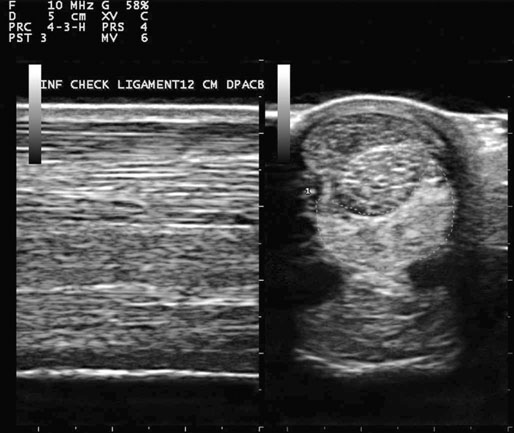
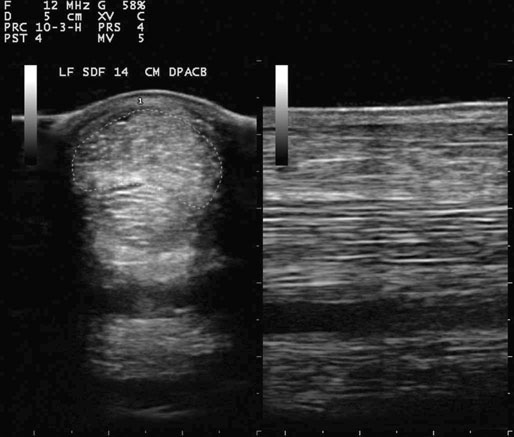
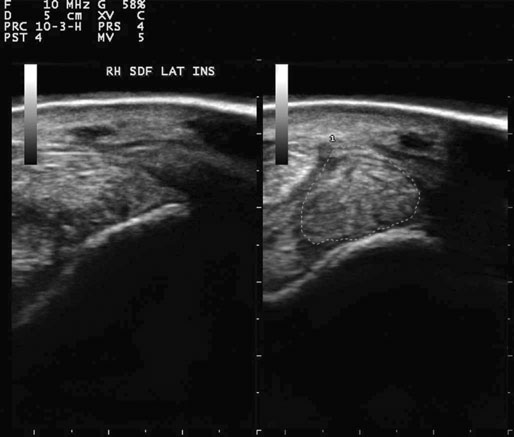
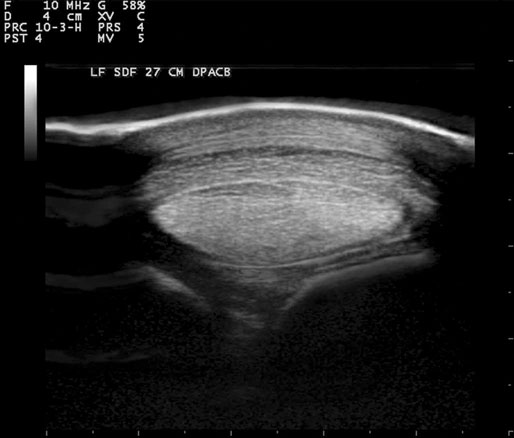
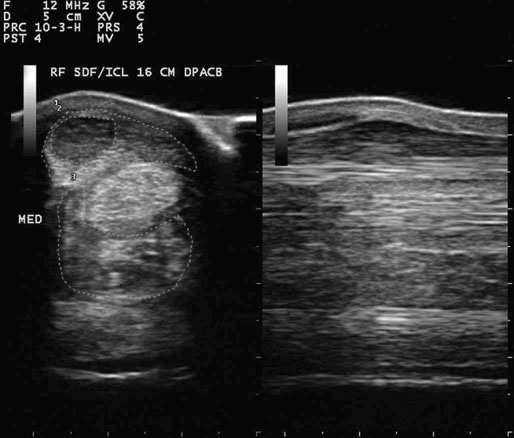
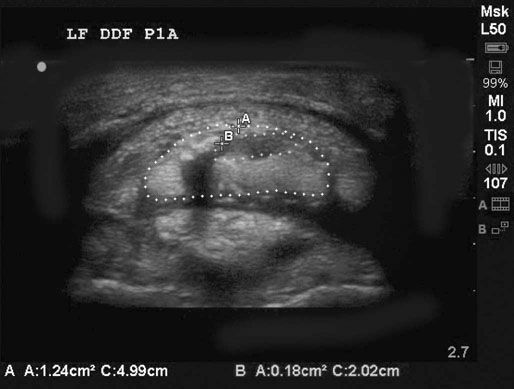
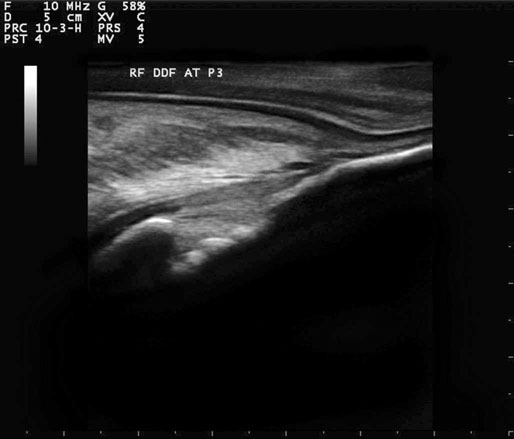
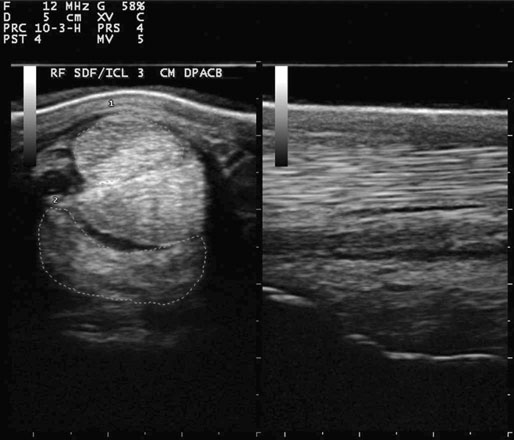
Horses presented for superficial digital flexor (SDF) tendinitis are usually in full athletic use. Affected horses often have a workload that consists primarily of galloping and/or jumping (Fig. 20.1). Most tendon injuries are due to cumulative damage rather than a single event, the exception being a fall or a strike from another limb. Horses often develop clinically apparent pain, swelling and lameness 2–3 days following SDF injury. Lameness ranges from grade 1 to 3 of 5 and is often transient or intermittent. Lameness often resolves rapidly with the use of ice, rest and anti-iflammatory agents. There will acutely be pain on palpation, heat and swelling at the lesion site. Pain on flexed palapetion is often the sign with longest duration as the lameness resolves. Affected horses frequently exhibit a decrease in performance ability after the initial lameness resolves.1,2 For SDF branch lesions, a low palmar digital nerve block generally provides analgesia. For SDF lesions in the metacarpal/metatarsal region, a high palmar nerve block resolves the lameness.3 Increased size of the affected tendon region combined with loss of echogenicity and normal parallel linear fiber pattern observed with diagnostic ultrasonography provides the definitive diagnosis (Fig. 20.2, Fig. 20.3, Fig. 20.4, Fig. 20.5, Fig. 20.6).4–10 Tenoscopy of carpal and digital sheaths provides diagnostic information as well as further treatment options. For example, under arthroscopic guidance debridement of frayed tendon fibers and resection of proliferative synovium and adhesions may be performed.11,12 • to control inflammation and prevent further tendon injury directly, through reducing tendon fiber swelling and influx of inflammatory mediators, or indirectly, through further exercise • provide adequate tendon support, primarily through shoeing • provide adequate rest followed by graduated increases in exercise to allow for optimum tendon healing. Cold therapy, such as ice for 20 minutes 2–3 times/day for three weeks, is an effective adjunct to reduce inflammation. Treatment with intramuscular polysulfated glycosaminoglycan, 500 mg every four days for seven treatments, has been shown to improve tendon healing.13 Although stem cell and platelet rich plasma (PRP) injections are in common use, no contolled study has yet shown that they produce collagen within injured tendon or ligament. A recent paper has shown that mesenchymal stromal cells survivied for approximately 10 days when injected into damaged tendon, and that they did not migrate, indicating little viable activity.14 Embryonic stem cells were able to survive for 120 days and to migrate indicating that futher research is warranted to determine if embryonic cells might produce viable tendon collagen. Another recent paper has shown that insufficient amounts of growth factor are released from platelets using current techniques to induce collagen growth.15 Stall (12′ by 24′) confinement with hand-walking should be initiated following examination. Unless the tendon is so severely damaged that rupture appears likely (rare), hand-walking is an important part of treatment and should not be delayed. If a free or box stall type of mechanical exerciser is available, horses can exercise up through the trot phase on this equipment. Walking times can be moderately increased above hand walking times. All exercise should be under supervision. Aquatic treadmills are also useful for horses when they reach the level of healing equivalent to the trot phase; earlier use may be excessive work for healing soft tissues.16 Following an initial period of stall rest and hand-walking, the SDF tendon should be re-evaluated using physical examination and ultrasonography to assess healing.17 Increasing exercise should be based upon examination findings rather than time elapsed. The horse should be confined to a space small enough so that it can only walk when not undergoing controlled exercise until healing is sufficient to allow canter work under saddle for one week. Please refer to Tables 20.1–5 for detailed exercise protocols. Table 20.1 Exercise protocol following the first examination (0–60 days). Horse is confined to a stall or equivalent size paddock (12′ by 24′ maximum) Table 20.2 Exercise protocol following the second examination (60–120 days). Horse is confined to a stall or equivalent size paddock (12′ by 24′ maximum) Table 20.3 Exercise protocol following the third examination (120–180 days). Horse is confined to a stall or equivalent size paddock (12′ by 24′) Table 20.4 Exercise protocol following the fourth examination (180–240 days). Horse can be turned out after riding exercise when it has been cantering five minutes for one week Table 20.5 Exercise protocol following the fifth examination (240–300 days) Superior check ligament desmotomy has been shown to improve SDF appearance in the short term; long-term results have been less encouraging. Superior check desmotomy has been associated with significantly increased strains on the SDF tendon and SL.18 Horses treated surgically were 1.2 times more likely to develop recurrent or new injuries after returning to training than horses managed non-surgically. Racehorses that have undergone a superior check ligament desmotomy are 5.5 times as likely to suffer a subsequent suspensory ligament injury as are horses without desmotomy.19 The SDF tendon has little margin of safety as horses in full work such as galloping or jumping generate forces near to its breaking strength.20,21 The SDF tendon and the suspensory (interosseous) ligament are the primary load bearing structures in the forelimb22 and are the soft tissues at greatest risk of injury in the horse that is working at speed. Factors that place excess load on the tendon, such as muscle fatigue which places increasing load on the much smaller, tendinous portion of the muscle/ tendon unit, poor hoof conformation/shoeing or lameness in another limb, place the tendon at increased risk of failure. SDF tendinitis prevention consists of: • increasing work load gradually rather than abruptly. A 5% increase in workload per week is generally a safe guideline • being attentive to hoof shape and shoeing to avoid a long toe, low heel configuration and to prevent a break in pastern/hoof axis • early recognition and treatment of other lameness to prevent compensatory tendon overload • recognition that certain conformational faults, particularly ‘back at the knee’ conformation, load the SDF additionally and place the horse at increased risk of tendon injury when in full work. • fifteen minutes of walk warm up prior to faster work in every exercise session will preload the SDF tendon to better withstand the forces applied without injury. Diagnostic ultrasonography will define the presence and extent of DDF damage (Fig. 20.7).23,24 For a diagnostic examination of the DDF within the hoof, as well as the navicular bursa and the impar ligament, the shoe should be removed and the frog should be pared to provide a level surface for good transducer contact. The foot should be soaked in water overnight to further soften the tissues. The insertion of the DDF on the solar aspect of the distal phalanx, the navicular bursa and the impar ligament can then be evaluated for disease (Fig. 20.8). Ultrasonography will also allow for sequential examinations, which are critical for the accurate assessment of healing stage of injured tendon so that an appropriate treatment and rehabilitation plan can be formulated for each stage of healing.17 For general tendinitis medical treatment, please refer to the section on SDF tendinitis. • diffusion of local anesthetic across membranes which are not sufficiently permeable to allow diffusion of larger molecules.25 • anesthesia of local nerves proximal to the bursa, causing reduction in pain that was not the result of inflammation within the bursa. Tarsal sheath synovitis may be treated medically in a similar fashion to the digital sheath (see following section. Tenoscopy of the sheath is an effective treatment for chronic/complicated cases with extensive synovial membrane proliferation and/or adhesions.26 • muscle fatigue, placing increasing load on the much smaller, tendinous portion of the muscle/tendon unit, poor hoof conformation/shoeing, or lameness in another limb • once a few fibers are damaged, strength is reduced and the tendon is predisposed to further fiber rupture with continued work • hemorrhage at the site of ruptured fibers and associated inflammatory mediator release cause further fiber damage either through compression by hematoma expansion or the detrimental effects of inflammatory products • palmar digital neurectomy used to treat heel pain likely leads to atrophy of the deep digital flexor tendon, placing horses at increased risk of DDF injury or rupture after the procedure. Also, following neurectomy horses lose the ability to protect the DDF tendon from over strain or to show clinical signs of DDF damage until they lose control of their ability to place the toe following complete tendon rupture. Athletic performance deteriorates in horses with DDF tendinitis due to initial lameness, followed by prolonged tendon weakness during the recovery phase. If excessive exercise is attempted while the tendon is relatively weak, the risk of tendon reinjury is high, leading to a repetitive syndrome of repeated short periods of acute lameness followed by longer periods of inability to perform regular work. DDF tendinitis prevention consists of: • increasing workload gradually rather than abruptly. A 5% increase in workload per week is generally a safe guideline • being attentive to hoof conformation and shoeing to avoid a long toe, low heel configuration and to prevent a break in pastern/hoof axis • early recognition and treatment of other lameness to prevent compensatory tendon overload • recognition that ‘heel pain’ may be due to excess strain on the DDF and that navicular bursitis may lead to secondary adhesions between the bursa and the DDF, leading to DDF damage. AL-DDFT desmitis can also occur secondary to moderately severe or severe SDF tendinitis, if the SDF tendon becomes sufficiently enlarged to contact the medial and lateral borders of the AL-DDFT. Adhesions may subsequently develop which cause AL-DDFT inflammation and damage.27 Diagnostic ultrasonography will reveal AL-DDFT enlargement, loss of echogenicity and deterioration of fiber pattern (Fig. 20.10).27 AL-DDFT desmitis and associated enlargement of the ligament may cause the DDF tendon to be completely encircled and compressed by the SDF and the AL and may be an additional source of the chronic pain often associated with AL desmitis (Fig. 20.11).
Soft tissue injuries
Tendinitis and desmitis
Superficial digital flexor tendinitis
Recognition
History and presenting complaint
Physical examination
Special examination

Treatment and prognosis
Therapeutic aims
Therapy
INJURY
0–30 DAYS
30–60 DAYS
Mild
Hand-walk 15 minutes twice daily
Increase walking time by 5 daily minutes per week
Moderate
Hand-walk 15 minutes twice daily
Increase walking time by 5 daily minutes per 2 weeks
Severe
Hand-walk 10 minutes twice daily
Hand walk 15 minutes twice daily
PROGRESS
60–90
90–120 DAYS
Good
Ride at walk 25 minutes daily
Increase 5 minutes every 2 weeks
Same protocol
Fair
Same as above
Poor
Hand-walk 30 minutes twice daily
Ride at a walk for 20 minutes; hand walk for 20 minutes at another time
PROGRESS
120–150 DAYS
150–180 DAYS
Good
Add a 5 minute trot set every 2 weeks
Add a 5 minute trot set every 2 weeks
Fair
Ride at a walk for 40 minutes daily and hand walk
Add a 5 minute trot set every 2 weeks
Poor
Re-evaluate case to determine cause and discuss further treatment options
PROGRESS
180–210 DAYS
210–240 DAYS
Good
Add canter 5 minutes every 2 weeks
Add canter 5 minutes every 2 weeks begin ground pole exercises
Fair
Add trotting 5 minutes every 2 weeks
Add canter 5 minutes every 2 weeks
Poor
Re-evaluate case and discuss further treatment options
PROGRESS
240–270 DAYS
270–300 DAYS
Good
Racing speed work, jumping or other competitive training
Ready for competition
Fair
Add canter 5 minutes every 2 weeks
Full flat work; no racing speed work or jumping
Poor
Re-evaluate case and discuss further treatment options
Surgical options
Etiology and pathophysiology
Prevention
Deep digital flexor tendinitis
Recognition
Special examination
Treatment and prognosis
Therapy
Etiology and pathophysiology
Prevention
Accessory ligament of the deep digital flexor tendon desmitis
Recognition
History and presenting complaint
Special examination
Soft tissue injuries: Tendinitis and desmitis