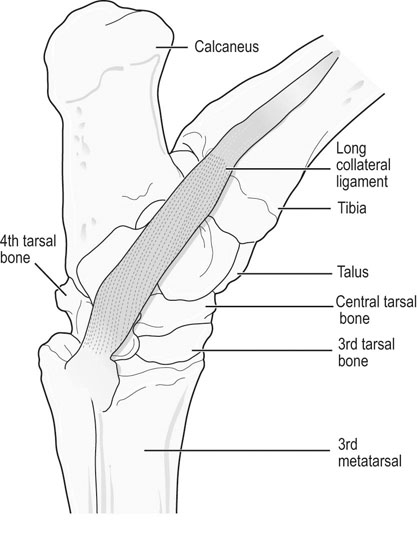
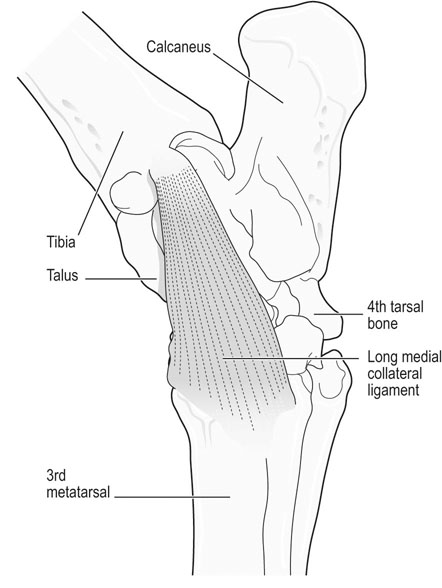
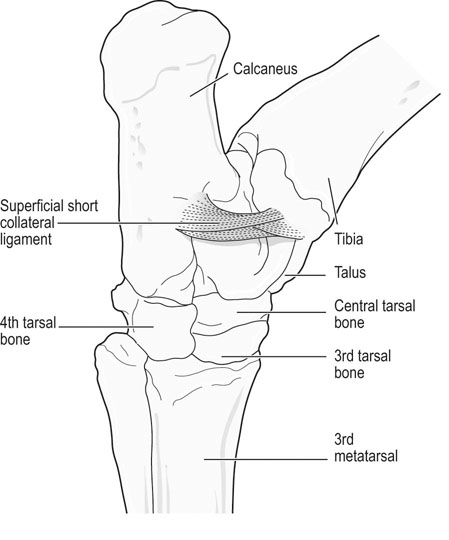
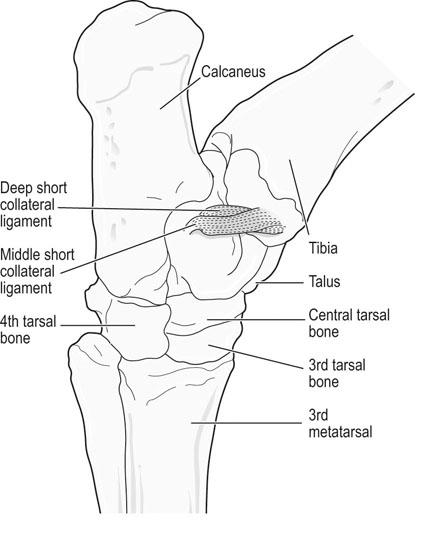
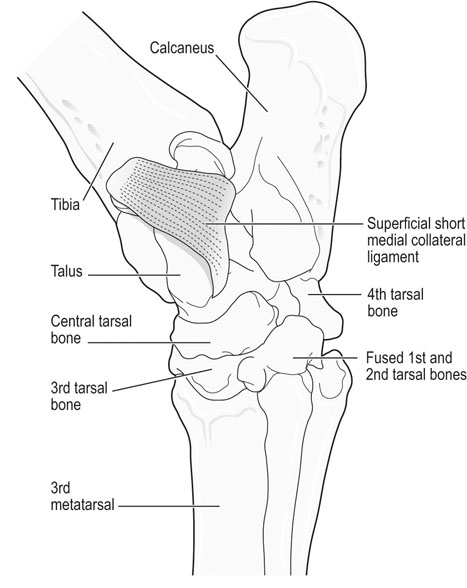
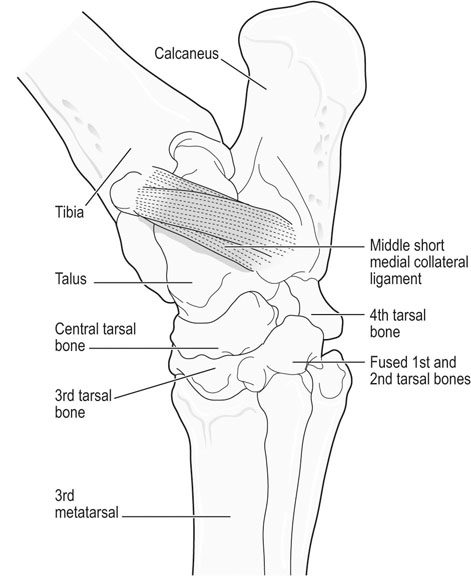
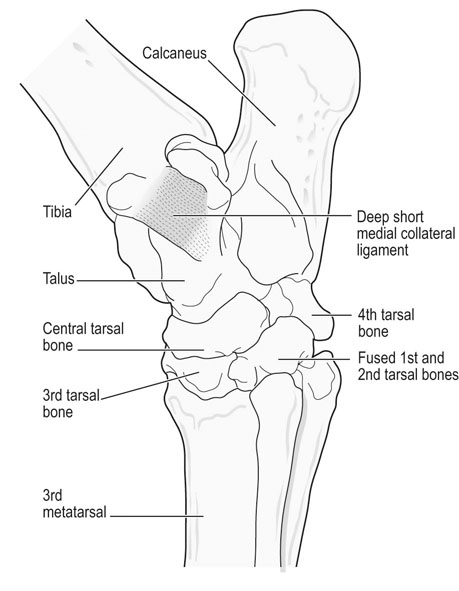
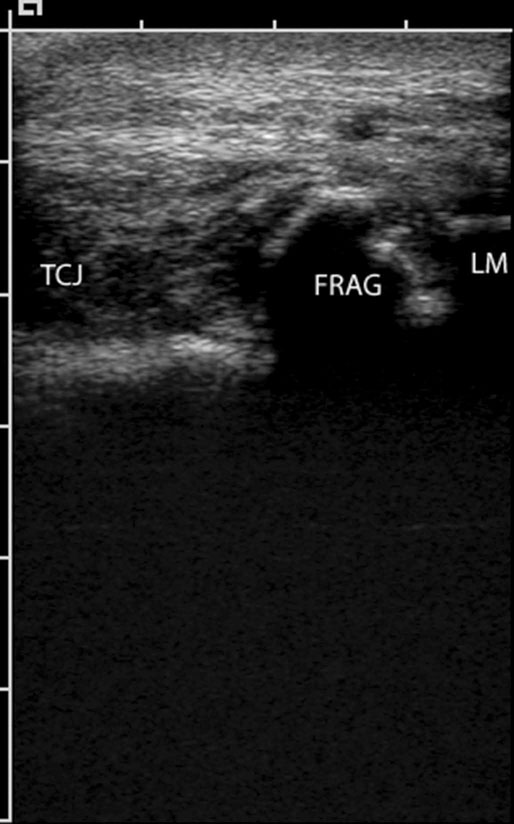
The equine tarsus has high-motion (tarsocrural) and low-motion (talocalcaneal, tarsometatarsal, centrodistal and talocalcaneal-centroquatral) joints. The distal tibia articulates with the medial and lateral trochlear ridges of the talus with its distal intermediate ridge lying within the trochlear groove in the tarsocrural joint (TC) (Fig. 19.1). This articulation provides for hock flexion and extension during locomotion. The proximoplantar aspect of the calcaneus projects plantar to the tibia and serves as the attachment of the gastrocnemius tendon (GT). The superficial digital flexor (SDF) tendon courses over the calcaneus on the plantar surface of the hock where it forms a fibrocartilagenous cap which has firm fascial attachments to the calcaneus to maintain its central position. The calcaneal and intertendinuous bursae surround these tendons at this level. The deep digital flexor (DDF) tendon lies within the tarsal sheath as it courses over the sustentaculum tali of the calcaneus. Distally, the talus and calcaneus articulate with the central tarsal bone and the proximal aspect of the fourth tarsal bone to form the talocalcaneal-centroquatral (proximal intertarsal, PIT) joint (Fig. 19.1). The central tarsal bone articulates distally with the third and fused first and second tarsal bones to form the centrodistal (distal intertarsal, DIT) joint. The tarsometatarsal joint (TMT) is the collective articulation of the fused first and second, third and fourth tarsal bones with the second, third and fourth metatarsal bones, respectively (Fig. 19.1). This complex bony arrangement is held together by complex collateral ligaments.1 The long lateral collateral ligament (CoL) originates proximally on the lateral tibial malleolus and courses distally to insert on to the calcaneus, fourth tarsal bone, talus and the fourth and third metacarpal bones (Fig. 19.1). The long lateral CoL is loose in flexion and taut during extension of the tarsus. There are three short lateral CoLs; the superficial, middle and deep ligaments (Fig. 19.2, Fig. 19.3). All originate proximally on the lateral tibial malleolus and insert distally on the calcaneus (superficial) and talus (middle and deep). The lateral short CoLs are variably tight or loose during flexion or extension of the tarsus. The medial long CoL originates proximally at the medial tibial malleolus and inserts distally on the fused first and second tarsal bones and on the talus, central and third tarsal bones by two separate fiber bundles (Fig. 19.4). It is loose during TC joint flexion and tight during extension. The short medial CoL is made up of the superficial, middle and deep short medial CoLs (Fig. 19.5, Fig. 19.6, Fig. 19.7). They originate proximally on the medial tibial malleolus and insert distally on the deep fascia, fibrous joint capsule, sustentaculum tali and central tarsal bone. The medial short CoLs are variably tight or loose during flexion or extension of the tarsus, with the majority of the deep component remaining tight during the entire range of motion of the TC joint.1 The TC joint communicates with the PIT joint in most horses. Communication between the DIT and TMT joints has been reported to occur in between 26% to 38% of horses when the TMT joint is injected first.2–4 Following the same injection, 34% of TMT joints would be expected to communicate with PIT and DIT joints.3,4 Increasing the volume or pressure of injection of liquid agents does not increase the probability of