CHAPTER two The Abdomen
THE ABDOMINAL CAVITY
The abdominal cavity is lined by the parietal peritoneum, which is continuous with the visceral peritoneum, which covers the viscera. The peritoneum is covered by a thin layer of fluid. The space between the parietal and the visceral peritoneum is normally a potential space. The mesenteries and the omenta are parts of the peritoneum. The retroperitoneal space is that area dorsal to the peritoneum and ventral to the sublumbar muscles. The kidneys lie in the retroperitoneal space.
Radiography
In elective cases, the patient should be fasted for at least 12 hours before investigation. Water is allowed. The use of a mild cathartic administered the day before the examination is helpful. If the area of interest is the gastrointestinal tract, it is probably best not to give an enema initially because it may cause significant changes in the radiologic picture. An enema may be given after the initial survey studies have been made. Isotonic saline enemas are recommended. The temperature of the enema fluid should be lower than body temperature. This lower temperature helps cause expulsion of much of the gas that would remain in the colon if a warm enema were given.
Evaluation of the Abdominal Radiograph
Normal Appearance
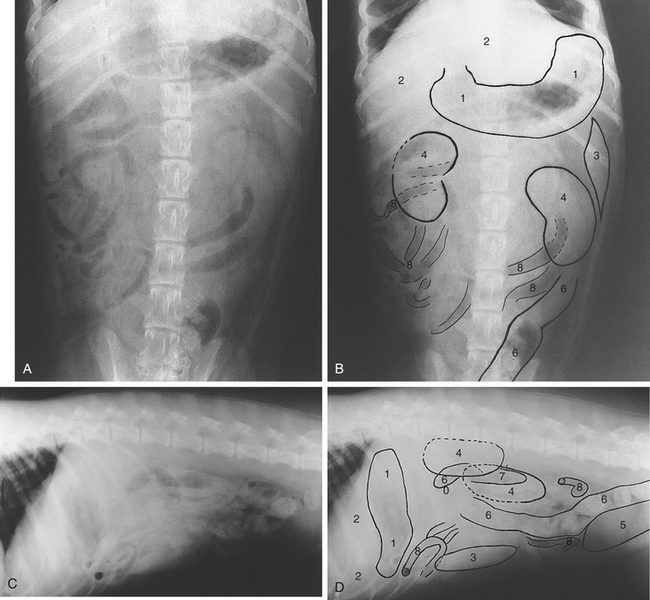
On survey radiographs of the abdomen, the diaphragm, abdominal wall, stomach, small intestine, large intestine, liver, and bladder can usually be recognized. On the ventrodorsal and left-right lateral recumbent views, the spleen is also usually seen. The kidneys may or may not be seen depending on the amount of perirenal fat present. The left kidney is seen in most dogs, whereas only the caudal pole of the right may be visible. The complete outline of both kidneys is usually visible in cats. The os penis is seen in the male dog. The prepuce of the male dog is usually seen because of the air that surrounds it, and the teats are often seen in the female for the same reason. The prostate gland may be seen if there is sufficient intrapelvic fat to outline it. The position and appearance of the normal viscera vary somewhat with the posture of the animal, its conformation, respiratory movements, and the amount of food material present in the alimentary tract (Figure 2-1).
Abnormalities
Abdominal Masses
Masses within the abdominal cavity are from enlargements of one or more of the intraabdominal structures. Enlargement of an organ may be attributable to physiologic or pathologic processes. Distention of the stomach after eating, enlargement of the uterus during pregnancy, and enlargement of the spleen during barbiturate anesthesia are examples of physiologic enlargements. Pathologic enlargement may be the result of inflammatory processes; abscess or cyst formation; hematoma, torsion, obstruction; or neoplasia. Hypertrophy may cause enlargement of an organ.
A mass can usually be identified on a plain radiograph. Abdominal masses are sometimes masked by intraabdominal fluid. If there is accompanying fluid, it should be removed and another radiograph made so that the mass may be more accurately identified. Alternatively, ultrasonography may be used. Some estimation of the origin of a mass may be gained from its position and from the manner and degree of displacement of other organs. Organs amenable to displacement are the stomach, the small and large intestines, the spleen, the uterus, the bladder, and to a lesser extent the kidneys. Movable organs will be displaced in a direction away from the mass. Such displacements often permit the examiner to suggest which structure is enlarged. For example, an enlarged liver displaces the stomach caudally and dorsally.
