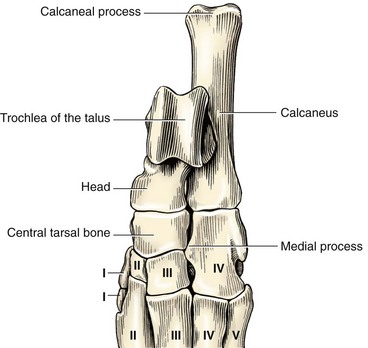
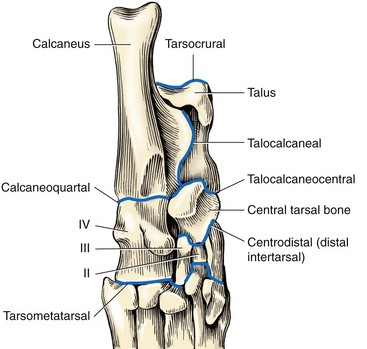
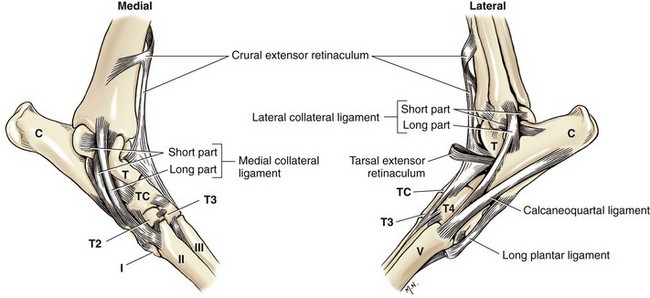
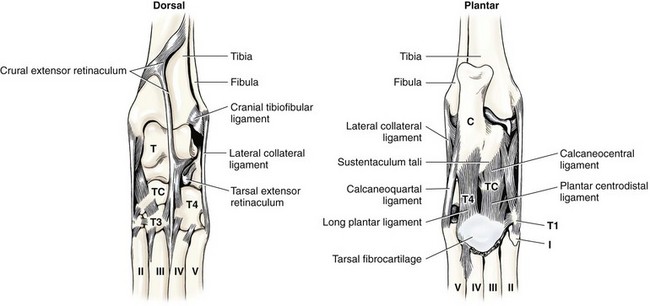
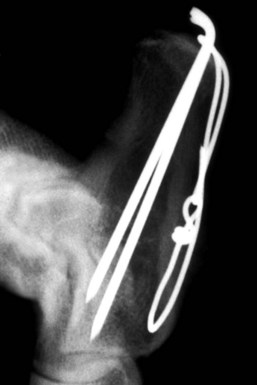
Chapter 64 The tarsus (hock) consists of the tarsal bones and joints between the crus and the metatarsus.20a It is a complex joint, so many varied injuries can occur. As with injuries involving the carpus, many descriptive reports have been published, but large case studies detailing conditions in this area are few. This may reflect the frequency of occurrence at individual centers. Therefore, this joint remains a clinical challenge. This chapter will focus on major injuries that affect the tarsus. Fractures are addressed using standard fixation techniques; fractures peculiar to this area will be described and fixation methods identified. Luxations and subluxations are important conditions affecting the joints, as are other injuries to adjacent or intrinsic ligaments and tendons. An effort will be made to identify key injuries to this area and to detail their clinical presentation, management, and outcome. Fractures of the metatarsal bones are very similar to those seen in the metacarpus; see Chapter 56 for details of management. The tarsus is a composite joint of the seven tarsal bones held together by a variety of ligaments (Figure 64-1). The fibrous component of the joint capsule forms a sleeve extending from the distal tibia and attaching at the proximal metatarsus. This supporting sleeve contains all of the tarsal ligaments and is much stronger and better developed on the plantar surface than on the dorsal aspect. This complex ligamentous support is critically important to the normal function of the joint. Many injuries to this area involve the soft tissue supports and result from spontaneous overstress rather than from direct injury from outside forces. The tarsus is more than three times longer in span than the carpus63 and is subject to propulsive forces generated by the hindlimbs; these are offered as likely reasons for its observed susceptibility to overstress injury. Seven individual bones are members of the complete tarsal joint: the talus (tibial tarsal bone); the calcaneus (fibular tarsal bone); the central tarsal bone; the fourth tarsal bone; and the first, second, and third tarsal bones (see Figure 64-1). These bones form three irregular rows, with the talus and calcaneus located on the proximal row, and the other bones on the distal rows. The talus is the only bone that forms an articulation with the tibia and fibula. It is located medially and has the most complex structure of all the tarsal bones. The talus is made up of three parts: the body, the head, and the connecting neck. In the body of the bone, the two ridges formed by the trochlea of the talus articulate with the corresponding cochlea of the tibia. A 25 degree lateral deviation is seen from the sagittal plane, produced by this articulation and allowing the hindlimbs to pass lateral to the forelimbs when the animal gallops.63 The head articulates with the central tarsal bone. The calcaneus, the largest of the tarsal bones, forms articulations with the talus and the fourth tarsal bone, and has a small articulation with the central tarsal bone. The articulation with the talus is extremely stable, with the two bones almost morticed together. The proximal part of the bone, the tuber calcanei, provides attachment for the common calcanean tendon. On the medial side of the bone is a bony process, the sustentaculum tali. The medially placed central tarsal bone articulates with all of the other tarsal bones and acts as a buttress support for the joint.12 The larger fourth tarsal bone spans the central portion of the joint laterally, forming articulations on the medial surface with the central and third tarsal bones. It articulates proximally with the calcaneus and distally with the fourth and fifth metatarsal bones. The metatarsal bones are numbered I to V from medial to lateral, and all are anatomically similar, with the exception of metatarsal I (dew claw). Sesamoid bones sometimes are present at the level of the tarsometatarsal joint in the Greyhound breed, with a lateral plantar tarsometatarsal sesamoid reported in 50%, and a small medial