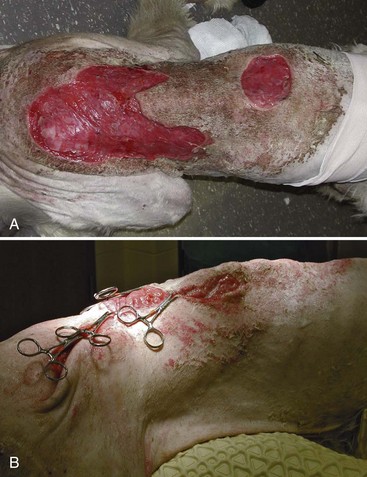
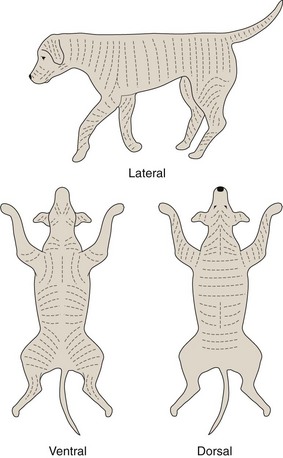
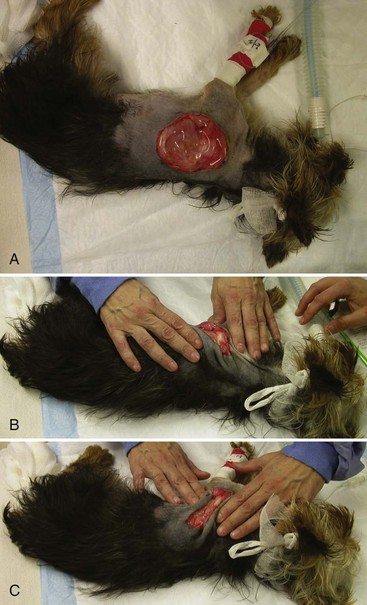
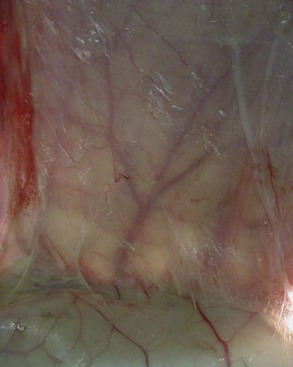
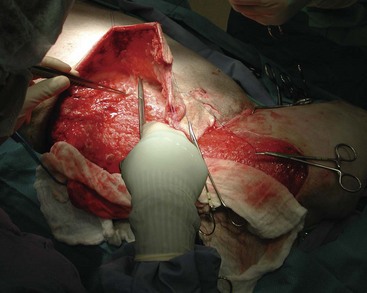
Chapter 77 One of the more satisfying outcomes a surgeon can experience is the successful reconstruction of a gaping wound that at first glance appears impossible to approximate. If, however, the surgeon fails to adequately address tension and shear forces and simply attempts closure at all costs, dehiscence will be inevitable (Figure 77-1). With some understanding of the biomechanical properties of skin and armed with a repertoire of reconstructive options, tissue ischemia and wound dehiscence from excessive tension can largely be avoided. This chapter discusses considerations for reconstructive surgery decision making, and describes techniques that can be used to distribute tension by mobilizing local skin without developing a flap or harvesting a free graft. 1. Obtain closure with minimal tension (i.e., to allow unimpeded wound healing). 2. Return function to the injured area (i.e., robust skin coverage, full range of motion). 3. Ensure that the final outcome is free of ongoing morbidity (i.e., pain-free). The reconstructive surgeon needs to practice meticulous technique, incorporating Halsted’s principles (Box 77-1) into his or her surgical consciousness. Instruments should be fine and sharp or atraumatic to reduce tissue damage. These include fine-toothed forceps (Bishop-Harmon, Brown-Adsons), DeBakey forceps, Metzenbaum scissors, Stevens tenotomy scissors, skin hooks, fine-tipped Mosquito hemostats, numerous fine-tipped Backhaus towel clamps for temporary skin positioning, bipolar or fine monopolar electrocautery, and sterile surgical skin marker pens. Using Allis tissue or Babcock forceps for mobilizing skin is not recommended because of the crush injury these instruments will inflict. In cutaneous reconstruction, the skin is often compromised from the initial injury or mobilization techniques, and rough handling exacerbates the damage. During lengthy procedures, skin is best handled by means of several strategically placed stay sutures or skin hooks. Open wounds should always be covered intraoperatively, usually with moistened surgical gauze, to minimize desiccating effects of the surgery lights (Figure 77-2). Wound factors of size, geometry, anatomic location, chronicity, wound-bed condition, and status of the peri-wound skin should all be taken into account when deciding how to mobilize tissues. Additionally, animal factors of the species; breed; body condition; age; temperament; and presence of any concurrent injuries, conditions, or medications that may alter wound healing should be considered. Finally, several owner factors such as likely compliance and commitment, financial capabilities, and importance of cosmesis need to be addressed. All of these wound, animal, and owner factors should be carefully scrutinized with respect to addressing the primary objectives listed previously and in light of the surgeon’s ability and experience (Table 77-1). Table • 77-1 Obtaining Closure Without Tension, Returning Function, and Ensuring a Pain-Free Outcome Upon preparing a patient for surgery, the surgeon should ensure that appropriate analgesia and nutritional intake are addressed. If prolonged inappetence has been experienced or is expected, the surgeon should consider feeding tube placement. This is especially appropriate for extensive wounds requiring staged debridement or reconstruction sessions. Preparation for surgery must include particularly generous clipping, skin preparation, and draping. The consequences of inadequate preparation in this regard will be the unwelcome appearance of hirsute skin into the operative site as the skin is mobilized. In addition to liberal skin preparation, the surgeon should strategically position the patient to maximize skin availability during surgery.9,21 This may involve temporary placement of towel clamps or sutures on wound edges to ensure that the available skin can be draped in appropriately (Figure 77-3). Leg ties should be loose (or nonexistent), and for axillary and inguinal wounds, the limbs should be free draped so that the reconstruction can be assessed through the full range of motion. A wound should never be closed by direct approximation of its edges if the resulting tension will lead to ischemia from pressure exerted by the sutures.13 This tenet holds true whether a wound is being closed by primary, delayed primary, or secondary closure. Necrosis of the skin adjacent to the sutures will invariably ensue followed by suture “cut-out,” and the subsequent wound dehiscence will be painfully evident.21,30 On extremity wounds, additional effects of excessive tension include the development of a “biologic