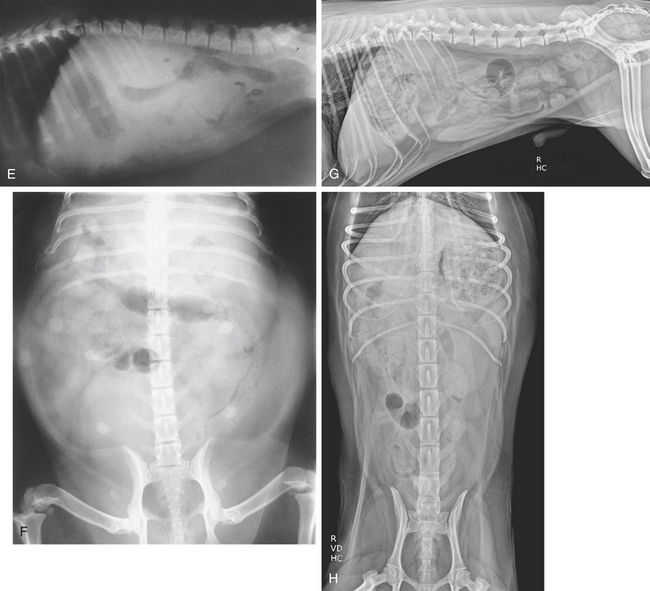
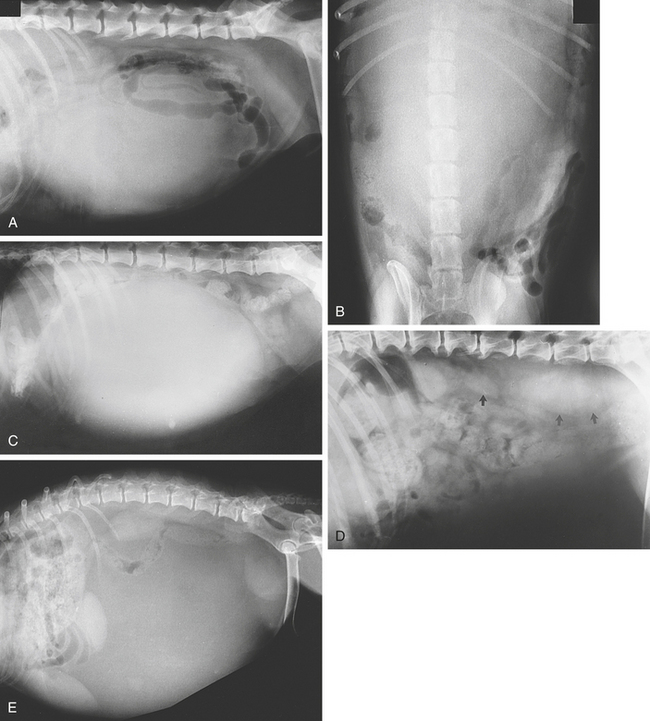
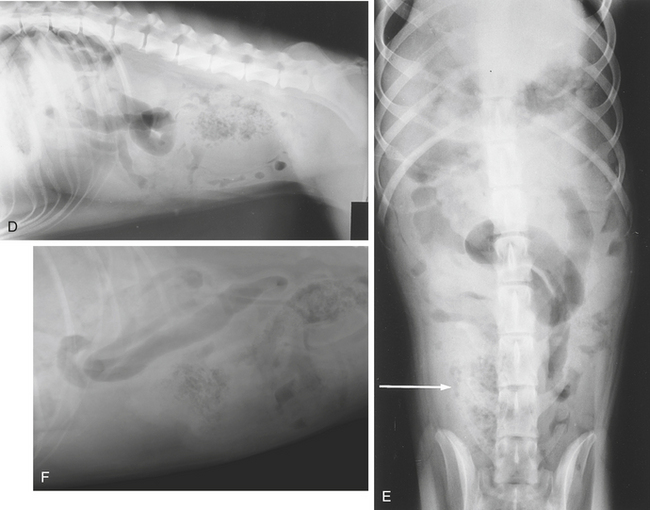
Sublumbar masses can be seen on lateral views. They may be caused by enlarged medial iliac (sublumbar) lymph nodes, enlarged renal silhouettes, ureteral rupture with accumulation of urine, hemorrhage, abscess formation, adrenomegaly, infection, or neoplasia of vertebrae or sublumbar structures. They displace the adjacent abdominal organs ventrally. Enlarged lymph nodes may present as intraabdominal masses in other locations (Figure 2-2, A to E).
Ultrasonography
Ultrasonography is useful in confirming the clinical or radiologic diagnosis of an abdominal mass. It also permits identification and localization of the organ of origin and assists in evaluation of other organs for concomitant disease. It should be done before abdominocentesis. Ultrasound-guided fine-needle aspiration or biopsy aids in a definitive diagnosis of such masses (Figure 2-2, F and G).
Intraperitoneal Fluid
Radiologic Signs
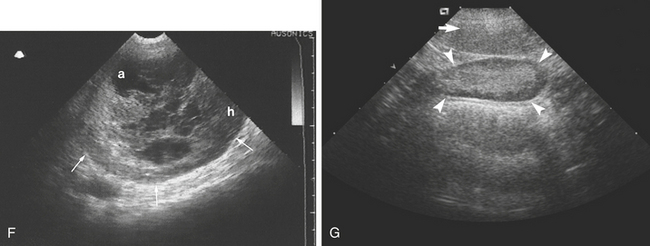
Other conditions may give a somewhat similar appearance to that of ascites. Intraabdominal hemorrhage may be caused by trauma or anticoagulant poisoning. Effusion of fluid may be associated with peritonitis with loss of detail within the abdomen, either localized or generalized, but the abdomen is not distended. Metastatic seeding of neoplasms may cause loss of intraabdominal detail and be associated with effusion. Emaciation causes loss of intraabdominal detail because of fat depletion. Young animals lack intraabdominal fat and thus show poor intraabdominal detail. Care should be taken not to mistake a fluid-filled viscus for ascites. A grossly distended bladder can extend very far cranially into the abdomen. Perinephrotic pseudocysts may be quite extensive and simulate ascites. An enlarged viscus will displace adjacent organs (Figure 2-3, C). Small amounts of fluid can be difficult to demonstrate radiographically.
Ultrasonography
The presence of intraabdominal fluid, which is a hindrance in radiologic evaluation of the abdominal cavity, assists ultrasonographic examination. Ultrasonography is more sensitive than radiography in detecting small volumes of free fluid. Transudates tend to be anechoic. Anechoic fluid dissecting between organs permits their margins to be examined because the fluid profiles organ edges. Fluid surrounding the bladder or gallbladder throws their walls into relief so that their internal and external aspects can be identified. Abdominal organs appear more echogenic than usual when surrounded by intraabdominal fluid. The relative echogenicity of the fluid can be compared with the normal anechoic urine or bile. Free blood in the abdomen has a more echogenic specular texture than a transudate or modified transudate. Peritoneal masses are also seen, provided they are profiled by fluid. Gross abdominal distention resulting from fluid can make examination difficult because the animal may resent transducer pressure. Abdominocentesis relieves the pressure and makes the procedure less stressful, but care must be taken not to introduce air into the abdomen (Figure 2-3, D to F).