intertarsal tarsometatarsal sesamoid in 27%.67 The entire joint functions as a ginglymus (hinge joint), with the majority of movement (90%) expressed only at the tarsocrural articulation. Six main articulations have been identified: tarsocrural31a (also referred to as talocrural20a), talocalcaneal, talocalcaneocentral, calcaneoquartal, centrodistal, and tarsometatarsal (Figure 64-2). The talocalcaneocentral and calcaneoquartal joints are collectively referred to as the proximal intertarsal joint. The centrodistal joint, also known as the distal intertarsal joint, is the articulation between the central tarsal bone and the first, second, and third tarsal bones. The articulations between the numbered tarsal bones and the metatarsal bones comprise the tarsometatarsal joints. The fibrous component of the tarsal joint capsule extends from the distal tibia to the proximal ends of the metatarsal bones and contains within it the soft tissue structural elements of the tarsal joints. As in the carpus, the fibrous capsule is attached to many of the individual tarsal bones as it passes over them. Thickenings are found on the dorsal and plantar aspects. The thickened plantar fascia is divided to form the tarsal canal, which lies medial to the calcaneus and plantar to the talus. This canal contains several important structures, including the tendon sheath of the flexor hallucis longus muscle, the plantar branches of the saphenous artery and vein, and the medial and lateral plantar nerves. Lateral and medial support is provided by the lateral (fibular) and medial (tibial) collateral ligaments, respectively. The medial collateral ligament is a complex of three distinct ligaments that combine to provide support.2 The most superficial of these forms a band running from the medial malleolus to the first tarsal bone, but it also forms attachments to the central tarsal bone (firm), the talus (tenuous), and the second tarsal bone (tenuous). This is the long part of the ligament; it becomes tight in extension and is loose in flexion. The short part of the medial collateral ligament consists of two distinct parts: the tibiocentral and tibiotalar portions. The tibiocentral portion is taut in extension and loose in flexion, as is the long portion. However, the tibiotarsal portion runs at 90 degrees to the other parts and is tight in flexion but loose in extension. It is also the most substantial component of the medial collateral ligament (Figure 64-3). The plantar ligaments, which are also important stabilizers, have three major components (Figure 64-4). The middle plantar ligament runs from the base of the calcaneus to the fourth tarsal bone and then to metatarsal bones IV and V. The medial plantar ligament attaches proximally to the sustentaculum tali, passes over and attaches to the central tarsal bone, and attaches distally to the tarsometatarsal joint capsule. Finally, the lateral plantar ligament leaves the caudal surface of the calcaneus and unites with the long collateral before attaching to the base of metatarsal bone V. Small avulsion fractures can arise with detachment of these ligaments. Innervation is supplied by two branches of the sciatic nerve; the tibial nerve, which divides just proximal to the tarsocrural joint to become the medial and lateral plantar nerves, and, the common peroneal nerve, which divides into the superficial and deep peroneal nerves. The saphenous nerve, a branch of the femoral nerve, provides cutaneous innervations to the dorsomedial part of the tarsus and metatarsus.20a Careful and thorough physical examination is necessary because of the many different problems that may affect the tarsus. Some conditions affect the standing angle of the joint during weight bearing. Careful attention should be paid to this angle, which is normally 135 to 145 degrees in dogs and 115 to 125 degrees in cats.52 Consideration should be given to both the actual angle and any differences in symmetry that exist between the hindlimbs. Observation and palpation for swelling and/or pain may localize an injury, because the bones have only sparse soft tissue cover in this area. Many of the injuries encountered result in instability; therefore, careful and systematic checks for palpable instability are carried out with the