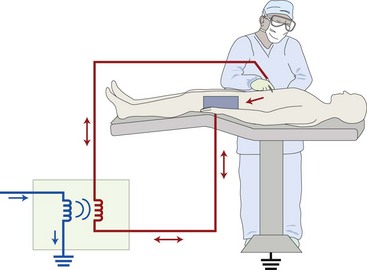
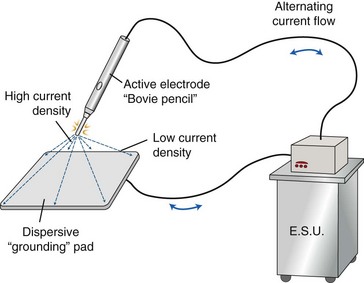
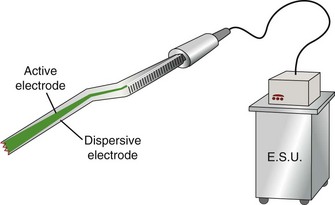
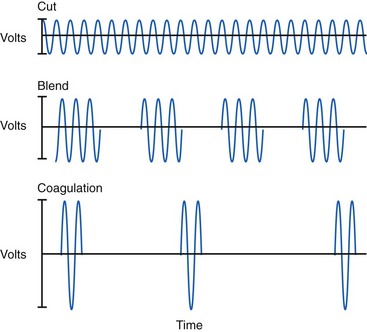
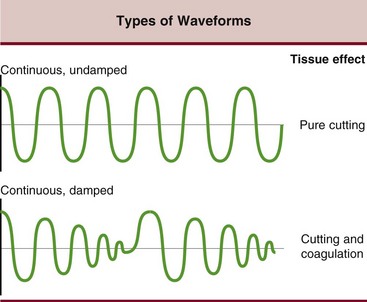
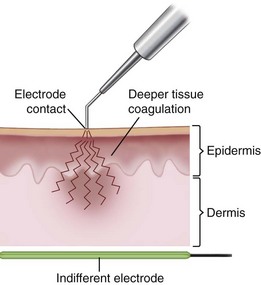
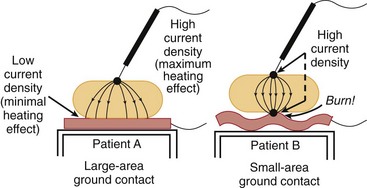
Chapter 16 In the 1920s, neurosurgeon Harvey Cushing, working with physicist William Bovie, developed a device that delivered high-frequency alternating electrical current that could be used to incise or coagulate tissue to obtain hemostasis.3,10 This device, commonly known as the “Bovie,” allowed Cushing to operate on patients that had been previously inoperable because of risk of hemorrhage. The Bovie has since become a cornerstone of modern surgery. Electrosurgery should not be confused with electrocautery. Electrocautery is the use of electrical current to heat an instrument, which is then used to cauterize tissue in the same manner as a branding iron affects tissues. Electrosurgery is a form of energy transfer via electrons from the instrument to tissues.3,10 All matter is formed of atoms with a nucleus of positively charged protons and neutral neutrons orbited by negatively charged electrons. Atoms become charged by gaining or losing electrons, creating a charged state. When positive and negative ions are placed in opposition, a gradient or voltage is created. A conductor provides a path so that electrons can flow along the gradient, creating a current. A current is proportional to the voltage and inversely proportional to the resistance of the conductor.6,10 Current always flows along the path of least resistance and heads toward the electron sink. Although commonly known as the ground in a circuit, for electrosurgery, the flow is actually toward the electron sink (patient return electrode, or dispersive pad) and not the earth ground; thus the generator is actually isolated from the earth ground (Figure 16-1). Living tissue is an excellent conductor because of its high electrolyte content.6 The mode of application of electrocautery energy may be monopolar or bipolar. Monopolar radiofrequency, which uses a current applied through a hand-held active electrode, travels back to the generator through an inactive electrode attached to the patient (the grounding pad), so that the patient is part of the electrical circuit (Figure 16-2).6,9,10 Monopolar electrocautery is also known as unipolar. Bipolar electrocautery consists of active and return electrodes incorporated into a single hand-held instrument, so that the current passes between the tips of the two electrodes and affects only a small amount of tissue (Figure 16-3).10 Because no flow of current occurs with electrocautery, a return electrode (grounding or dispersive pad) is not necessary. Although radiofrequency devices and lasers differ fundamentally in the way they generate heat within a tissue, both classes of devices are capable of producing temperatures within the range considered necessary for collagen denaturation and subsequent tissue shrinkage (65° to 75° C).10 When collagen is heated to 65° C, its heat-labile, intramolecular cross-links are broken, and the protein undergoes a transition from a highly organized crystalline structure to a random, gel-like state (denaturation).10 Collagen shrinkage occurs through the cumulative effect of the “unwinding” of the triple helix due to destruction of the heat-labile intramolecular cross-links and the residual tension of the heat-stable intermolecular cross-links.3,10 However, it must be remembered that when it comes to cell viability and tissue response, heat is heat. Once critical temperatures are reached, cells will die (45° C) and collagen will become denatured (65° C), no matter what the source of energy. Typical radiofrequency surgical generators operate as monopolar or bipolar units.9 A monopolar electrosurgical unit is used both in surgical dissection and for hemostasis. When undamped high-frequency electrical current (Figure 16-4) is passed through tissue, the active electrode, or tip, acts like a bloodless knife, and the tissue at the wound edges disintegrates.9 Thermal injury also occurs peripheral to the plane of cutting, resulting in thrombosis of tissue-associated blood vessels. When the current flow is intermittent, or the oscillations in the current are dampened, hemostasis is accomplished without cutting (Figure 16-5).6 Monopolar cautery causes cells to rapidly dehydrate and vessels to coagulate. Damage to tissue can be extensive, and the unit power setting should be the lowest possible to achieve the desired tissue effect (Figure 16-6). Frequently, precise application of energy to the tip of divided blood vessels is all that is needed. Cutting cautery may be of significant value in saving operative time and reducing blood loss. However, its extensive use creates increased susceptibility to infection and seromas when compared with cold knife dissection. The grounding plate must be well secured at some appropriate point under the patient and kept as large as possible for dispersing energy and avoiding burns (Figure 16-7).
Surgical Modalities
Laser, Radiofrequency, Ultrasonic, and Electrosurgery
Radiofrequency Technology
Tissue Effects of radiofrequency Energy
Monopolar versus Bipolar
< div class='tao-gold-member'>
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Surgical Modalities: Laser, Radiofrequency, Ultrasonic, and Electrosurgery
Only gold members can continue reading. Log In or Register to continue