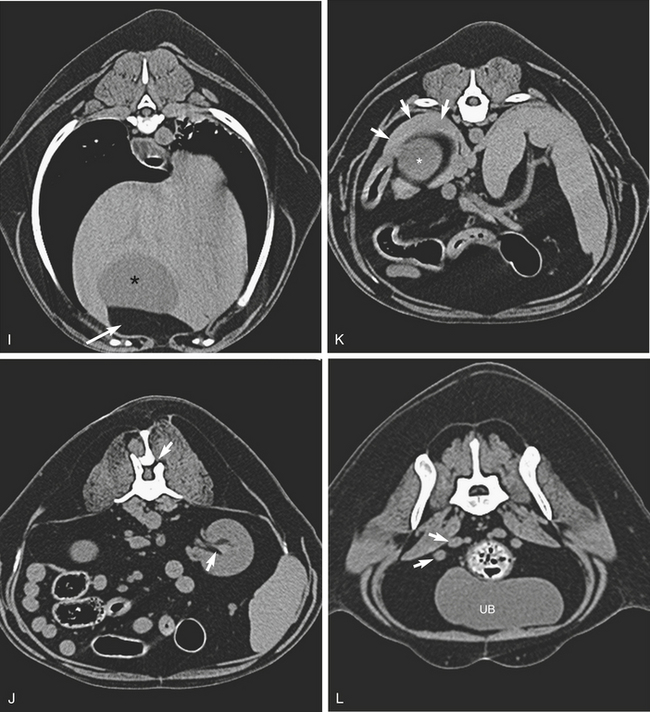
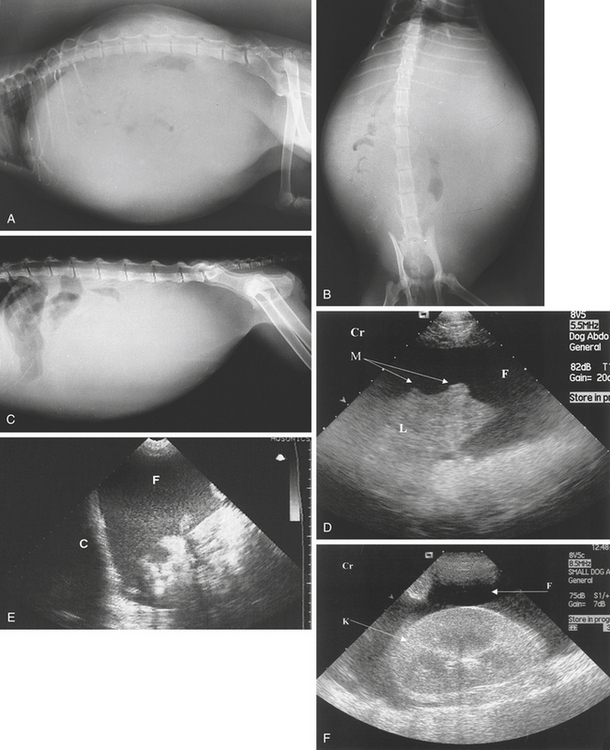
Peritonitis
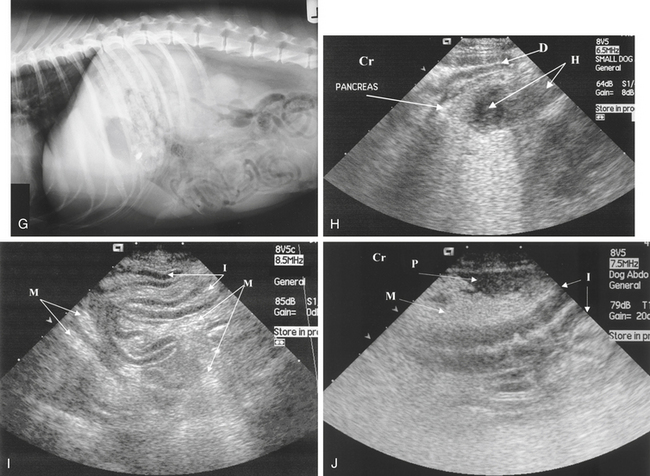
Peritonitis may be localized or generalized. If it is localized, only those structures in the affected area will lose their radiographic sharpness. If it is generalized, there is a widespread haziness of the abdomen. Abdominal carcinomatosis or metastatic neoplasia produces a picture similar to peritonitis. A nodular or granular pattern may be seen (Figure 2-4, A to G).
Ultrasonography
The presence of echogenic particles oscillating in the abdominal fluid with or without strands of hyperechoic tags of fibrin is suggestive of peritonitis. The serosal surfaces of the abdominal organs may show an irregular outline. All abdominal organs should be carefully examined for a potential source of regional peritonitis (Figure 2-4, H to J).
Free Gas in the Abdomen
Radiologic Signs
Ultrasonography
Ultrasound may be more sensitive for detecting small volumes of free gas. The patient should be placed in lateral or dorsal recumbency and a few minutes allowed to elapse before scanning to allow bubbles to rise to the upper abdominal wall. A high-frequency linear probe is recommended. Free gas appears as a hyperechoic structure with comet-tail artifacts immediately adjacent to the inner margin of the abdominal wall. Free gas has a similar sonographic appearance to intestinal gas but is distinguished by the absence of a surrounding bowel wall (Figure 2-5, F).
THE ABDOMINAL WALL
Abnormalities
A disruption in the continuity of the diaphragm or the abdominal musculature results in a rupture. There may be mineralization within the muscles in Cushing’s disease (see Figure 6-1, F). Gas may track along fascial planes in pneumomediastinum or after trauma. Tumors of the abdominal wall are rare and the outline may be obscured by intraabdominal fluid.
Hernias
Ultrasonography can be used to identify the contents of a hernia. Fat will be identified as relatively hyperechoic material within the sac. Intestinal loops may be seen as linear structures containing hyperechoic gas, anechoic fluid, or a mixture of both. Peristalsis may be appreciated if present. If the bladder is herniated and if it contains urine, it is easily identified because the anechoic urine readily confirms the diagnosis. Figure 2-6 shows examples of hernias and ruptures.
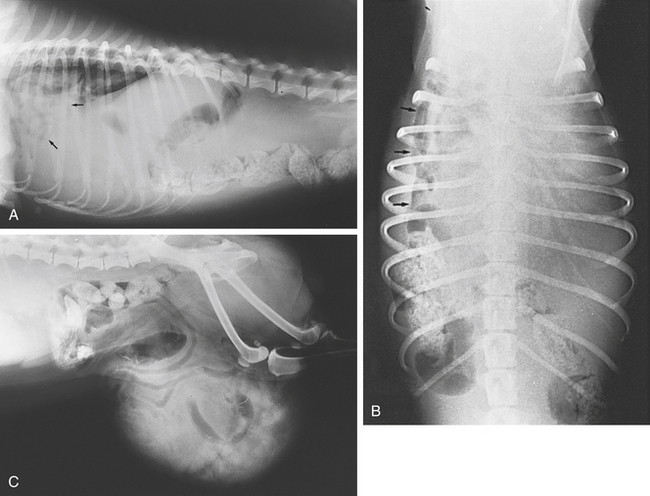
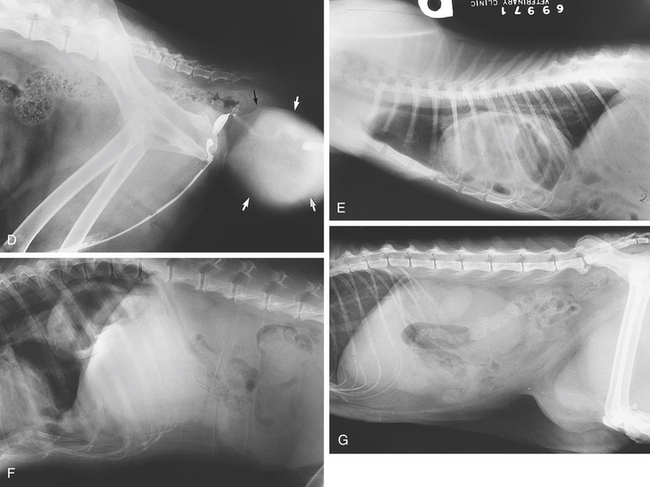
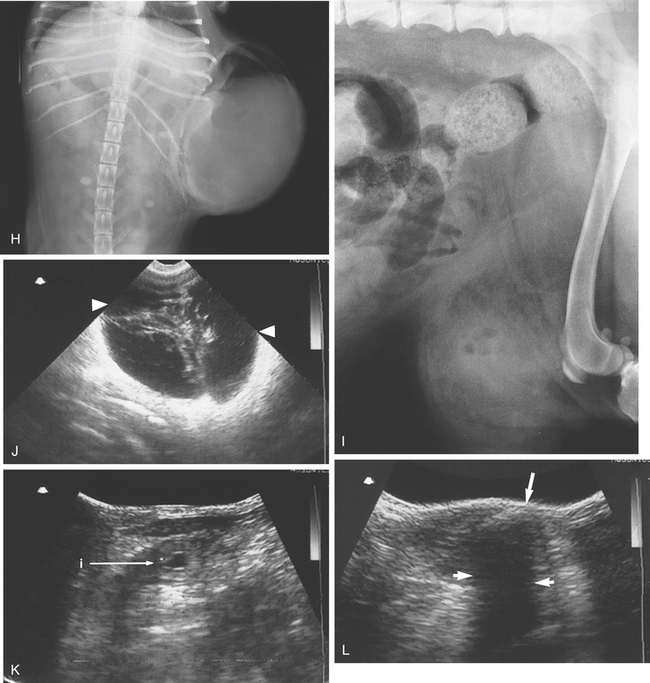
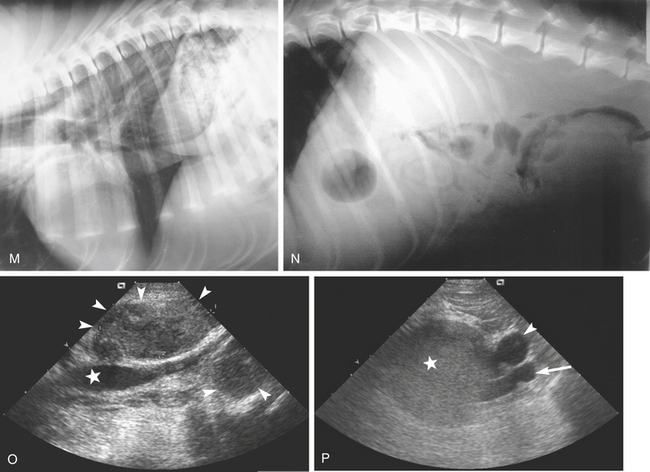
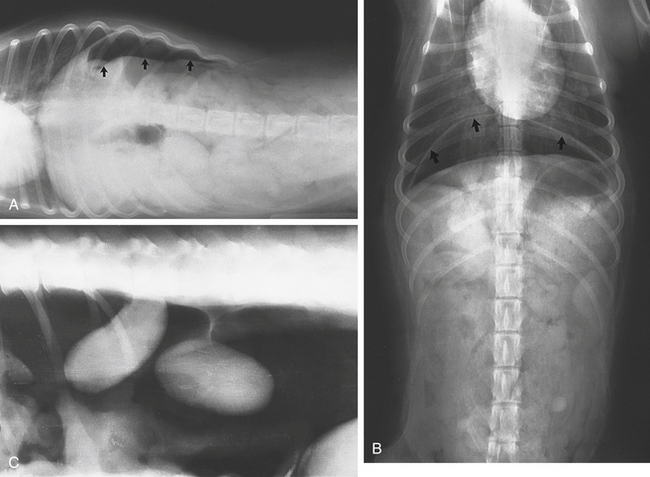
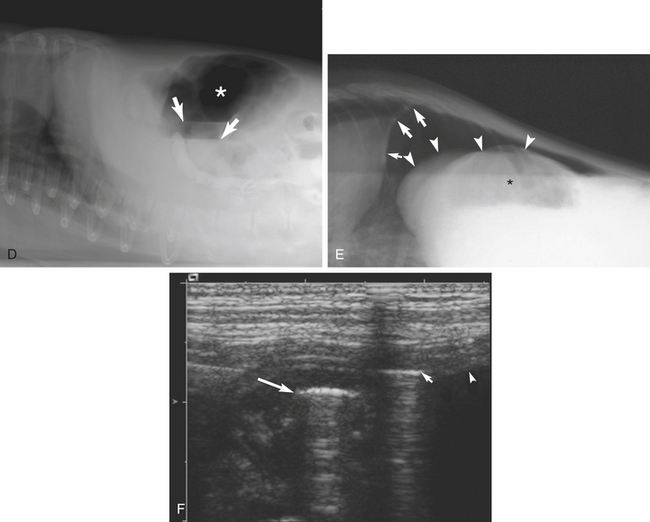