joints stressed in mediolateral, dorsoplantar, and rotatory planes. This examination should be repeated when the animal is sedated or anesthetized. The range of movement of the tarsocrural joint should be assessed and is typically 39 degrees in flexion to 164 degrees in extension in the normal canine joint32; a greater range of 22 degrees (flexion) to 167 degrees (extension) is found in the cat.34 Any difference between movement observed during conscious examination and values obtained when the animal is sedated or anesthetized may indicate guarding of the joint due to pain.32 Establishing the site of pain, swelling, and instability greatly assists identification of the injury with imaging techniques. Fractures of the talus are rare but can involve the head, neck, or body of the bone (Figure 64-5). Fractures through the body can involve the articular surface and require surgical reduction and stabilization. The prognosis is generally guarded. Fractures of the articular surface, not unlike osteochondral fragments, can affect the lateral or medial trochlear ridges. Reattachment of the fragment should be attempted and can be accomplished with Kirschner wires, small screws that are countersunk, or biodegradable rods.13 Good surgical exposure is necessary to allow accurate reduction of the fragment, and osteotomy of the medial malleolus may be required to repair fractures of the medial ridge, or osteotomy of the fibula to give access to the lateral ridge. A caudal approach has also been described.18 Fractures may occur through the neck and head. Surgical stabilization using small lag screws has been advocated,14 but this can be difficult to achieve because of the shape of the bone. The author has successfully treated five cats by traction and external splint stabilization using a medially located unilateral transarticular external skeletal fixator (Figure 64-6).40 This obviated the need for open reduction, provided good reduction using traction to align the bone, and allowed early weight bearing. All fractures healed uneventfully, and the external skeletal fixators were removed at 8 weeks.40 Fractures of the calcaneus are functionally debilitating as they affect the function of the common calcanean tendon apparatus. Fractures most often are seen in working dogs, notably the racing Greyhound,12 but can occur sporadically in other nonworking breeds. Four patterns of fracture have been recognized, namely, midshaft fractures (Figure 64-7), slab fractures located dorsomedially or laterally, avulsion fractures involving the plantar ligaments from the base of the bone, and, rarely, Salter-Harris I fractures associated with avulsion of the proximal epiphysis.30 In racing Greyhounds, the calcaneus of the right tarsus is much more likely to be involved, and this fracture is commonly associated with a concurrent central tarsal bone fracture. It has been proposed that the central tarsal bone fractures first, and the resultant loss of stability exposes the calcaneus to muscular forces, resulting in midbody and slab fractures.50 Fracture of the base of the bone with avulsion of the plantar ligaments is not commonly associated with other fractures. This produces instability at the level of the proximal intertarsal articulations and can result in subluxation at this level and deformity or a pseudo-plantigrade stance. Identification of fracture is dependent on careful clinical palpation in the conscious and sedated or anesthetized dog, and on good quality radiographs to show the individual fracture type. Stress views are extremely useful in characterizing plantar avulsion fractures.12 Treatment is dependent on surgical stabilization of both the concomitant central tarsal bone fracture and the calcaneus. Small lag screws and Kirschner wires can be used to reassemble slabs or comminuted fragments. Midshaft fractures can be stabilized using a pin and a tension band wire (Figure 64-8).14 Care should be exercised in placing Kirschner wires, which should be inserted in a plantarolateral and plantaromedial location, to minimize interference with the digital flexor tendons. It has also been suggested that a tension band wire should be introduced under the flexor tendons to engage the Kirschner wires, which are bent to lay as close to the bone as possible to avoid irritation of the tendons.52 Alternatively, a laterally placed bone plate can be used. Veterinary cuttable plates are particularly useful for this purpose and are especially valuable in comminuted fractures.53 Prognosis can be good, but this depends on concomitant fractures and the results of surgery.13 Avulsion fractures of the sustentaculum tali and plantar apparatus generally are treated by arthrodesis of the joint. Prognosis is good for functional return but poor for a return to racing.30 Fracture of the central tarsal bone occurs almost exclusively in the racing Greyhound and usually affects the right tarsus (leg toward the outside of the racing track), but it can occur in other breeds as well.29 The author has identified the same injury affecting the left tarsus in a coursing dog. Fractures of the central tarsal bone accounted for 79% of all tarsal injuries in a survey on racing Greyhound injuries.27 Loss of the stabilizing buttress effect of the central tarsal bone allows collapse and hyperextension of the joint. This can commonly lead to concomitant fractures; the fourth tarsal bone and the calcaneus are most often affected.6 Five different patterns of central tarsal bone fracture have been recognized and classified. • Type I: nondisplaced dorsal slab fracture • Type II: displaced dorsal slab fracture • Type III: large displaced medial fragment • Type IV: medial slab fracture with a dorsal slab fracture Type IV with a medial fracture and a dorsal slab is the most common type of fracture. Type IV and V injuries account for 75% of all central tarsal bone fractures.6 Displacement of the medial fragment allows the joint to collapse; this places additional strain on the other tarsal bones. In type I and type II fractures, this collapse usually does not occur. This can present some challenges in diagnosis. Careful clinical assessment and good quality radiographs are essential to prevent these fractures from being missed (Figure 64-9). Type III is the rarest type. Early diagnosis and surgical stabilization using lag screws is the optimum treatment for types I through IV.7 The dorsal slab has an articular component; therefore stable fixation will yield the best result. In types III and IV, the medially displaced component must be restored and held firmly in position to prevent collapse of the joint. In type IV fractures, both main components should be reduced and held in position before insertion of the lag screws, with the medial screw inserted first. In all cases, care must be taken in selecting and inserting the screw to ensure that the small slab fragments are not fractured iatrogenically, and to avoid inserting screws into the joint spaces. Clearly, any concomitant fractures require concurrent management. Fracture dislocation of the central tarsal bone has been described in six Border Collies.26 This injury does not fit into the traditional classification, and it is suggested that it has been described previously as a dislocation of the central tarsal bone.39 Dislocation is associated with fracture of the plantar process; this fracture was identified on radiographs of five of the six animals described. Loss of buttress support produced similar results to those described previously, with concomitant fractures of the fourth tarsal bone and the calcaneus described in three dogs. The injury occurred during free exercise, and all affected animals were over 5 years of age. Isolated fractures of the third tarsal bone have been described in the racing Greyhound.27 They are usually dorsal slab fractures and can be treated with lag screw fixation. It is claimed that this fracture is more common than was originally thought; an incidence of 20% was reported in a recent survey of tarsal fractures in racing Greyhounds.27 Prognosis is good for return to racing after surgical stabilization of the fracture, provided there is no evidence of joint collapse as a result of the fracture. Prognosis is excellent independent of presentation. Principles for identification and management of metatarsal fractures are similar to those of metacarpal fractures, which are more common. See Chapter 56 for additional information. Fractures of metatarsal IV occasionally occur in association with central tarsal