communication, but will increase the amount of subcutaneous leakage of fluid.2 The TMT and DIT joints may also communicate with the tarsal sheath, tendon of the tibialis cranialis and the subtarsal tissues near the origin of the suspensory ligament at the plantar surface of the third metacarpal bone.2,4 Due to this variable communication between synovial structures of the tarsus, intrasynovial anesthesia or medication of the DIT or TMT joint cannot be accurately predicted to affect more than a single compartment and may have an extrasynovial effect on the suspensory ligament, tarsal sheath or TC joint. Complete radiographic evaluation of the affected and contralateral tarsi should be performed where osteochondrosis is suspected. These include the dorsoplantar, lateromedial, dorsolateral-plantaromedial and dorsomedial-plantarolateral obliques and a flexed lateromedial view. Osteochondral lesions of the distal intermediate ridge of the tibia and lateral trochlear ridge of the talus are best observed on the dorsomedial plantarolateral view (Fig. 19.8 and Fig. 19.9). Medial malleolus lesions are more difficult to observe and can be obscured by the medial trochlear ridge.5 Angling a dorsoplantar view 10 degrees towards dorsolateral plantaromedial will help view the whole medial malleolus. Lesions of the distal intermediate ridge and medial malleolus of the tibia consist of variably sized osteochondral fragments still attached to the parent bone (Fig. 19.8). Lateral trochlear ridge lesions are usually lucent areas on the distal aspect of the ridge accompanied by overlying, variably sized osteochondral flaps (Fig. 19.9). The lesions can vary in size and depth and in some horses marked distal trochlear ridge osteochondral fragmentation may be the predominant radiographic finding. Horses may have radiographically inapparent osteochondral lesions of the trochlear ridges causing lameness and effusion. These may be imaged using ultrasound.6,7 Arthroscopic debridement of osteochondral lesions is recommended for most cases of osteochondrosis where there is TC swelling provided the lesions are mature. Arthroscopy will allow a more complete assessment of the affected area and identify lesions that are radiographically silent. Conservative therapy may be appropriate for yearlings prior to complete development of lesions or cases without swelling or lameness. The aim of treatment is to remove the involved tissue and debride the surrounding area of all loose and unattached cartilage.8 This will remove the stimulus for synovitis and minimize continued trauma to the affected area during high-speed exercise. In horses treated conservatively with rest or a reduction in the exercise schedule, the aim is to minimize disruption of the osteochondral lesion to allow healing by completion of endochondral ossification with increasing skeletal maturity or by fibrous attachment of the affected area to the parent bone.9 This will increase stability of the lesion and minimize the development and progression of synovitis. It is difficult to predict how long it will take for conservative therapy to work and how effectively the lesion is ossified or anchored, as radiographic monitoring will usually reveal persistence of the lesion. Return to high-speed exercise may cause a recrudescence of the lameness, necessitating surgical therapy or a more prolonged rest period.9 Approaches for arthroscopic surgery of the tarsus are well described.10 Bandaging and stall rest are continued for 2–3 weeks after surgery. Hand-walking can be started 10–14 days after surgery with limited turnout (paddock) initiated after 30–45 days, depending on the location of the osteochondrosis and extent of articular cartilage involvement. Horses with uncomplicated distal intermediate ridge lesions usually have a