Figure 2-6 A and B, Diaphragmatic rupture (hernia). Small intestine gas shadows can be seen within the thorax (arrows). The abdomen appears empty except for the large intestine. The diaphragm lines are obscured. C, A large inguinal hernia. Small intestine gas shadows are seen within the hernial swelling on this lateral view.D, A perineal hernia containing the bladder. The bladder is outlined by positive contrast medium (arrows). E, Peritoneopericardial hernia. The cardiac shadow is enlarged and distorted. Small and large intestinal gas shadows can be seen within the cardiac outline (see Chapter 3, p. 257). F, A 4-year-old Labrador had surgery for a long-standing diaphragmatic hernia some 4 weeks before presentation. A portion of stomach can be seen in the caudodorsal thorax. This proved to be a hiatal hernia. G, Inguinal hernia. A 5-year-old female domestic short-haired cat had been off form for several months. The left kidney is grossly enlarged. The bladder lies ventral to the abdominal floor in an inguinal hernia and is seen just cranial to the femurs. Ultrasonography showed the left kidney to be hydronephrotic. The cause was obstruction of the ureter caused by the abnormal bladder location.H, Paracostal hernia. A 10-year-old crossbred Terrier was lame and had a subcutaneous swelling over the ribs. The ventrodorsal radiograph shows a large soft tissue mass with a gas shadow cranially in the left paracostal region. The adjacent ribs are spread by the mass. This was a herniated stomach. I, Inguinal abscess. This 7-year-old Cocker Spaniel had an inguinal hernia repair 4 days before presentation. There was vomiting, polydipsia, and polyuria. The hernial mass was fluctuant. A lateral radiograph shows a soft tissue swelling lying ventral to the abdominal wall and containing gas and fat opacities. J, This 12-year-old Pointer has a large fluid-filled structure within an inguinal mass (arrowheads). A large, predominantly anechoic, fluid-filled mass lies within the inguinal area. The lumen contains some echogenic material. Several stellate hypoechoic fibrin strands or septa are scattered throughout the mass. Diagnosis: postoperative seroma. K, A fluid-filled loop of intestine (i) is seen in cross-section within a small inguinal hernia. L, This dog was involved in a road traffic accident 2 weeks earlier. On clinical examination there was a nonreducible mass in the inguinal region. A gas-filled loop of intestine (arrow) lies within an inguinal hernia. An acoustic shadow is seen distally (short arrows).M, Hiatal hernia. A 9-month-old Wolfhound puppy had a history of acute vomiting for 4 weeks. A lateral radiograph shows the food-filled fundus of the stomach herniated through the esophageal hiatus and lying in the caudodorsal thorax. There is air in the esophagus dorsal to the trachea. N, Retroperitoneal hemorrhage. This Greyhound had a history of poor performance and recurrent abdominal distention after work. The lateral radiograph shows a retroperitoneal soft tissue opacity displacing the abdominal organs ventrally. O and P, Sagittal (O) and transverse (P) images of the caudal abdomen at the level of the terminal aorta. O, Rounded, plump medial iliac lymph nodes (arrowheads) lie adjacent to the terminal aorta (asterisk). P, The transverse image shows an enlarged lymph node (asterisk) lying laterally to the caudal vena cava (arrowhead) and aorta (arrow). This was a lymphosarcoma.
