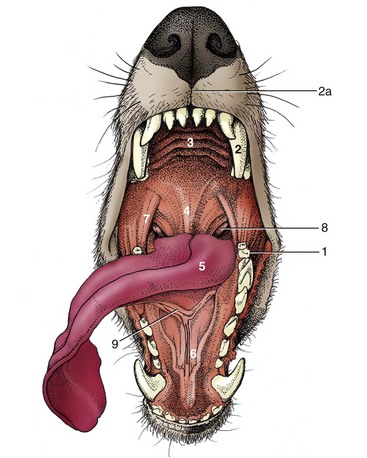
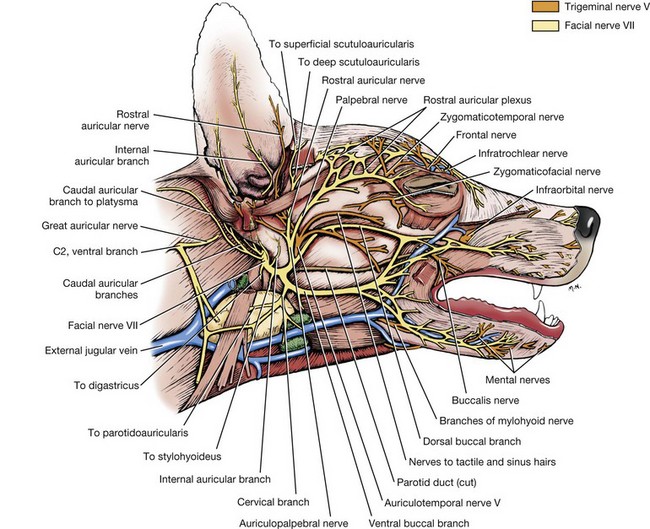
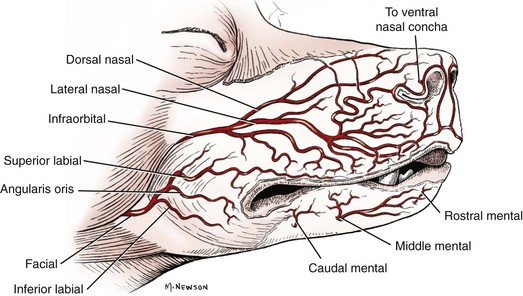
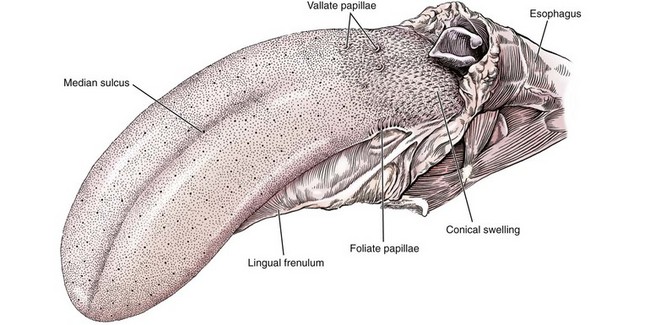
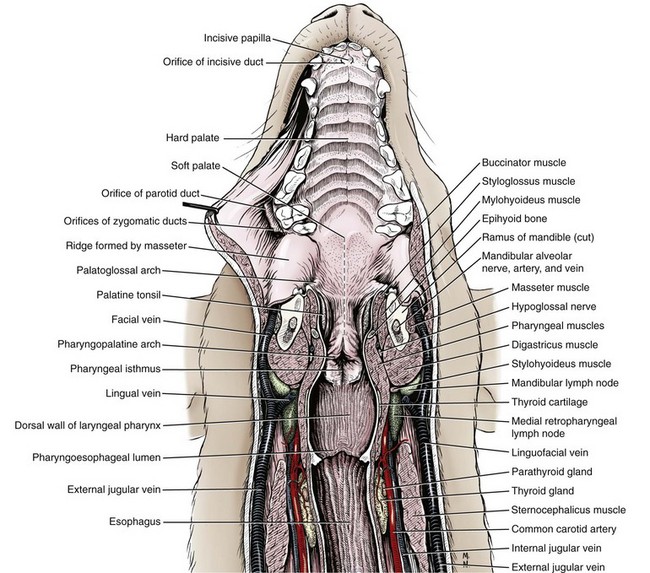
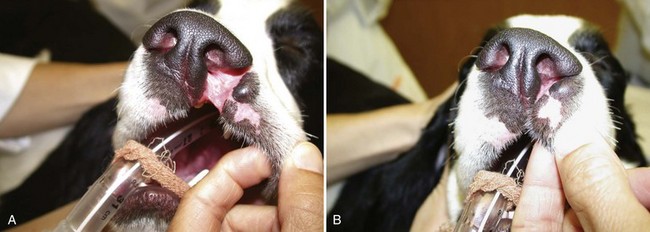
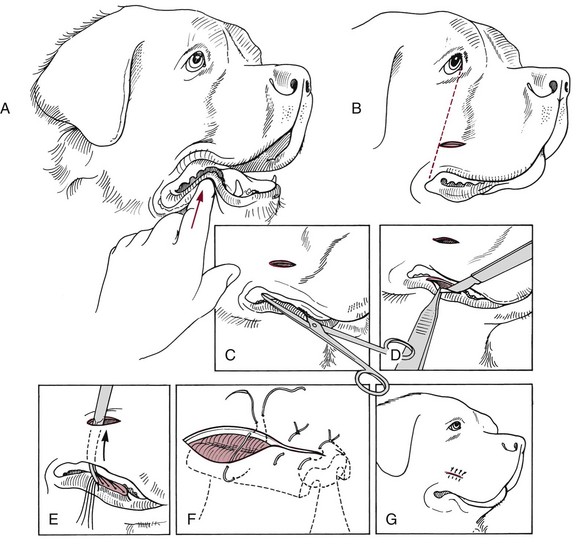
Chapter 87 The oral cavity generally refers to the space and associated structures bound laterally and rostrally by the lips and cheeks, dorsally by the hard palate, and ventrally by the tongue and underlying mucosa. The space ventral to the soft palate bound caudally by the pharyngeal wall makes up the oropharynx. The oral cavity proper refers to the space between the lower and upper dental arcades. The oral vestibule is the real and potential space lateral to the teeth and inside the cheeks (Figure 87-1). The lips and cheeks in dogs and cats are the structures that make up the lateral boundaries of the oral vestibule. They are composed of an outer integument layer, middle muscular and fibroelastic layer, and an inner mucosal layer.19 Cranial nerve (CN) VII (facial nerve) provides motor innervation to these muscles, and CN V (trigeminal nerve) provides sensory innervation to the outer and inner surfaces of the lips and cheeks (Figure 87-2). The tissues are relatively vascular, with branches of the facial artery supplying the lower lip and cheek and branches of the infraorbital artery supplying the upper lip and cheek (Figure 87-3).19 The lips and cheeks provide a lateral and rostral barrier to the oral vestibule and aid in expression of emotions such as anger and fear.19,45,55 Although not normally involved with prehension of food or drinking of water, the lips and cheeks may be important in retention of saliva, especially from the zygomatic and parotid salivary glands, the only glands that empty into the oral vestibule. The tongue is the most versatile organ in the oral cavity. It is responsible for food prehension, water lapping, sucking, mastication, tasting, swallowing, grooming, thermoregulation, and vocalization. Most of these functions require precise motor control, which is why the tongue consists almost entirely of skeletal muscle. The tongue consists of a root, which anchors it to the oropharynx; a body, which extends rostral to the root and is attached to the floor of the oral cavity via the frenulum; and the apex, which is rostral and unattached to the frenulum. Adjacent to each side of the frenulum is a raised area of mucosa running longitudinally called the sublingual fold. This fold courses rostrally, ending at the sublingual caruncle (see Figure 87-1). The mandibular and sublingual ducts course under the mucosal folds and open at the caruncle. The root of the tongue consists of a set of three paired extrinsic muscles: the styloglossus, hyoglossus, and genioglossus (Figure 87-4). The styloglossus muscle has three subdivisions, all of which originate on different regions of the stylohyoid bones and insert along the span of the ventral aspect of the tongue. In concert, they draw the tongue caudally; individually, they depress the tongue onto the point at which each muscle inserts. The hyoglossus muscle originates on the basihyoid bone and inserts on the caudal two thirds of the tongue. It acts to retract and depress the tongue. The genioglossus originates from the medial aspect of each mandible immediately caudal to the symphysis and separates into three bundles as it fans dorsocaudally. The vertical bundle inserts onto the rostral portion of the ventral tongue; the