shorter convalescent time. Training is resumed after 90–120 days for most cases of TC osteochondrosis. Horses with extensive articular cartilage fibrillation or synovitis will usually benefit from an extended (5–6 months) interruption of strenuous activity. Single-dose intra-articular hyaluronic acid and corticosteroids may be beneficial in decreasing synovitis and reducing the catabolic effects of inflammation on the articular cartilage. The prognosis for horses with OC of the TC joint is excellent if there is a favorable response to either surgical or conservative treatment. Horses treated conservatively may be less likely to have a prolonged athletic career, but the performance is usually comparable to unaffected horses while they are actually competing.8 In young growing horses, lesions of the TC joint are less likely to spontaneously resolve than stifle lesions.11 Horses treated conservatively or surgically are likely to race as successfully as unaffected horses of the same age, breed and use.8,12 The size of the lesion or resolution of the effusion after surgery do not appear to be as reliable prognostic indicators for horses that undergo arthroscopic surgery for osteochondrosis of the distal intermediate ridge or medial malleolus of the tibia or the lateral trochlear ridge of the talus. Horses that have erosive articular cartilage lesions at the time of surgery have a guarded prognosis for athletic soundness. Osteochondrosis is a multifactorial disease so complete prevention is unlikely.11 Genetic selection away from breeding lines predisposed to osteochondrosis is controversial because superior racing stock in some breeds may have a genetic predisposition for the disease. In cases of TC osteochondrosis, the prognosis for racing performance with treatment is good, making removal of these animals from the breeding pool unrealistic. Osteochondrosis is a developmental disease characterized by disorders of the growing cartilage in the epiphysis and growth plates. The disease is multifactorial with genetic, nutritional (copper deficiency or zinc excess, calcium and phosphorus imbalance from feeding excess grain), metabolic (vitamin D deficiency) and endocrine (hypothyroidism) influences.11,13–15 The predictable locations of many osteochondral articular lesions in the horse are sites where the developing articular cartilage or growth plates are thick, the vascular supply is tenuous and the biomechanical loads are high. Therefore, vascular and traumatic insults in these locations are probably very important in the expression of this disease in horses.14,16,17 The ultimate expression of the disease is unpredictable but controlling some of these factors may help reduce the incidence of the disease in a particular area or farm. Athletes with tarsal CoL injuries will present with a rear limb lameness of variable severity that worsens with exercise and can usually be markedly exacerbated by upper limb flexion.18 There may be palpable swelling, thickening and pain of the soft tissues surrounding the affected structure. Effusion of the TC joint or tarsal sheath may be obvious. TC joint effusion has been reported as a consistent finding in Standardbred pacers with long CoL injuries.18 Horses with TC luxations will have marked periarticular swelling, crepitus and an obvious angular (valgus or varus) and rotational deformity of the tarsus at presentation.19,20 Open tarsal luxations usually involve the synovial cavity of the affected joint and the articular cartilage can often be visualized through the wound. The limb should be carefully evaluated for concomitant structure involvement before proceeding with attempts at reduction and stabilization as the prognosis worsens with extensive soft tissue damage. Horses with intertarsal or TMT luxations may also present