Inguinal Hernia
Radiography can be helpful in determining the contents of an inguinal hernia. Gas shadows within the hernial outline indicate the presence of a portion of intestine. The uterus casts a homogeneous, fluid type of opacity, as does the bladder. Fetal skeletons may be seen if the animal is in late pregnancy. A barium study can be used to determine the position of the intestine. Ultrasonography will determine the contents (Figure 2-6, C, G, K, and L).
Perineal Hernia
Fat, a displaced rectum, or the anechoic urine-filled bladder may be identified in the perineal swelling on ultrasound examination (Figure 2-6, D).
Hiatal Hernia
In this hernia there is a protrusion of the stomach, or part of it, through the esophageal hiatus of the diaphragm, displacing the terminal esophagus cranially. The cardiac area of the stomach is most likely to be involved. The term hiatal hernia implies a herniation of part of the stomach through the esophageal hiatus into the thorax. With the sliding type of hernia, the displacement is intermittent and usually affects the gastroesophageal junction, together with the cardia of the stomach. A barium study will show the position of the stomach. These hernias are common in brachycephalic dogs. To demonstrate this hernia, it may be necessary to have the animal tilted with the head down because the stomach may slide into and out of the thorax. Fluoroscopy, while feeding the animal barium mixed with food, may show a sliding hernia.
In a paraesophageal hernia a portion of the stomach passes through the esophageal hiatus to lie alongside the esophagus. This type usually does not affect the gastroesophageal junction and is rare in dogs and cats. Clinical signs are primarily dysphagia, regurgitation, and discomfort after eating (Figure 2-6, F and M). Gastroesophageal intussusception is a rare form of hiatal hernia in which all or part of the stomach invaginates into the esophagus (see p. 75). The hernia appears as an elongated fusiform soft tissue mass in the dorsal thorax, displacing the trachea ventrally and distorting the heart. The absence of a normal stomach shadow in the abdomen is an important radiographic clue.
Diaphragmatic Hernia
Diaphragmatic hernia (rupture) is described in Chapter 3. Celiography or peritoneography, that is, introduction of contrast medium into the peritoneal cavity, has been described as an aid in the diagnosis of these hernias. Abdominal organs may be seen within the pericardium in peritoneal pericardial hernia (see Chapter 3, p. 257; and Figure 2-6, E).
Abscess
On radiographs an abscess presents as an intraabdominal mass. It may be homogeneous in nature or contain focal lucencies. There may be local lack of serosal detail because of peritonitis. Regional ileus and bunching of the intestines may be observed. Abscess formation may be caused by perforation of the gastrointestinal tract, pancreatitis, foreign body such as a surgical swab or sponge, or trauma (see Figure 2-4, D to F, and Figure 2-6, I).
Ultrasonography
On ultrasonography, intraabdominal abscesses, or abscesses within hernias, produce hypoechoic, poorly marginated masses containing variable quantities of fluid. They usually have a mixed echogenic appearance and are surrounded by a capsule and may be attached to the serosal surface of abdominal organs or to the abdominal wall. Adjacent inflammation may be indicated by hyperechoic fat, pockets of anechoic/hypoechoic fluid, and regional intestinal ileus (see Figure 2-4, H). The presence of echogenic particles oscillating in the abdominal fluid with or without strands of hyperechoic tags of fibrin is suggestive of peritonitis. Serosal surfaces of adjacent organs may show an irregular outline (see Figure 2-4, I and J).
THE RETROPERITONEAL SPACE
Abnormalities
The retroperitoneal space may be the seat of sublumbar masses caused by abscessation; enlarged lymph nodes, kidneys, or adrenal glands; or neoplasia of sublumbar muscles, connective tissue, or vertebrae. Retroperitoneal fluid may be caused by hemorrhage or leakage of urine from the kidneys or ureters (Figure 2-6, N). Gas or air from a pneumomediastinum is occasionally seen outlining structures in this region.
Ultrasonography
Ultrasonographic examination permits examination of the sublumbar region. Lymph nodes, vessels, and kidneys are clearly visible. Masses in the region are readily accessible for fine-needle aspiration or biopsy provided that major blood vessels are avoided (Figure 2-6, O and P).
Abdominal Blood Vessels
Similarly, the main branches of the vena cava are the common iliac veins, paired deep circumflex iliac, right testicular or ovarian, paired renal and phrenicoabdominals, and multiple hepatic veins.
The portal vein is located in the midventral abdomen and is the vessel closest to the transducer when imaging from the right side with the animal in left lateral recumbency (Figure 2-7, H and I).
