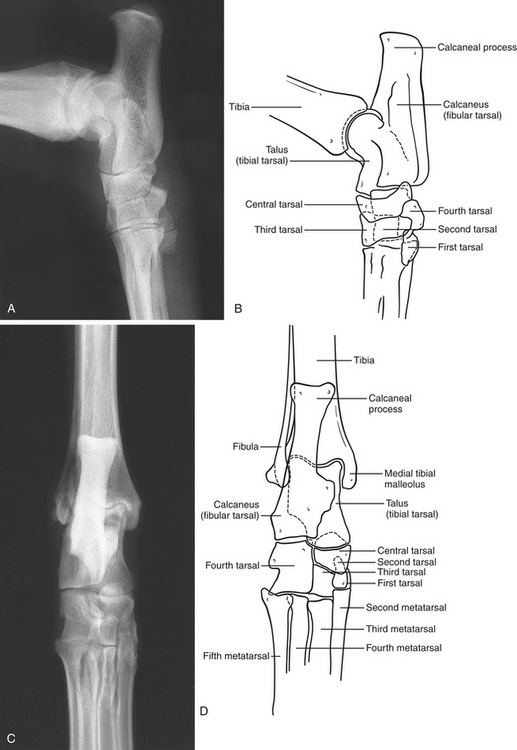
| Tarsus | ||
| Talus (tibial tarsal bone) | Birth-1 wk | |
| Calcaneus (fibular tarsal bone) | Birth-1 wk | |
| Tuber calcis | 6 wk | 3-8 mo |
| Central | 3 wk | |
| First | 4 wk | |
| Second | 4 wk | |
| Third | 4 wk | |
| Fourth | 2 wk | |
| Metatarsus and pelvic limb phalanges are approximately the same as the metacarpus and pectoral limb phalanges. | ||
| Sesamoids | ||
| Fabellar | 3 mo | |
| Popliteal | 3 mo | |
| Plantar phalangeal | 2 mo | |
| Dorsal phalangeal | 5 mo | |
From Ticer JW: Radiographic techniques in small animal practice, Philadelphia, 1975, WB Saunders.
Response of Bone to Injury or Disease
Decreased Opacity
Osteopenia denotes a decreased opacity in bone. It may take the form of osteoporosis or osteomalacia. Osteoporosis denotes a deficiency of mineralization as well as a deficiency of osteoid tissue. Osteomalacia implies a sufficiency of osteoid but inadequate mineralization. Osteoporosis and osteomalacia are indistinguishable radiographically. Care is required with radiographic exposures because overexposed studies may simulate osteopenia.
Increased Opacity
If for any reason growth is arrested, such a period of retarded development is reflected in the skeleton by transverse lines of increased opacity in the diaphyses of long bones adjacent to and parallel with the physes; these are known as growth arrest lines. They are of no clinical significance of themselves (see Figure 4-3, B).
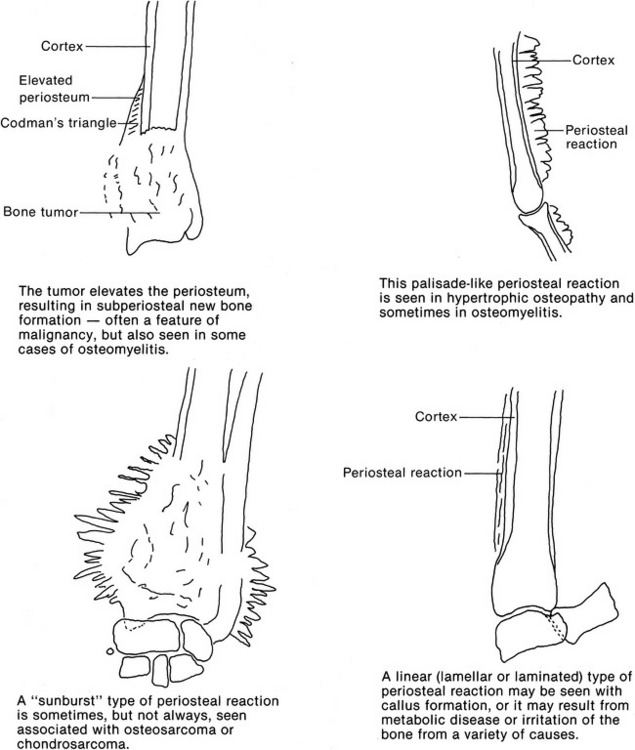
Periosteal Reaction
Palisade reaction: New bone is formed extending in columns outward at right angles from the cortex. The new bone forms a solid continuum. This type of reaction is seen with hypertrophic osteopathy and sometimes osteomyelitis.