with an open wound, which makes the diagnosis straightforward. In horses with desmitis of the CoL tarsal radiographs may reveal enthesiophytes at the attachments of the CoL to the parent bone.18 There may be dystrophic mineralization of the tissue evident in chronic cases and degenerative joint disease or collapse of the joint space(s) if there is long-standing instability present due to the CoL injury. Tarsal radiographs of horses with intertarsal or TMT luxations may reveal a widened joint space dorsally at the affected site during the acute phase (Fig. 19.10). If the radiographs are taken with the foot on the ground or the soft tissue swelling has stabilized the joint (luxation is reduced), the radiographic diagnosis may not be obvious. Therefore, a stressed lateromedial radiographic view is recommended to identify this injury. The foot is lifted slightly off the ground by an assistant and pulled in a plantar direction to open the affected articulation dorsally and obtain an adequate image of the luxation (Fig. 19.10). The patient will often resent this manipulation, necessitating adequate restraint (sedation and/or lip chain). The CoLs of the tarsus are easily accessible for ultrasonography. Their structure is complex making interpretation challenging but disruptions of the long components of the medial or lateral CoL are more readily diagnosed.21–23 Collateral ligament injury is often associated with other soft tissue injuries of the tarsus so a complete ultrasound investigation of the area is important.22 In horses with desmitis of the CoL tarsal radiographs may reveal enthesiophytes at the attachments of the CoL to the parent bone.18,24 There may be dystrophic mineralization of the tissue evident in chronic cases and degenerative joint disease or collapse of the joint space(s) if there is long-standing instability present. The more superficial areas of the short portions of the CoLs and long plantar ligament can be adequately imaged.21,22 Ultrasonographically there will be disruption of the fiber pattern, hypoechoic fluid accumulation within the ligament or hyperechoic deposition of fibrous or mineralized soft tissue, depending on the stage and extent of the injury. Pronounced periarticular soft tissue swelling may interfere with ultrasonographic imaging of these structures. Perineural analgesia of the peroneal and tibial nerve should improve most lameness associated with CoL injuries of the tarsus. Nuclear scintigraphy in horses with tarsal CoL injuries will reveal a pattern of increased radioisotope uptake at the attachment of the CoL to the bone.18 The pattern of uptake and its location will help identify the structure involved (long versus short CoL) and the degree of involvement (single versus multiple areas).18 Scintigraphy is especially useful in horses with a subtle lameness localized to the hock where radiographic studies are inconclusive. Magnetic resonance imaging would be ideally suited for the diagnosis of CoL injuries of the tarsus in horses.25,26 Horses with desmitis of the CoL need to be rested to allow the collagen in the ligament to be replaced and to organize along the lines of stress. Affected horses should have stall rest for the first 14–21 days after the injury, with a gradual resumption of hand-walking only (5–10 minutes twice a day) after that time. Systemic NSAID therapy, cold compresses or hydrotherapy and leg wraps are helpful in eliminating soft tissue swelling and restoring adequate circulation to the injured area. Continued activity with further ligament disruption will generate a pronounced fibrovascular response that will eventually fibrose in a disorganized manner, resulting in an architecturally weakened structure with little elasticity and poor function. This will interfere with joint movement and create a