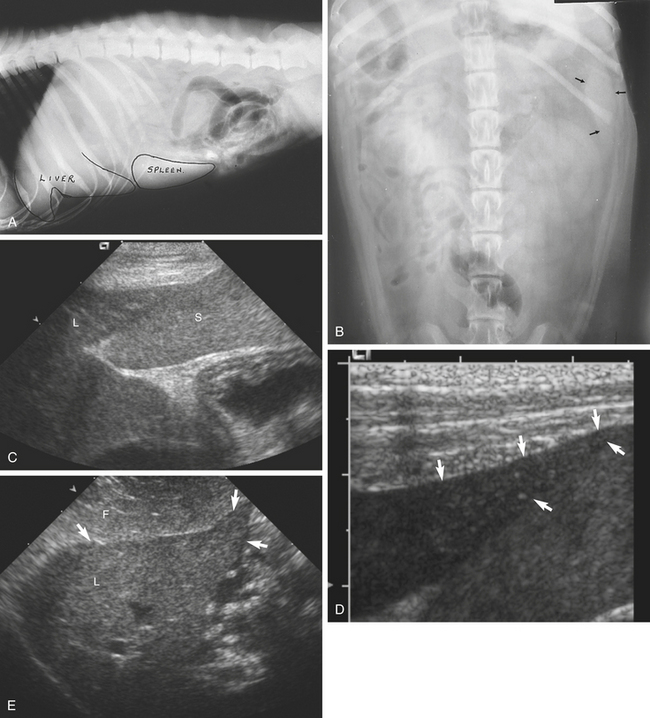
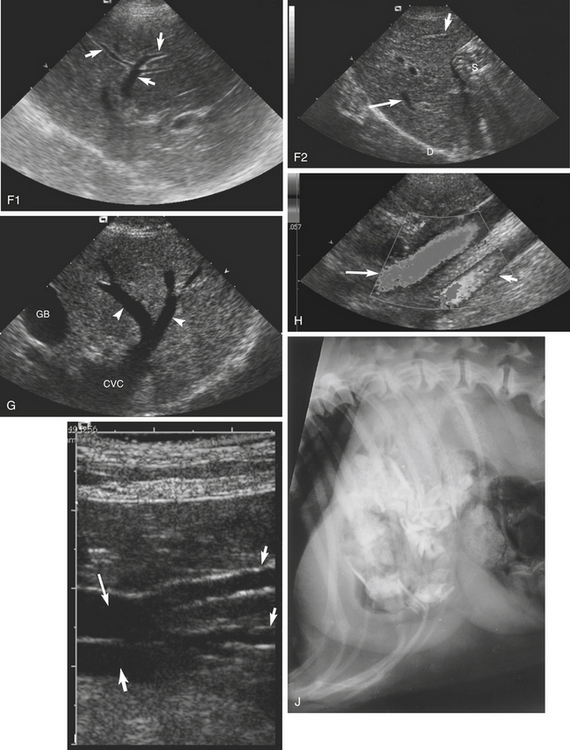
Figure 2-7 A, Positions of the normal liver and spleen. B, A ventrodorsal view of the abdomen with the outline of the head of the spleen (arrows). C, Midline sagittal sonogram of the cranial abdomen. The relative echotextures of the liver (L) and spleen (S) can be seen. The spleen is hyperechoic compared with the liver. The structure in the far right field is the fluid-filled stomach. D, Normal sharp edge to the caudal liver margin (arrows). E, Midline sagittal sonogram of the liver (L) of a fat dog showing a large quantity of fat (F) in the ventral abdomen outlining the liver margin (arrows).F1, Normal portal vessels (arrows) in the liver. The portal vessels have bright hyperechoic walls. F2, This midline sonogram of the liver shows normal portal vessels (short arrow) and hepatic veins (long arrow). G, Hepatic veins (arrowheads) draining into the caudal vena cava (CVC). GB, gallbladder. H, Color flow Doppler sonogram showing the caudal vena cava (long arrow coded blue) traveling toward the diaphragm. The aorta is seen in the far field (short arrow, coded red) (see Color Plate 2-7, H). I, This sagittal plane sonogram shows the terminal aorta bifurcation (long arrow) and caudal vena cava (medium arrow) bifurcation and the external iliac vessels (small arrows). J, Bones in the stomach of this 11-year-old Labrador were an incidental finding and were fully digested 24 hours later.
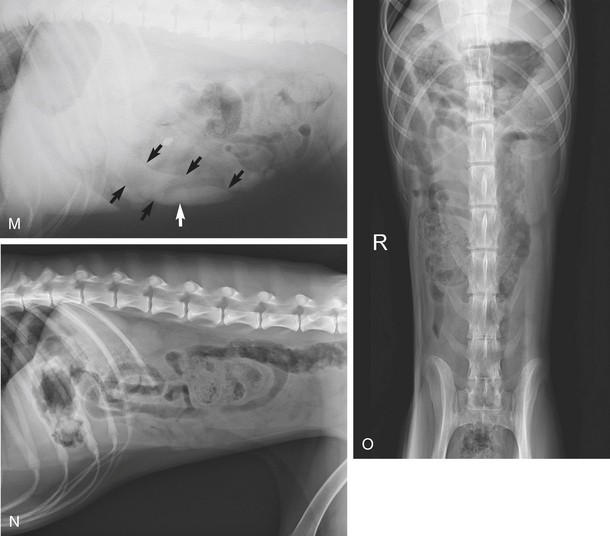
THE LIVER
Anatomy
The liver lies within the intrathoracic portion of the abdomen. It is made up of six lobes, the left medial, left lateral, right medial, right lateral, quadrate, and caudate lobes. Cranially the liver is convex in outline and lies, for the most part, in contact with the diaphragm. Caudally it is in contact with the right kidney at the renal fossa, the cranial flexure of the duodenum, and the stomach. The depth of the abdomen is greatest in this area. Its right border is formed by the right medial lobe cranially and the right lateral lobe and the caudate process of the caudate lobe caudally. Its left border is formed by the left medial lobe cranially and the left lateral lobe caudally. The quadrate lobe is centrally placed cranially. To the right and to the left the liver is adjacent to the abdominal wall. The gallbladder is situated in the right cranioventral abdomen.
Normal Appearance
On the ventrodorsal view, the liver appears as a homogeneous soft tissue opacity caudal to the diaphragm. Its outline is not well marked. Its caudal border on the right side may be determined from the position of the cranial duodenal flexure and the cranial pole of the right kidney in obese animals. Centrally the lesser curvature of the stomach marks its caudal limit. On the left it is covered by the fundus of the stomach. The caudal lobes of the lungs are superimposed on the liver to some extent on both lateral and ventrodorsal views, and pulmonary vessels are frequently seen superimposed on the liver shadow.
The area of the falciform ligament appears larger on expiration than on inspiration. In the cat a distended gallbladder may protrude, simulating hepatomegaly. In obese cats, fat in the falciform ligament may displace the liver dorsally (Figure 2-7, A and B).
Ultrasonography
The hepatic tissue is loosely granular, with an even echotexture and echogenicity. The portal vessels are identified by their bright hyperechoic walls. Hepatic vessels are seen as anechoic linear and circular areas scattered throughout the liver. The hepatic arteries and bile ducts are not usually identified. The cranial border of the liver is identified as a hyperechoic curving border that represents the interface between the lungs and the diaphragm. Liver margins should be sharp and well defined. The relative echogenicity of the liver to adjacent and presumably normal organs should be compared to establish whether any marked abnormalities are present. The liver is hypoechoic compared with the spleen and equal to, or more echoic than, the kidney cortex. However, more than one organ may be abnormal, so comparative observations should be made with caution. The gallbladder is seen as a large pear-shaped anechoic structure on the right side of the liver. Sometimes granular sediment is present, particularly in fasting animals. Various artifacts may be associated with the gallbladder: acoustic enhancement, side-lobe artifact, and edge shadowing (see Chapter 1, pp. 17 and 19).
The caudal vena cava is identified in the midhepatic region traversing the diaphragm (Figure 2-7, G and H). The stomach is seen lying caudal to the liver. Gastric gas is identified as a hyperechoic region undergoing peristalsis within the stomach. The pylorus may be identified as a vaguely circular structure in the right ventral abdomen. The falciform fat that lies ventral to the liver may interfere with the liver examination. It has a variable echogenicity and a linear woven texture. In obese animals, image quality may be less than ideal. Ultrasonographic criteria for hepatic size are not reliable in inexperienced hands (Figure 2-7, C to G).