oblique bundle inserts onto the ventral region of the caudal aspect of the tongue; and the straight bundle inserts on the caudal third of the tongue, the basihyoid bone, and the ceratohyoid bone. The genioglossus muscles depress and protrude the tongue. All three pairs of extrinsic muscles are under control of the hypoglossal nerves. The intrinsic muscles of the tongue are complex and often course into one another with no discernible borders. To simplify matters, the muscles are categorized into units of fibers: superficial longitudinal, deep longitudinal, transverse, and perpendicular. The intrinsic muscles are responsible for protruding the tongue and a variety of other intricate movements. As with the extrinsic muscles, their actions are controlled by the hypoglossal nerves. Also contained in the body of the tongue is the lyssa. The lyssa is a tubelike structure of muscle, fat, and sometimes cartilage encased in a dense sheath of connective tissue that lies on the median plane on the ventral aspect of the tongue. The function of the lyssa is unclear; however, one theory is that it serves as a stretch receptor for the tongue.19 The dorsal surface of the tongue is covered with a thick mucous membrane consisting of cornified squamous epithelium. Within the mucous membrane are structural units called papillae (Figure 87-5) that help protect the tongue from objects that enter the mouth and assist in prehension of food and water.19 Fungiform, vallate, and foliate papillae are gustatory and therefore contain taste buds. Nongustatory papillae include filiform and conical papillae. Conical papillae have the added function of facilitating grooming by acting as a type of comb, especially in the feline tongue, where the papillae are shaped like hooks. A thin line of hair growth in the median sulcus (“hairy tongue”) can be a normal finding in some dogs.34 The oropharynx is the space between the oral cavity proper and the laryngopharynx and nasopharynx (Figure 87-6). It is bound dorsally by the soft palate and ventrally by the root of the tongue. The soft palate separates the nasopharynx from the oropharynx and consists of paired palatine, tensor and levator veli palatini, pteropharyngeal, and palatopharyngeal muscles covered in a stratified squamous epithelium on the oral surface.19 The palatopharyngeal muscles extend laterally and make up the palatopharyngeal arches. These arches form the rim of the intrapharyngeal ostium and act as a sphincter between the oro-, naso-, and laryngopharynx. The soft palate helps protect the nasopharynx from entrance of food during deglutition by becoming taut and elevated by tensor and levator veli palatini muscles, respectively. This action results in the caudal free edge of the soft palate pressing on the pharyngeal wall, sealing off the nasopharynx. The tongue compresses food against the soft palate to form a food bolus, which is transferred to the laryngopharynx and esophagus by muscular contractions of the tongue. The muscles of the soft palate are under the control of CNs IX and X. Blood is supplied to the soft palate by a branch of the maxillary artery that courses through the minor palatine foramen, forming the minor palatine artery.19 The tonsillar fossa, which contain the palatine tonsils, are situated immediately rostral to the dorsolateral aspect of each palatopharyngeal arch (see Figure 87-1). The paired palatine tonsils are masses of lymph tissue consisting of a larger, fusiform portion, which occupies the majority of