tourniquet,” resulting in swelling, pain, and discoloration of the leg distal to the inappropriate closure (Figure 77-4). Skin tension is determined by the predominant pull of collagen and elastin fibers in dermal and hypodermal tissues. There are regional anatomic differences in the pliability of skin, thickness of the dermis, and degree of attachment between hypodermal elements and underlying fascia.2,22,33 Looser skin of the trunk, neck, cheeks, and top of the head is more easily mobilized than the tighter skin of the extremities. The dermis also becomes thinner and less well perfused as it ages, making geriatric skin more susceptible to ischemia and stress. Similar to the Langer lines developed for human plastic surgery, tension lines in the skin of an “average” dog have been described (Figure 77-5).11,24 Because of marked variability within the canine species, elasticity and amount of available skin vary with breed.29,30 In some breeds (e.g., Bassett hounds, beagles, retrievers), tension lines are not as critical, but in other breeds (e.g., sighthounds, Doberman Pinschers), they must be seriously considered (Figure 77-6). Tension lines in dogs, especially those with tighter skin, should be considered in two circumstances: when making an incision and when closing a defect.9,21,30 An effective and easy way of assessing the amount of tension likely to be induced by closure is to manipulate the wound in several directions, attempt to approximate the wound edges, and estimate whether the tension is within physiologic limits (Figure 77-7). Closing the wound parallel to tension lines generally places less tension on the sutures, minimizes puckers or “dog ears,” and reduces the incidence of a “biologic tourniquet.” In most cases, it is also the “easier” direction to close the wound. Occasionally, when a longitudinal laceration is across the line of inherent skin tension (which will cause it to gape considerably), it is easier and logical to simply approximate the wound along its long axis even though tension will be pulling the incision apart.30 In such situations, the anticipated additional stress on the incision can be addressed with some tension-relieving sutures. When making an incision in surgery, however, the direction of the cut should be parallel to the tension lines, thus allowing any tension on the final sutured incision to be aligned with the long axis of the incision rather than across it. In addition to tension, wound closures in highly mobile areas are subject to shear, where forces acting on one wound edge may oppose the forces acting on the apposed wound edge.30 Cyclic shear forces in wounds are especially evident in the axilla and inguinal area, over joints, and at the tail base and also apply to foot pad lacerations. Because of the wide range of motion of the jaw in dogs and cats, wounds adjacent to the commissure of the lips are also subject to significant shear. Even when there is no apparent tension pulling apart a closure, shear forces alone can ruin a fine reconstructive effort. When repairing wounds in these areas, the surgeon must not only address the shear forces internally by achieving a robust closure but also address the shear forces externally by immobilizing or protecting the area during the extended healing period. This is generally accomplished with a combination of external coaptation, confinement, and in cases of pad incisions, prohibiting weight bearing for several weeks. The inherent viscoelastic nature of skin imparts to it several properties: an initial pliability, a tendency to return to its original shape when deforming stress is removed, and an ability to adapt when prolonged stress is applied.20,22,35 The surgeon can turn the latter property to advantage when it comes to relieving tension on the primary suture line. The principles of mechanical creep, stress relaxation, and biologic creep arise from these properties (see Skin Stretching Techniques). Undermining involves the use of scissors or a scalpel to separate the skin from underlying tissue, usually through a distinct plane of dissection.8,9,21,25,30 On areas of the body that have a panniculus carnosus muscle (e.g., cutaneous trunci, platysma, sphincter colli superficialis), undermining should be performed deep to this muscle to preserve the deep subdermal plexus, which arborizes superficially to perfuse the dermis. The surgeon should also be aware of and try to preserve any perforating direct cutaneous vessels that supply the skin (Figure 77-8). When there is no panniculus muscle, the plane of dissection for undermining should be deep, just superficial to the muscle fascia (e.g., on the antebrachium) or even including a superficial layer of fascia (e.g., lateral thigh). The surgeon should always be conscious of preserving the deep subdermal plexus. Undermining draws