Abnormalities
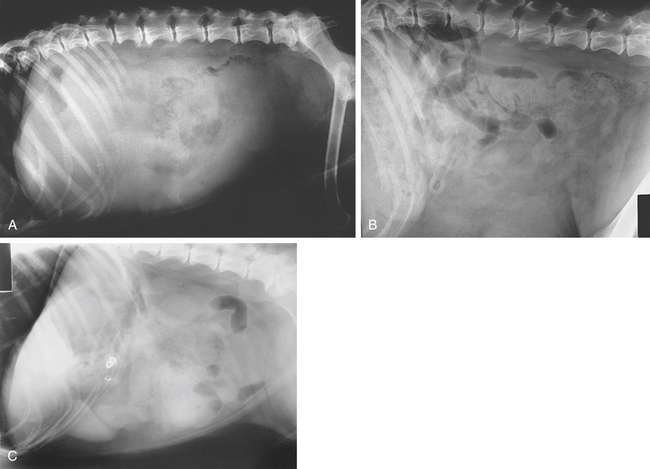
Enlargement (Hepatomegaly)
Radiologic Signs
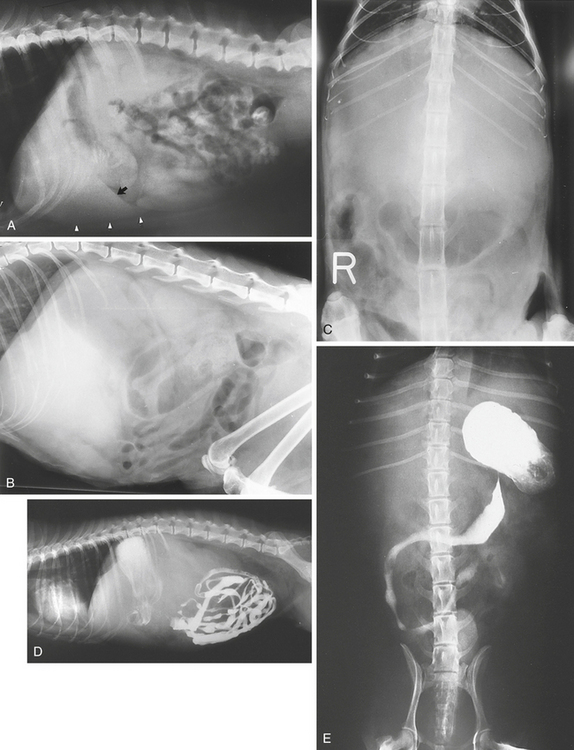
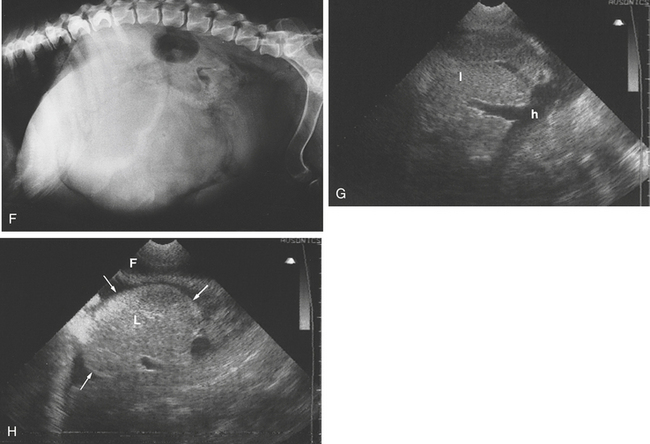
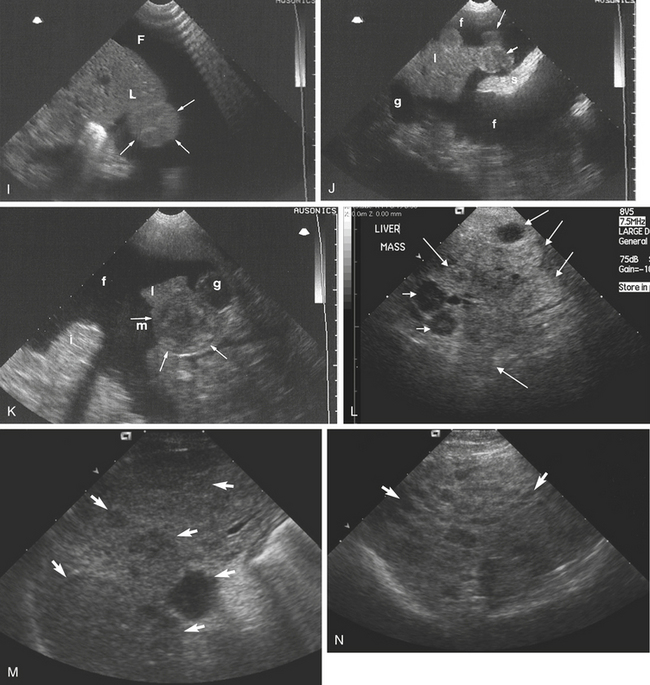
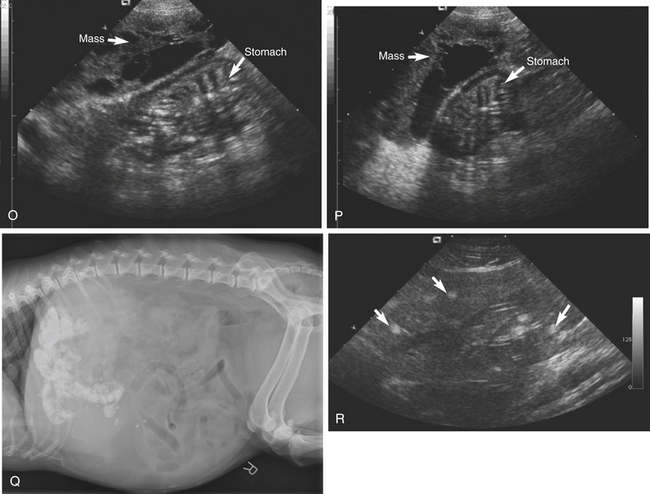
Figure 2-8 A, Enlargement of the liver. The liver (arrowheads and arrow) is seen to extend well beyond the costal arch. B and C, Hepatomegaly. An 11-year-old domestic short-haired cat was suspected to have lymphosarcoma. The gastric silhouette is displaced caudally on both views by an enlarged liver. D, and E, Displacement of the stomach and duodenum by an enlarged liver. The full extent of the displacement is not obvious on the lateral view. This is a good example of the value of two views. A carcinoma of the bile duct was found at autopsy. The kidneys are displaced caudally.F, This 11-year-old Glen of Imaal Terrier presented with a history of seizures over the previous 24 hours. The animal was anemic and had an elevated alanine aminotransferase (ALT) level. The lateral radiograph shows a vaguely circular, large, soft tissue opacity caudal to the costal arch and pylorus. At surgery this proved to be a pedunculated tumor involving a single hepatic lobe. It was a hepatocellular carcinoma. G and H, This 9-year-old Springer Spaniel was in the late stages of heart failure. G, The hepatic veins (h) are markedly enlarged and extend deeply into the liver tissue (l). H, The liver margin (L) is enlarged and rounded (arrows) and is outlined by anechoic fluid (F) in the peritoneal cavity. The fluid was a transudate.I to O, Metastatic lesions in the liver have variable sonographic presentations, and not all parenchymal changes in the liver are pathologic. Fine-needle aspirates or biopsy is required to make a definitive diagnosis. I, Intraabdominal fluid (F) surrounds a bulbous protrusion (arrows) of a liver lobe (L). The hepatic margins are rounded. Poor skin contact has caused a reverberation artifact on the right corner of the image. J, A 6-year-old Retriever with ascites. Intraabdominal fluid (f) outlines a neoplastic hypoechoic nodule (arrows) at the tip of the liver lobe (l). s, Spleen; g, gallbladder. K, This is a paracostal view from the right side of the abdomen of a 10-year-old German Shepherd with ascites. A discrete circular mass (arrows) occupies the tip of the liver margin. This was a metastasis from a splenic hemangiosarcoma. The gallbladder (g) lies adjacent to the neoplasm. m, Mass; i, intestine; l, liver; f, fluid. L, A midline sagittal sonogram of the cranial abdomen in this dog shows multiple masses. Some are hypoechoic and hyperechoic (medium arrows). Others have a central hyperechoic region (short arrow) typical of a so-called target sign within the liver. These are multiple metastases. M, Hypoechoic metastatic masses of various sizes (arrows) are seen scattered throughout the liver. N, This lacy, hypoechoic pattern (arrows) is sometimes associated with metastatic disease. In this case it was caused by lymphoma.O and P, In some cases metastases may contain loculated anechoic areas. These are sagittal and transverse sonograms of a caudal liver lobe margin containing an anechoic fluid-filled septated mass (arrows). Diagnosis: hemangiosarcoma. Q, This 13-year-old Shetland Sheepdog presented with ascites. This lateral radiograph shows diffuse nodular mineralization throughout the hepatic parenchyma. Some isolated, focal, round, mineralized foci seen in the midventral abdomen are probably in the spleen. Serosal detail is poor in the cranioventral abdomen. The small intestine is displaced caudally. This is the same case as Figure 2-11, M. Diagnosis: diffuse hepatic disease. R, Hyperechoic circular nodules (white arrows) are seen throughout the liver of this cat. They were incidental findings and of no clinical significance and may be a result of parasitic infestation. Histopathologic confirmation was refused by the client.