The term “aggressive” is often used to describe processes in bone that appear to be very destructive and are not being contained by an inflammatory or defensive reaction. The principal signs of aggression are a proliferative periosteal response that is interrupted in nature, a rapid destruction of bone, poor margination of the lesion, a disorganized reaction, and invasion of the surrounding soft tissues. With aggressive lesions there is a poorly defined transitional zone between affected and unaffected bone. Aggression may be associated with malignancy or with osteomyelitis (Figure 4-4).
Change in Size or Contour
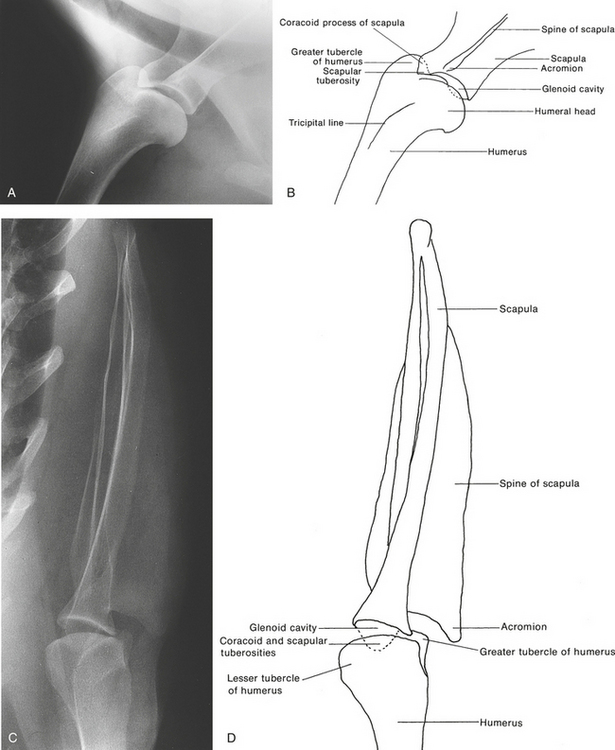
Bones may be of an abnormal size or have an abnormal contour as a result of disease or trauma, particularly during the growth phase. Premature closure of a physis will cause a bone to be shorter than normal. The shortened bone may affect the growth and shape of bones in its immediate neighborhood and result in joint deformity. Bones may have an abnormal size or shape after fracture healing when reduction or immobilization has not been adequate. In the vertebrae, compression fractures result in foreshortening. Bone may remain thickened at the site of a healed fracture (Figure 4-5, A). The term valgus indicates an angulation away from the midline of the body and the term varus, an angulation toward the midline.