bone fractures. Luxation or Subluxation of the Tarsocrural Joint The degree and direction of dislocation will depend on the nature and extent of the injuries (e.g., lateral collateral ligament disruption or distal fibular fracture will give a varus deviation with an opening on the lateral side of the tarsocrural joint). It is not uncommon to find that both medial and lateral supporting structures have been damaged (Figure 64-10, A). It also is not uncommon to find a combination of fracture and ligament disruption on different sides of the dislocated joint. The medial ligaments are disrupted most frequently owing to the large number of shear injuries affecting the medial side of the joint.19 This is significant because the medial side of the joint is subject to greater stress as a result of the slightly valgus posture of the hock.63 Reduction and stabilization of a distal fibular fracture can be accomplished in a similar fashion. A pin can be introduced in normograde fashion from the distal end of the bone (see Figure 64-10, B). Alternatively, pins can be used to fix the distal fibula to the tibia. Both types of pin placement can be protected with a tension band. The joint must be protected for 3 to 4 weeks after stabilization using a short lateral splint. Dealing With a Ruptured Ligament.: Primary repair of the ligament should be attempted. Once the ends of the ligament are identified, placement of suture using a locking loop pattern will restore continuity and prepare the structure for optimum healing. Unfortunately, primary repair is not always possible, but when performed, the tarsus must be protected during the healing period; this is best done using an internal splint applied directly over the damaged ligament to augment and mimic the action of the ligament. An internal splint will also ensure joint stability when primary repair is not possible. An internal splint is created by placing bone anchors, or screws with washers, at the attachment points of the ligament; these implants serve as anchor points for monofilament wire, nylon, or other substitute material that is used to augment or replace the damaged ligament. Successful stabilization in the tarsus is based on the knowledge that collateral ligaments are complex structures consisting of a long and a short component, and on an appreciation of the important role that both components have in stabilizing the joint in both flexion and extension.2 Because of their size and location, the short portions of collateral ligaments are often overlooked during repair procedures; this seriously reduces the immediate stability of the joint. A technique for replacing both long and short parts of collateral ligaments on lateral and medial sides has been described3: three small screws are used with one screw placed at the communal attachment of the collateral ligament on the distal tibia or fibula, and the other two at the distal attachment points of the short and long parts of the collateral ligaments (see description in anatomy section) (see Figure 64-10, B). Bilateral injuries must be stabilized on each side. An alternative technique22 uses transosseous tunnels to allow correct placement of suture material without the use of metal implants. This technique has been described as allowing more accurate placement of the suture at proximal and distal attachment sites for the collateral ligaments than can be achieved with the use of screws. Use of a malleolar tunnel resulted in a more isometrically placed prosthesis.33 Monofilament suture material was preferred to braided nonabsorbable material because of the high incidence of postoperative infection described when the latter was used.22
Tarsus and Metatarsus
Anatomy
Individual Bones
Articulations
Ligamentous Support
Innervation and Vascular Supply
Clinical Evaluation of the Tarsus
Fractures of the Individual Tarsal Bones
Fractures of the Calcaneus
Fracture of the Central Tarsal Bone
Fracture Dislocation of the Central Tarsal Bone
Second, Third, and Fourth Tarsal Bone Fractures
Fractures of the Metatarsal Bones
Tarsal Luxations and Subluxations
Fractured Malleolus
Ligament Rupture
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Tarsus and Metatarsus
Only gold members can continue reading. Log In or Register to continue