Localized masses within the liver, depending on their size and location, can cause a variety of displacements of adjacent organs. In general, masses in the right side of the liver tend to displace the stomach and duodenum to the left and dorsally, and left-sided masses tend to displace the stomach and spleen to the right and dorsally. A mass originating in the right side of the liver can displace the tail of the spleen caudally. A mass originating in the caudate lobe of the liver can displace the right kidney caudally. Hepatic cysts may be mistaken for hepatic neoplasia because they may cause severe, focal hepatic enlargement (Figures 2-9 and 2-10, O). Liver masses can displace the small intestine caudally.
Discrete or diffuse mineral opacities are occasionally seen in the liver. They may be associated with neoplasia, granulomatous diseases, or parasites. Dystrophic calcification may be of no clinical significance (see Figure 6-1, E).
Ultrasonography
On ultrasonography the liver will appear enlarged with smooth margins. In patients with generalized hepatomegaly, the ventral aspect of the liver extends further caudally than is normal and makes the sonographic window for evaluation of the liver much larger. The liver may extend caudally as far as the umbilicus, so that if the probe is placed on the skin midway between the xiphoid and the umbilicus, the field of view is filled with liver. Hepatic enlargement can also be assessed by examining the caudate lobe of the liver and the right kidney. If the liver size is normal, the cranial pole of the right kidney sits in the renal fossa of the caudate lobe, and the depth of the caudate lobe and kidney are approximately the same. With severe generalized hepatic enlargement, the caudate lobe appears to partially surround the right kidney.
Focal changes in the liver may be solitary or multiple. The echogenicity may vary from anechoic to hypoechoic to hyperechoic or may be mixed or complex and may have distinct or indistinct margins. Focal lesions contrast with the adjacent hepatic parenchyma. Focal lesions that can have variable echogenicity include benign nodular hyperplasia, hemorrhage, abscess, and neoplasia. Nodular hyperplasia is a benign lesion of decreased or increased echogenicity and is a common incidental finding. Focal changes may be seen with either metastatic or primary neoplastic infiltration, and they cannot be differentiated with certainty from benign lesions (Figure 2-8, I to P). Differential diagnosis should include hepatitis and cirrhosis. The so-called target sign, usually a hypoechoic rim surrounding a hyperechoic center, is produced by variations in tissue texture. It is the most consistent, but not a definitive, sign of neoplasia. The diagnosis of benign versus malignant neoplastic disease, or their differentiation from other focal lesions, requires fine-needle aspirate for cytologic evaluation or tissue core biopsy for histopathologic analysis. Fine-needle aspiration by ultrasonography permits the specific sampling of liver tissue and sequential examination of lesions for evaluation of treatment regimens (Figure 2-8, Q and R).
Hepatic cysts are usually anechoic, often congenital, and generally an incidental finding. Some cats with polycystic kidney disease may also have hepatic cysts. These may be single or multiple and are variable in size. The contents are usually anechoic, and the capsule is thin and cannot be distinguished from the liver parenchyma. Single large cysts can result in moderate or severe focal hepatic enlargement. Distal acoustic enhancement is a feature (see Figure 2-10, O).
Distention of the hepatic veins may be seen with hepatic venous congestion such as occurs in right-sided cardiac failure. The distended anechoic vessels are seen extending peripherally into the hepatic tissues (Figure 2-8, G and H). The main vessels are seen to drain into the caudal vena cava in the craniodorsal hilar region. This junction often looks like a rabbit’s ears. Focal hemorrhage in the liver parenchyma, when fresh, is usually echogenic and gradually changes to a hypoechoic area as the lesion regresses.
Abdominal arteriovenous fistulas have been described in dogs. There may be associated ascites. The fistulas are seen as large, anechoic, tortuous vessels. Doppler ultrasound is required to differentiate these from portosystemic shunts.