upon the full elastic potential of the skin in the closure and forms the basis of numerous reconstructive efforts (Figure 77-9). Many wounds can be closed by use of undermining alone or with a combination of undermining and another tension-relieving procedure. It is critical that the peri-wound skin is sufficiently healthy and pliable with respect to blood supply, inflammation, and edema to be able to tolerate undermining and to reap the elastic benefits of the technique (Figure 77-10). If the peri-wound region is not in good condition, then reconstruction should be delayed until tissue conditions have improved. This layer of sutures can significantly reduce tension on the skin sutures and should always be used when there is likely to be motion or tension at the suture line.9 To ensure good holding power, bites should be taken in the more superficial, fibrous layer of the hypodermal tissues rather than in the fatty subcutaneous tissues. After satisfactory subcutaneous suturing, the skin edges should be almost touching, thus allowing finer skin sutures to provide apposition rather than tension relief (Figure 77-11). Subcutaneous sutures can be placed in an interrupted or continuous pattern. In high-risk areas (e.g., areas of high motion, multiple converging suture lines), interrupted sutures should be placed so that if partial dehiscence occurs, the remaining subcutaneous sutures will still hold. Placing interrupted subcutaneous sutures in a far–near–near–far, far–far–near–near, or cruciate pattern will provide superior tension relief compared with simple interrupted sutures.4
Tension-Relieving Techniques
Surgical Principles
Instrumentation
Decision Making and Planning
Factors
Considerations/Guidelines
Wound Factors
Size
<5 cm diameter
Direct closure or tension-relieving technique
5–10 cm diameter
Tension-relieving technique, skin flap
<10 cm diameter
Tension-relieving technique, skin flap, staged procedures, partial closure, second intention healing
Geometric Shape
Crescent, triangular, rectangular, circular
To avoid the formation of “dog ears,” see relevant text and figures in this chapter for closing variably shaped wounds
Anatomic Location
Trunk and neck
More amenable to tension-relieving technique or skin flap
Proximal limb; face
More amenable to flap development
Distal limb
More amenable to free graft or second intention, muscle flap
Chronicity
Acute or chronic
Assess integrity of blood supply to wound; assess quality of granulation tissue (bright red, purple, friable, exuberant, pale, or fibrous)
Bacterial Load
“Clean”, or “clean-contaminated”
Closure appropriate, drain placement if dead space
“Contaminated” or “Dirty”
Immediate closure not recommended unless vital structures exposed; active drain placement advised
Structural Damage
Severe soft tissue trauma can disrupt perfusion and negatively impact wound healing; ensure all devitalized tissue is debrided from the wound, and consider augmenting the blood supply with a reconstructive procedure
Peri-wound Status
Blood supply, edema/induration, inflammation
Delay reconstruction until peri-wound tissues are in healthy condition and suitable for manipulation
Patient Factors
Species
Dog, cat
More skin is generally available in cats, but extensive removal of their subcutaneous fat may slow healing
Breed
Tight skin, thin skin
Animals with tight skin and thin skin (e.g., greyhounds) require critical planning and nursing to avoid tension and pressure
Body Condition
Obese (BCS > 7/9)
Thin (BCS < 3/9)
Increased fat in the panniculus layer can challenge reconstruction. Minimize tension and movement in obese animals.
Age
Geriatric
May have less cutaneous perfusion, prolonged healing time
Temperament
Aggressive, boisterous
Ensure animal is an appropriate candidate for the proposed procedure
Systemic Factors
Malnutrition, organ failure, endocrinopathy
Underlying conditions may delay healing
Owner Factors
Commitment
Are owners prepared to manage animal in postoperative period?
Will compliance with instructions be an issue?
Financial
Provide realistic quotations, update frequently
Cosmesis
Assess how important final appearance is to the owner (e.g., show dog)
Surgeon Factors
Experience
Novice
Consult specialist with view to referral; consider taking continuing education course; practice on a cadaver or model
Intermediate
Consult texts and articles; practice on a cadaver or model
Experienced
Consult with other specialists; photograph and document challenging cases; think “outside the box”
Tension, Shear, and Viscoelasticity
Tension
Shear
Viscoelasticity
Techniques for Relieving Tension
Tension-Relieving Sutures
Strong Subcutaneous Sutures
< div class='tao-gold-member'>
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Tension-Relieving Techniques
Only gold members can continue reading. Log In or Register to continue