persistent mechanical or painful disruption of the gait.18 These horses should be monitored ultrasonographically and with nuclear scintigraphy during their convalescence to evaluate ligament healing. Exercise intensity can be gradually increased when there is a significant reduction in the size of the original injury and increased tissue organization. This usually requires 3–6 months of rest. Swimming these patients may be beneficial before starting flat work to increase the strength of the tissues without loading them. Patients with CoL injuries can return to full athletic use if these injuries are diagnosed early, treated aggressively and rehabilitated properly. Standardbred pacers have a good prognosis for racing as well or better after diagnosis (scintigraphy) and treatment (rest) of long CoL injuries. However, horses with extensive disruption that involves most of the cross or longitudinal section of the ligament(s) will usually not be able to return to rigorous athletic use, especially if mineralization or osteophyte production eventually interferes with joint function.18 Depending on the inciting cause, location and size of the fracture, there will be a sudden onset of a moderate to severe lameness following a traumatic episode (fall, kick or collision) or high-speed exercise.27 The location and size of the fracture will determine the degree and location of any observed synovial effusion or periarticular swelling. Horses with the more common non-displaced fractures of the tarsus will usually exhibit a significant improvement in the degree of lameness at a walk or slow jog within a few days of the injury. Horses treated with NSAIDs may show an even more dramatic improvement while on the medication. A persistent draining tract may be present when the original trauma results in a break in the skin over the affected bone. There is usually some degree of soft tissue swelling, pain and crepitus localized over the area of the fracture. Horses with slab fractures of the central or third tarsal bone are usually very lame immediately after the injury, but improve considerably after a few days.28,29 There is minimal swelling, crepitus or effusion associated with third tarsal bone fractures at presentation, but there may be effusion of the TC joint in horses with central tarsal bone fractures.29 A painful response can often be elicited by deep palpation over the cranial or lateral surface of the affected joint.29 Horses with fractures of the calcaneus will usually present with effusion of the tarsal sheath and/or calcaneal bursa. There may be a wound near the calcaneus that can discharge clear synovial fluid or purulent material. The degree of lameness is variable depending on the location of the injury. Horses with osteomyelitis of the calcaneus, sustentaculum tali and/or sepsis of the tarsal sheath are usually very lame.30 Lateral malleolus fractures are readily seen on the dorsoplantar radiographs (Fig. 19.11).27,31 Oblique views may assist in determining whether the fragment is dorsal or plantar (Fig. 19.12). Ultrasound examination will also be helpful in locating the exact position of the fragment which is important for surgical planning (Fig. 19.13). The fragments are variably sized and the degree of surrounding osseous reaction is an indicator of duration. Most slab fractures of the third or central tarsal bone are located in a frontal plane or on the craniolateral edge of the bone. Therefore, they are best imaged on the lateromedial or dorsomedial to plantarolateral oblique radiographic views.28,29 Most are non-displaced and there is minimal dorsal or medial distraction of the slab. For this reason they may be difficult to observe with radiography.32 They can be 4–8 mm thick and variably wide.29 Fragmentation of the calcaneus or sustentaculum tali can