the fossa, and a smaller portion that is less conspicuous and lies on the rostrolateral wall of the fossa.9 Normally, only a small portion of the tonsils is visible because they are mostly concealed in the fossa by an overlying membrane originating from the soft palate. The palatine tonsil derives its main blood supply from the tonsillar artery, a branch of the lingual artery.19 In addition to the palatine tonsils, dogs and cats possess a lingual tonsil (tonsilla lingualis) situated on the base of the tongue that is not grossly appreciable, and a pharyngeal tonsil (tonsilla pharyngea) located in the roof of the nasopharynx.19 The entire process of deglutition has been divided into three phases: oropharyngeal, esophageal, and gastroesophageal.58 The oropharyngeal phase has been further subdivided into the oral, pharyngeal, and pharyngoesophageal stages.58 The stages are sequential in occurrence, and each has a defined function. The oral phase involves formation of a food bolus by compression of food between the tongue and palate. The bolus is then propelled toward the base of the tongue at the entrance of the pharynx.58 This stage is completely voluntary, with sensory and motor innervation to the muscles of mastication, soft palate, and tongue provided by CNs V, VII, and XII.36 The bolus at the base of the tongue stimulates the reflex pharyngeal stage of deglutition. The tongue and pharyngeal constrictor muscles transport the food bolus through the pharynx through a peristaltic-like manner.58 To prevent food from entering the airway, the epiglottis covers the glottis, and the soft palate presses against the pharyngeal wall to block the entrance to the nasopharynx. The pharyngeal stage is involuntary and under the control of the swallowing center and CNs IX and X. The passage of food from the pharynx through the cricopharyngeal sphincter and into the esophagus is the pharyngoesophageal stage of deglutition. Relaxation of the sphincter starts as soon as the pharyngeal muscles begin constriction. The degree of sphincter opening varies with the size and consistency of the bolus.58 The pharyngoesophageal stage terminates with closure of the sphincter and relaxation of the pharyngeal constrictor muscles. This stage is also involuntary and under the control of CNs IX and X.58 Clinical Signs and Diagnostics General clinical signs of oral disease include ptyalism, dysphagia, inappetence, weight loss, pain, halitosis, and oral hemorrhage.2,7,34,41,51 Young animals with congenital oral disorders may fail to thrive.53 In many cases, the oral abnormality is an incidental finding on oral examination or noticed by the owner before any symptoms are apparent.2,51 Several patient factors must be considered in preparation for oral surgery. Organ failure, metastasis, infection, arrhythmia, endocrinopathy, and coagulopathy can influence the anesthetic and surgical plan, the overall prognosis, and the cost of treatment. For most patients, a thorough physical examination and appropriate blood, serum, and urine analyses are standard before anesthesia and surgery. The prothrombin time, partial prothrombin time, and buccal mucosal bleeding time tests should be considered when a coagulopathy is either suspected or anticipated during the course of surgery. Blood typing or cross-matching should also be considered in patients carrying a risk of significant blood loss. In patients known or suspected to have oral neoplasia, cytologic evaluation of fine needle aspirates taken from mandibular