JOINTS
Radiography
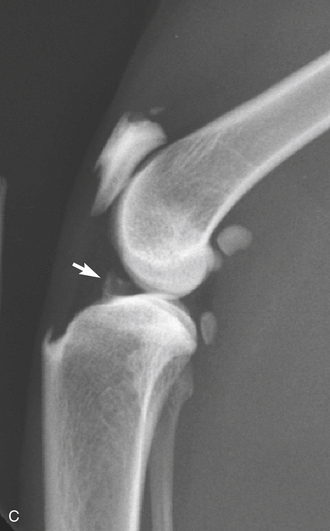
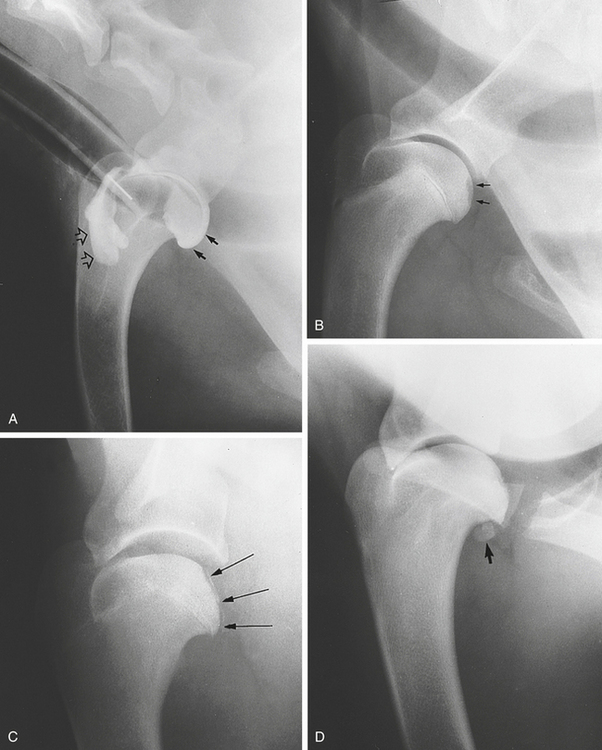
Arthrography—injection of contrast medium into a joint—is not widely practiced in veterinary radiology. Its use has been confined mainly to the shoulder joint to demonstrate defects in the articular cartilage or cartilage flaps in osteochondrosis. It can also be used to demonstrate defects in the joint capsule and abnormalities in the bicipital tendon sheath. A positive contrast medium is preferred. A nonionic, low-osmolar, iodine-based contrast material is used. Iohexol or iopamidol may be used in a concentration of 100 mg/mL. Synovial fluid is first aspirated from the joint, and contrast medium is then injected. The contrast should be diluted to 50% with sterile saline. From 2 to 9 mL is used, depending on the size of the animal. To enter the shoulder joint, a 20- to 22-gauge short bevel or spinal needle is inserted approximately 1 cm below and lateral to the acromion process. The needle is directed distally, medially, and caudally. The joint is manipulated to disperse the contrast material. Radiographs should be taken after 5 minutes. General anesthesia is required, and aseptic procedures are mandatory (see Figure 4-15, A).
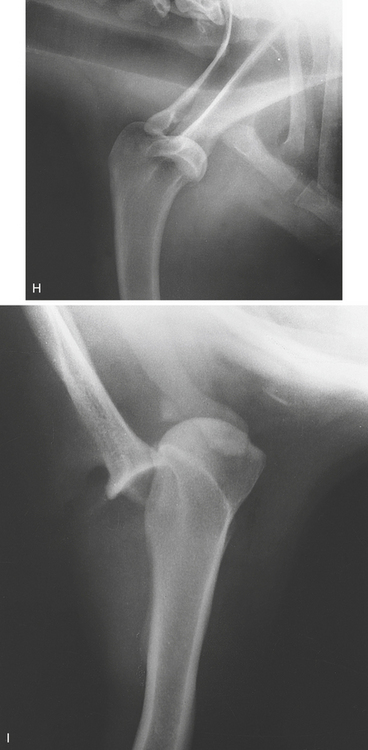
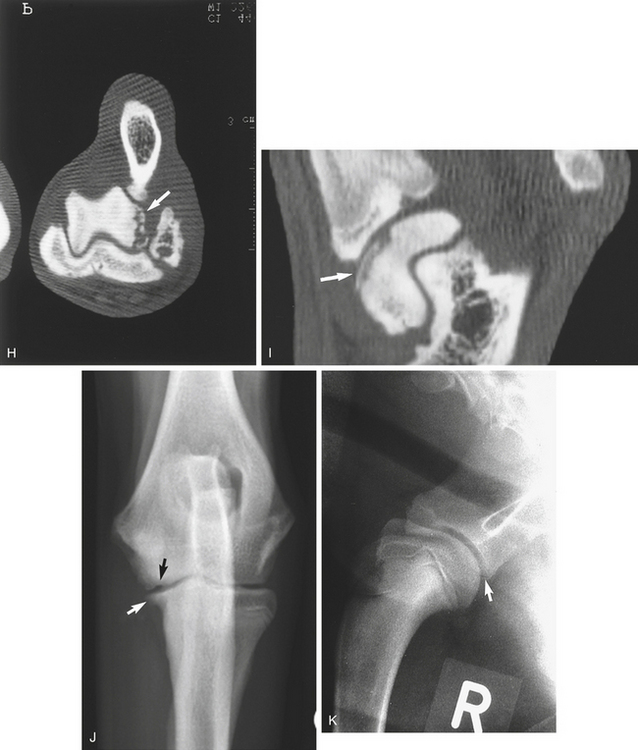
Computed tomography, if available, gives a cross-sectional representation of a joint and enables small fragments or lesions to be identified and localized (see Figure 4-15, H and I).