be difficult to image on conventional radiographic views if they are small and located on the dorsal, distal or axial surface of the bone. Those on the proximal, caudal and lateral surfaces are easier to identify on conventional views. If axial or distal fragmentation of the calcaneus is suspected or there is distension of the tarsal sheath associated with a wound, a skyline (dorsoplantar to distoplantar) view of the plantar aspect of the tarsus should be obtained. Radiographically there may be marked lysis of the calcaneus or sustentaculum tali associated with bony fragments in horses with osteomyelitis and/or sequestrum formation (Fig. 19.14). Transverse fractures of the calcaneus are readily apparent on the lateromedial and oblique radiographic projections. These fractures are rare and will have a similar presentation to a horse with disruption of the reciprocal apparatus (dropped hock and hyperflexion of the limb during attempts at weight bearing). Ultrasound may be helpful to determine synovial cavity involvement in traumatic injuries to this area. The calcaneal bursa and tarsal sheath should be carefully examined for evidence of synovial thickening, intra-synovial gas or foreign bodies and echongenic material within the synovial space. Osseous disruption of the talus can usually be seen on the conventional views of the tarsus. Large fractures are readily apparent, but distomedial fragments may be visible only on a skyline view of the plantar tarsus and there will be bony lysis when a septic process accompanies the injury within the tarsal sheath. Fractures affecting the trochlear ridges of the talus may be small and located distally on the ridge(s) or groove or they can involve a large portion of the articular surface with marked joint instability, pain and effusion (Fig. 19.15). Sagittal fractures of the talus can be difficult to observe and multiple of dorsoplantar views may be required to highlight the fracture line (Fig. 19.16). Scintigraphy will identify the site of the fracture if one is suspected (Fig. 19.17). Slab fractures of the third or central tarsal bone in racehorses can be managed both conservatively or with lag screw fixation.29,33 Horses treated conservatively (stall rest) may develop osteoarthritis of the affected joint however many can successfully return to racing. This appears to be more common with third than with central tarsal bone fractures.28,33–35 Standardbred racehorses tend to have a better prognosis for a return to racing following conservative treatment than Thoroughbred racehorses.35 The surgical technique requires general anesthesia and radiographic or fluoroscopic guidance for proper drill and screw placement.29 These fractures can usually be repaired with a single 3.5 or 4.5 mm cortical screw or a cannulated screw system. The head of the cortical screw is usually not countersunk to reduce the probability of the fragment shattering when the implant is tightened. An incision over the affected joint to identify the center of the fragment and proximal and distal margins of the joint for proper screw placement will expedite surgery. It should minimize the risk of damage to the dorsal tarsal vessels that can occur when the surgery is done with needle guidance through stab incisions. The horses are assisted during recovery and confined to a stall for 4–6 weeks. Gradual introduction to hand-walking can begin at that time and return to training can occur 4–8 months after repair. Radiographic evaluation may be the best guide for increasing activity levels. Lateral malleolus fractures should be treated surgically, especially in horses with synovial effusion and lameness.27,31 Arthroscopic visualization will allow a thorough evaluation of the entire joint to assess the articular surface for damage, look for and remove