lymph nodes is recommended. Medial retropharyngeal lymph nodes also receive afferent lymphatic drainage from the oral cavity, particularly the tongue, but are palpable only when they are significantly enlarged.19 Evaluation of a three-projection thoracic radiograph study is a good screening tool for detection of metastasis in the lungs and other thoracic structures or if lower airway tract disease is suspected. Computed tomography (CT) images, particularly those obtained from a helical unit, provide an even better screening test for thoracic metastasis.39 Primary cleft palate is the most common congenital disorder affecting the lips in dogs (Figure 87-7). The pathogenesis and surgical principles are described in more detail in Chapter 100. Essentially, the condition results in a cosmetic defect that is repaired by reestablishing separation between the nasal and oral cavities and reconstructing the nares, nasal planum, philtrum, and lip by use of oral mucosal and cutaneous flaps. Abnormal dentition may require tooth extraction. Other congenital conditions of the lips include abnormal lip fold conformation, tight lip syndrome, and lower lip redundancy and eversion. In tight lip syndrome, the rostral edge of the lip tissue is pulled over the mandibular dental arcade (Figure 87-8). This results in trauma to lip tissue during mastication and, in some cases, inhibition of mandibular growth and disruption of normal tooth eruption.17,37 Tight lip syndrome has only been described in Shar-Peis. Treatment options include incising the lip mucosa at the gingival margin to allow the lip tissue to retract,37 excising a segment of skin on the chin to pull the lip margin ventrally,37 or deepening the rostral and lateral vestibule.17 Congenital redundancy and eversion of the lower lip, which is common in some large and giant breeds of dogs, can allow saliva to fall out of the oral cavity. Although not a health concern for the dog, a constant discharge of saliva can become a management issue for many owners. Antidrool cheiloplasty has been described as a treatment to increase retention of saliva.44,49 In this surgery, a mucocutaneous flap made in the lower lip is pulled through a full-thickness incision made in the caudodorsal vestibule and out through the cheek (Figure 87-9).46 The flap is then sutured in place to the subcutaneous tissue and the cheek skin. A case series describing the procedure in six dogs reported that all of the dogs had a decrease in the amount of saliva and food falling from the mouth, and owners in the study were very satisfied with the results.46 Alternatively, the redundant fold of tissue near the commissure can be resected with a full-thickness wedge resection. Resection can include any regions of hyperplasia, ulceration, or dermatitis. A stay suture is placed through the edge of the lip margin on each side of the resection to ensure exact apposition of the margin. The wound is closed in three layers, with a continuous pattern of 3-0 or 4-0 rapidly absorbable, synthetic monofilament suture in the mucosal and muscular layers and an intradermal or cutaneous pattern in the skin.
Soft Tissues of the Oral Cavity
Functional Anatomy and Physiology
Tongue
Oropharynx
Tonsils
Physiology of Deglutition
General Considerations
Disorders of the Lips and Cheeks
Congenital Disorders
< div class='tao-gold-member'>
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Soft Tissues of the Oral Cavity
Only gold members can continue reading. Log In or Register to continue