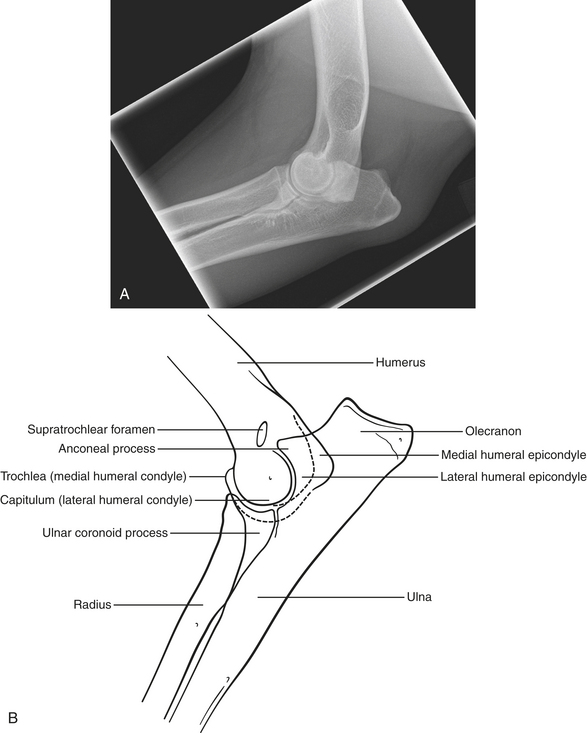
Normal Appearance
The articular cartilages, synovial fluid, and joint capsule are not visible on radiographs. The subchondral bone (i.e., the bone just beneath the articular cartilage) is visible and merges smoothly with the cortex of the metaphysis in mature animals. The infrapatellar fat pad in the stifle joint can be seen on a lateral view as a triangular radiolucency lying caudal to the patellar ligament. The patellar ligament is seen as a soft tissue band attaching to the tibial tuberosity forming the cranial boundary of the fat pad. The fat pad provides contrast so that joint effusion or capsular thickening may be identified. In cats a small triangular mineralized opacity is often seen between the distal femur and proximal tibia (see Figure 4-5, B). The joints in young animals appear to be much wider than those in adults. This is because the immature, largely cartilaginous epiphyses and small cuboidal bones are not fully seen. In very young animals the incompletely ossified epiphysis often has an inhomogeneous mineralization and a stippled, ragged, and irregular margin particularly obvious in large breeds. It should not be mistaken for an abnormality.
Abnormalities
Congenital, developmental, metabolic, and various other conditions can affect bones and joints.
Luxations
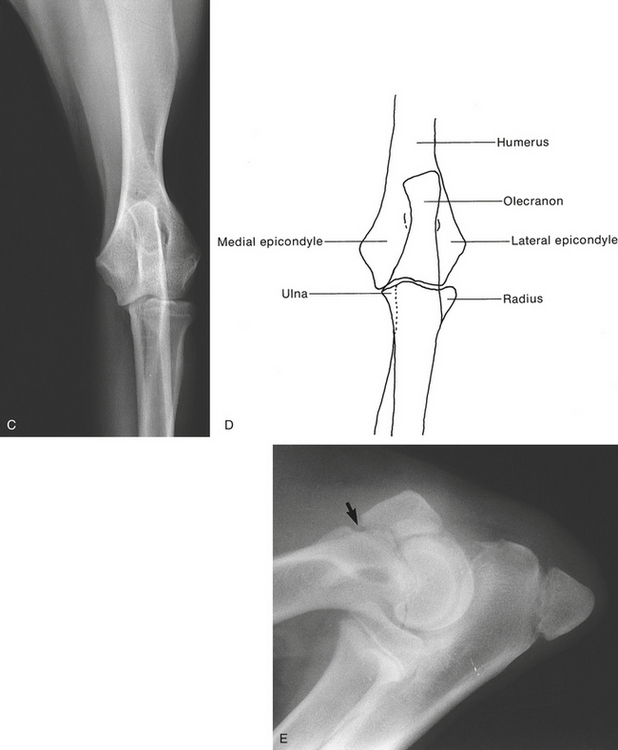
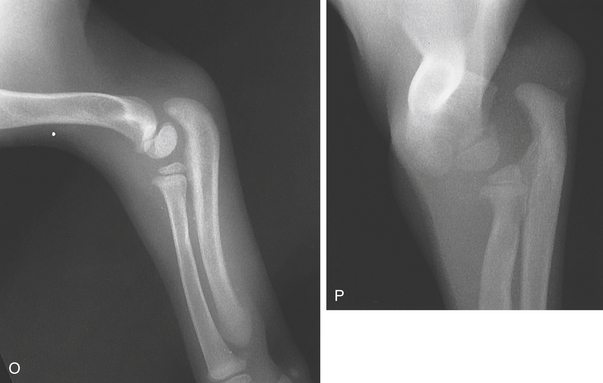
Luxation of the Elbow Joint
Congenital
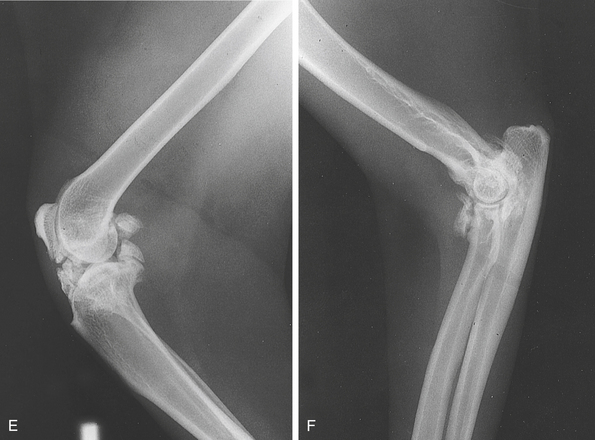
Congenital luxation of the elbow joint is seen in smaller breeds of dogs. Clinically there is either a marked lameness or the limb is being carried. Two types of congenital luxation of the elbow joint are recognized. In one type the humeroulnar joint appears normal but the radial head is displaced laterally and caudally. In the second type the humeroradial joint appears normal but the proximal ulna is rotated through 90 degrees. No semilunar notch is seen on a lateral view of the ulna. Both types of luxation may coexist (see Figure 4-7, P).
Acquired
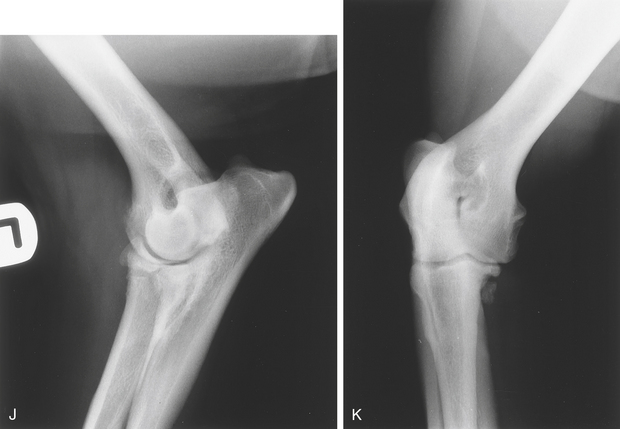
Traumatic luxation of the elbow without an associated fracture results in the radius and ulna being displaced laterally. A luxation associated with a fracture of the proximal ulna results in proximal and cranial luxation of the radial head and caudal displacement of the proximal ulnar fragment. The luxation of the humeroradial joint results in the humeral condyle lying caudal to the proximal radial metaphysis. This is known as Monteggia’s fracture. Subluxation of the elbow joint can occur associated with collateral ligament damage. In such cases stressed studies are useful. In all cases postreduction studies are advisable (see Figure 4-7, H to N).
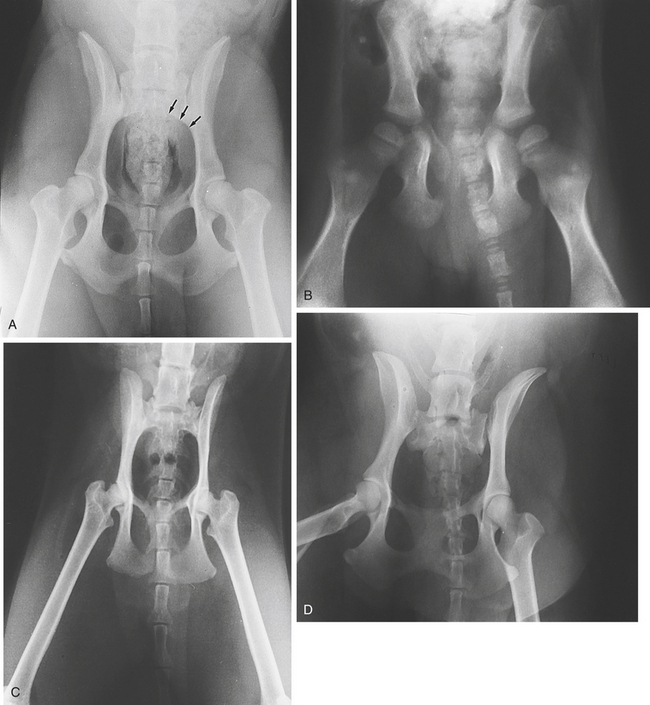
Luxation of the Hip Joint
In hip joint luxation as a result of trauma, the femoral head is usually displaced dorsally and cranially. It may displace ventrally or come to lie immediately dorsal to the acetabulum, where it may be easily missed. Two views at right angles to one another are necessary because a dislocation may be missed on one or the other view. An extended ventrodorsal view is necessary to demonstrate a subluxation that may be missed on inadequately positioned or frog-leg views. An avulsion fracture associated with the ligament of the head of the femur (round ligament) may be seen within the acetabulum. There may also be chip fractures of the acetabular rim. Luxation may also occur as a result of degenerative conditions such as hip dysplasia (see Figure 4-10, E and F).
The Stifle Joint
Rupture of the Cranial Cruciate Ligament
Rupture of the cranial cruciate ligament from trauma may affect any breed of dog. In the larger breeds of dog such as the Rottweiler and Saint Bernard, it may result from degenerative changes in the ligament. It may appear as early as 5 months of age and is often bilateral. A definitive clinical diagnosis is made by demonstrating the cranial drawer sign, although its absence does not preclude a partial tear or disruption. A tibial compression test may also be used. Rupture of the caudal cruciate ligament is rare and usually occurs only with complete luxation of the stifle with rupture of the collateral ligaments and cranial cruciate ligament (see Figure 4-11, H to K).
Radiologic Signs
Congenital Luxation of the Patella
Congenital patellar luxation may result from the following:
There may be an associated abnormal angulation of the distal femur because these abnormalities result in the patellar straight ligament being out of line with the trochlear groove. This abnormal angulation is most common in small dogs. The luxation is almost invariably medial. Lateral luxation of the patella is occasionally seen in large dogs with genu valgum, that is, lateral deviation of the limb below the stifle joint.
Radiologic Signs
Luxation may also be the result of trauma, in which case it may be either medial or lateral.
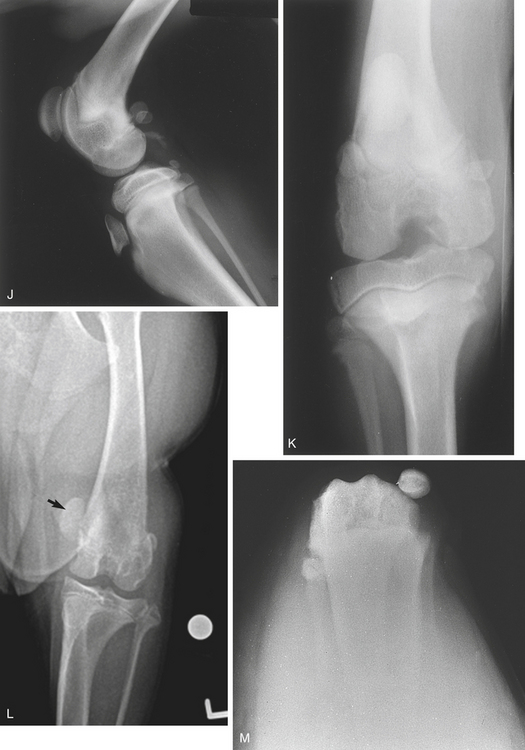
Care should be taken not to rely entirely on the radiographic diagnosis. A luxating patella may be in its normal position when a radiograph is made because positioning the animal for radiography may bring about a temporary reduction of the luxation (Figure 4-11, L and M).
Luxation of the Tarsus
Luxation of the tarsus may be traumatic or congenital. Any of the bones of the tarsus may become displaced after trauma. Such abnormalities are readily detected on standard views (see Figure 4-12, G).
Luxation of the Carpus
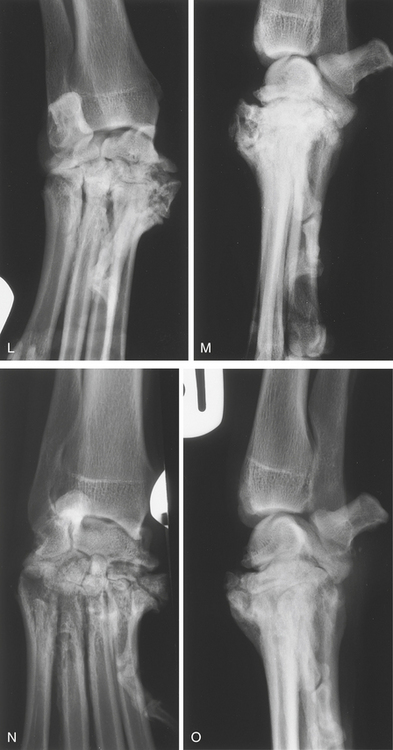
Luxation of the carpus may occur as a result of trauma. Oblique studies are required to identify small fracture fragments associated with luxation. Carpal subluxation or luxation has been described as a syndrome in Shetland Sheepdogs and Collies. It is chronic in onset, and signs of degenerative joint disease are common (Figure 4-13, L to O).
Degenerative Joint Disease
Osteoarthrosis
Degenerative joint disease results in fissure formation and fragmentation of the articular cartilage, which then becomes less efficient in protecting the subchondral bone. This in turn precipitates remodeling changes on the articular surfaces and new bone formation around the edges of the joint. Gas accumulation has been described in the shoulder joint associated with degenerative changes. This is known as the vacuum phenomenon (see Chapter 5, p. 520).
The term osteoarthritis implies inflammation of a joint and adjacent bones.
Radiologic Signs
Inflammatory Joint Disease
Arthritis
Arthritis is inflammation of a joint and may be infectious or noninfectious. The condition involves inflammation of the synovial membrane with a variable degree of involvement of the surrounding joint structures. Noninfectious arthritis is usually the result of immune-mediated disease. A definitive diagnosis often requires arthrocentesis, biopsy, and blood tests. Bone scintigraphy is occasionally helpful in localizing an inflammatory site (see Color Plate 4-30, Z1).
Infectious (Septic) Arthritis
Infectious arthritis may result from wounds or spread of an infectious process from neighboring structures. It may also result from invasion of the joint by blood-borne agents. Clinically, severe lameness, distention of the joint capsule, heat, and pain on palpation occur. Joint movements are limited. Arthrocentesis is the diagnostic method of choice.
Radiologic Signs
Nonerosive
Disseminated Idiopathic Skeletal Hyperostosis
Disseminated idiopathic skeletal hyperostosis, a generalized condition affecting the spine and joints, of a large dog has been reported. Proliferative new bone formation is seen affecting joints and tendon insertions on bony prominences such as the great trochanter of the femur. Changes are also seen on the vertebrae (see Figure 5-35, F).
Synovial Osteochondromatosis
Mineralized chondromas within joint capsules and in the surrounding soft tissues have been described in middle-aged and older larger breed dogs. They are believed to be caused by synovial metaplasia. There may be associated periarticular osteophyte formation. Intraarticular chondromas that do not calcify require demonstration by contrast arthrography, ultrasonography, or magnetic resonance imaging. It is commonly seen in older cats with chronic severe osteoarthrosis. In this species, lesions in the stifle joint must be differentiated from meniscal calcification (see Figure 4-5, B and C).
Bicipital Tenosynovitis
Bicipital tenosynovitis is inflammation of the sheath of the bicipital tendon. Plain radiographs may show a sclerosis in the intertubercular groove with enthesophytes on the supraglenoid tubercle. Arthrography will show irregular distention or incomplete filling, caused by adhesions, of the bicipital sheath. Ultrasonography will demonstrate anechoic fluid in the tendon sheath surrounding the tendon. The tendon may or may not be normal. It may be enlarged or torn. Comparison with the opposite side is useful. Lameness is chronic, affecting one or both forelimbs, and may be intermittent. It is exacerbated on exercise. Pain is elicited on palpation of the shoulder joint and tendon (see Figure 6-7, H and J). Rupture of the biceps brachii tendon sheath has been reported. Arthrography demonstrates leakage of contrast into the soft tissues.
Calcifying Tendinopathy
Calcifying tendinopathy may be associated with bicipital tenosynovitis. Small mineralized opacities may be seen cranial to the intertubercular groove. A tangential (skyline), flexed, proximocranial-distocranial view of the groove will show where the mineralization lies. Ultrasonography may show fiber irregularities and mineralization within the tendon as hyperechoic foci. There may be acoustic shadowing. Movement of the limb in flexion and extension during examination is often helpful. Distension of the joint capsule or tendon sheath may also be seen. It is seen in large breeds, may be bilateral, and may or may not be of clinical significance.
Calcifying tendinopathy may also affect the tendons of the supraspinatus, infraspinatus, coracobrachialis, and gastrocnemius tendons (see Figure 4-14, C).
Developmental Anomalies
Osteochondrosis
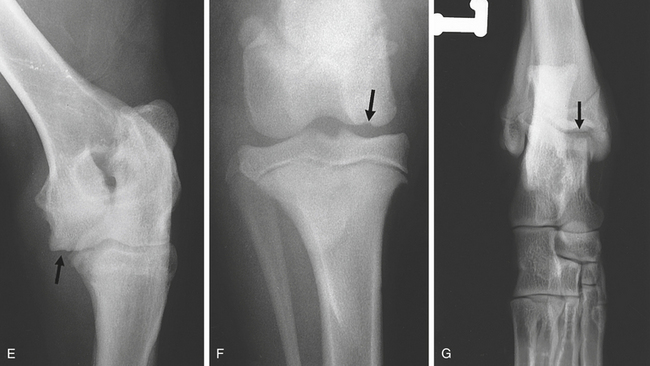
Osteochondrosis occurs in larger dog breeds, usually between 4 and 9 months of age. Affected animals show lameness. Manipulation of an affected joint is resented. A definitive diagnosis is usually made radiographically. The most common site in the dog is the caudal third of the humeral head, but the trochlea of the humeral condyle, the femoral condyles, the medial and lateral malleoli of the tibia, the medial and lateral trochlear ridges of the talus, and the cranial endplate of the sacrum (see Chapter 5, p. 521) may also be affected. Ununited anconeal process and fragmented medial coronoid process of the ulna are believed to be manifestations of osteochondrosis. The condition is frequently bilateral.
Computed tomography is particularly useful in the location and identification of small osteochondral fragments in joints, particularly the elbow and tarsus (Figure 4-15, H and I).