any loose osteochondral fragments, inspect the fractured malleolus and flush debris out of the joint. The fracture fragment(s) can be removed arthroscopically, although this is a challenging procedure for large fragments that require extensive dissection of the short collateral ligaments.27 Dorsal and plantar portals are often required. Alternatively, the fragment can be removed quickly and effectively through a dorsal arthrotomy centered over the fragment.31 Careful dissection will prevent further damage to the long lateral CoL. If the fragment is large enough, where a considerable portion of the attachment of the long lateral CoL is involved, reduction and fixation with a lag screw (4.5 or 5.5 mm cortical screw) will be necessary. Removing these large fragments will cause further damage to the CoL and would perpetuate TC instability. Assisted recovery should be used with these horses to limit further damage to the CoL and avoid tarsal luxation and a short cast may be applied for recovery. Postoperatively, the limb is kept bandaged for 2–4 weeks to control swelling and reduce the effusion. In some horses, a residual amount of effusion will remain that appears to be inconsequential to future performance. Hand-walking can be initiated at 2–3 weeks after surgery and turnout in 4–6 weeks. Training can resume in 90–120 days depending on the resolution of the majority of the effusion and lameness and the degree of pre-existing damage to the long lateral CoL. If a lag screw fixation was performed, 6–8 months of rest will be required before resuming exercise to insure healing of the malleolus and CoL. Radiographs can be used to assess bony healing. Fractures of the calcaneus can be treated conservatively or surgically. Fragmentation of the calcaneus or sustentaculum tali is usually accompanied by a soft tissue defect over the lesion and/or marked effusion of the tarsal sheath. Secondary sepsis of the tissue will be manifested as osteomyelitis of the calcaneus and/or sepsis of the tarsal sheath or calcaneal bursa, depending on the location of the wound or bony lesion.30,36,37 Arthroscopic exploration of the calcaneal and intertendinous bursae or the tarsal sheath allows surgical debridement of fracture fragments and necrotic bone and any associated tendon injury and lavage.38–40 Systemic and local administration of appropriate antibiotic based on culture and sensitivity results should be continued post surgery. When trying to salvage a horse for breeding, a midtarsal tenotomy or tenectomy of the DDF will decrease motion of the tendon within the sheath, reducing pain and remove infected tendon tissue.30 Due to the low numbers of many types of tarsal fractures reported, establishing a prognosis is challenging. A thorough assessment of the ligamentous, synovial cavity, articular and bony involvement is important. Horses with extensive damage to the CoL, SDF, fibrous joint capsule or articular cartilage have a poor prognosis for athletic use, even if a surgical procedure successfully removed fragmentation, secured loose fractures or resolved sepsis. Horses with fragmentation of the dorsodistal or very plantar aspect of the trochlear ridges, and fractures of the lateral malleolus, have a good prognosis for return to function with proper therapy. Standardbred racehorses with slab fractures of the third tarsal bone treated surgically or conservatively appear to have a good prognosis for return to racing but the prognosis of Thoroughbred racehorses is not so good when treated conservatively.35 Horses with more complex injuries (transverse calcaneal or complete talus fractures) have a poor prospect for returning to high-level athletic activity. Bone injuries with secondary synovial sepsis carry a guarded prognosis.37,38,41 Aggressive treatment may salvage affected horses for non-athletic purposes. A rapid return of synovial fluid variables to normal levels suggests a better prognosis than those where they remain high at days 4–6.41 Thoroughbred or other performance horses that have a wedge-shaped conformation of the craniolateral aspect of the third tarsal bone may be predisposed to sustaining a slab fracture of this bone during high-speed training or racing, by presumably concentrating compressive forces along the trough in the wedge.42 Diagnostic analgesia is required in most cases to localize pain to the distal tarsus. Regional anesthesia involves performing tibial and peroneal nerve blocks following desensitization of the lower limb and proximal plantar metatarsus. This is not specific for the distal tarsal joints, however most problems of the larger synovial structures of the tarsus will result in easily identified effusion. The horse should be examined at 20 minutes post injection and further blocks should be delayed for one hour as sometimes the response is delayed. Intra-articular anesthesia of the distal tarsal joints is also not specific due to variable communications with a number of other structures but does localize pain to the region. The TMT and DIT joints communicate in approximately 26–35% of horses and anesthetic can also diffuse into the tarsal sheath or proximal intertarsal or TC joint after injection into the TMT joint space.2–4 The proximal palmar metatarsus should be blocked prior to a TMT block because the plantar distal extensions of the synovial cavity run either side of the proximal suspensory ligament.4 In cases with severe radiographic changes the response to intra-articular analgesia may be poor. Radiographs are difficult to interpret in isolation because many horses have mild radiographic changes where pain cannot be localized to the distal tarsal joints, whereas some horses with significant pain localized to this area have normal radiographs.43 Based on MRI findings, radiography is unreliable for the detection of subchondral bone lesions, subchondral bone sclerosis and even fractures of the tarsal bones.32 Radiographic changes that may be observed in association with osteoarthritis of the small tarsal joints include loss of joint space, periarticular osteophyte and enthesiophyte production and/or subchondral bone lysis (Fig. 19.18, Fig. 19.19). The disease may be localized to either the dorsomedial or the dorsolateral aspect of the joint(s). The radiographic changes, when present, are consistently seen on the lateromedial and dorsolateral to plantaromedial oblique projections. Horses with degenerative joint disease of the TCa joint will have radiographic evidence of bony lysis and sclerosis at the normally smooth contour of the articulation between the talus and calcaneus. Scintigraphy is useful to determine if subchondral bone is actively modeling or remodeling. In a high proportion of horses with distal tarsal joint pain, there is a loss of the normal pattern of uptake of radioisotope44 and lesions detected with MRI can be identified with scintigraphy, albeit with less anatomical detail32 (Fig. 19.20). It is important to note that the normal scintigraphic pattern is different for different breeds and disciplines.45,46
Tarsus and stifle
Tarsus
Anatomy
Osteochondrosis
Recognition
Imaging


Treatment and prognosis
Treatment
Prognosis
Prevention
Etiology and pathophysiology
Collateral ligament injuries
Recognition
Physical examination
Imaging

Treatment and prognosis
Treatment
Prognosis
Tarsal fractures or osteitis of the calcaneus or talus
Recognition
Presentation
Physical examination
Imaging





Treatment and prognosis
Treatment
Prognosis
Etiology and pathophysiology
Osteoarthritis
Recognition
Physical examination
Imaging


![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree