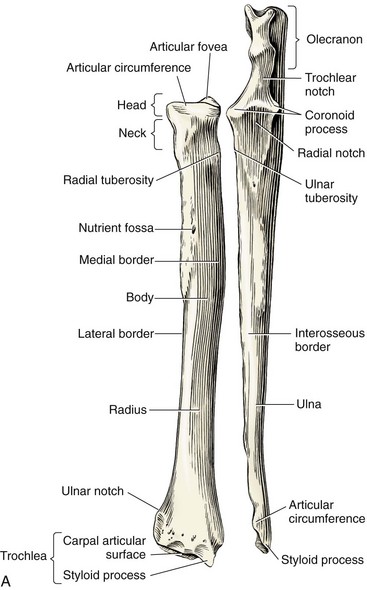
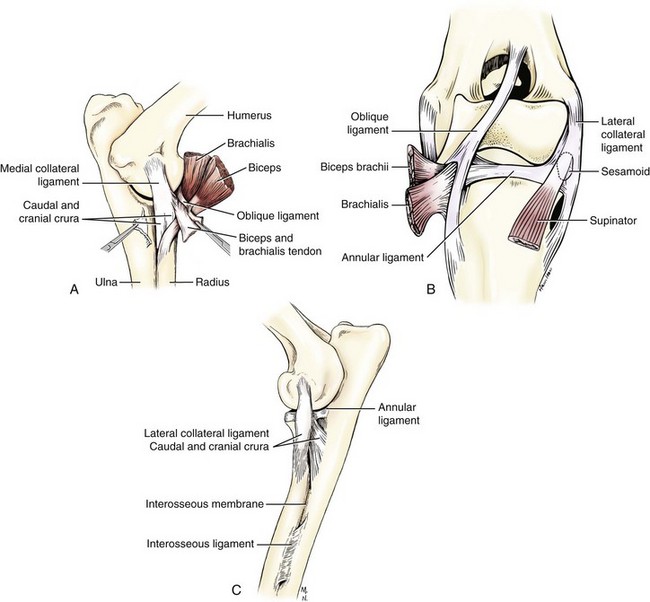
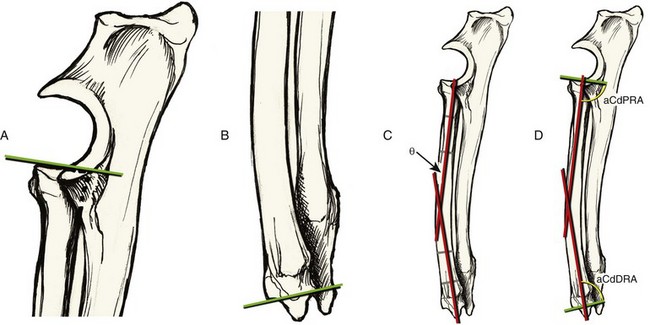
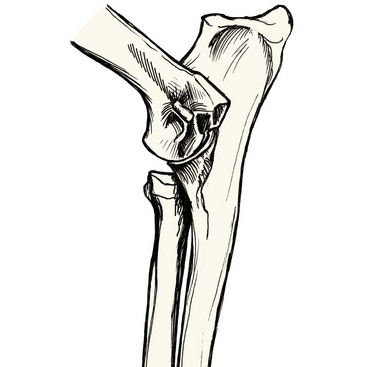
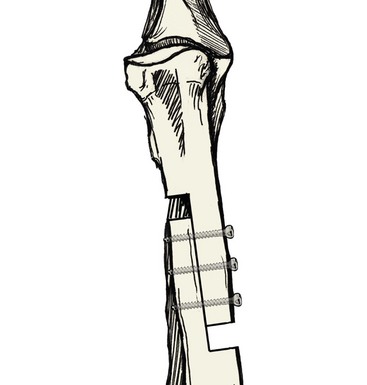
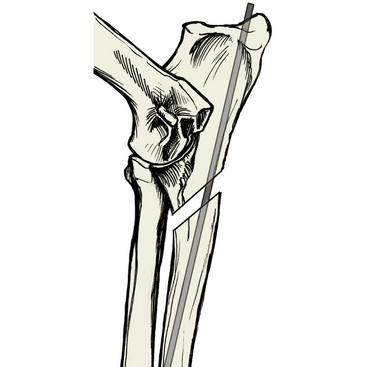
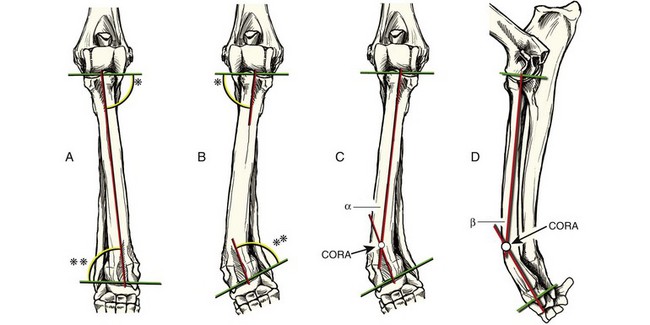
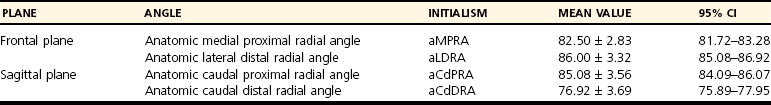
Chapter 55 The antebrachium comprises two bones, the radius and ulna, which cross one another in the frontal plane as they extend from the elbow joint proximally to the carpus distally (Figure 55-1). Proximally, the radius articulates with the ulna along its caudal border, which rests within a corresponding concavity in the ulna called the radial notch. Distally, the ulna similarly articulates with the radius along its medial cortex, where it rests within the ulnar notch. The raised prominences of the ulna on either side of the radial notch make up the medial and lateral coronoid processes. Whereas earlier texts suggest that the weight-bearing capacity of the coronoid processes is minimal, recent evidence refutes this. Cadaveric studies now suggest that 51% of the forelimb weight-bearing force is carried by the proximal radial articular surface at the level of the elbow; the remaining force is thus born by the ulna.33 The proximal ulna possesses other prominences of clinical importance, including both the anconeal process and the olecranon. The anconeal process exists as a hook-shaped projection of bone that fits within the olecranon fossa of the humerus during elbow extension. The olecranon serves as an important lever arm by acting as an attachment point for, among other muscles, components of the triceps brachii muscle that are powerful extensors of the elbow joint. Because the antebrachium is the only paired bone system in the quadrupedal appendicular skeleton in which both bones contribute to significant weight bearing, the resulting configuration is very complex, both in development and in function. Although the bones rest closely together, they are joined not by an osseous union, but rather by numerous soft tissue attachments. Thus, although motion occurs between the two bones during ambulation and weight bearing, it is attenuated by the soft tissue constraints that exist between the radius and ulna (Figure 55-2). This is of importance when attempting to surgically move a portion of one bone separate from the other, as is often necessary to treat some pathologic conditions. Proximally, the elbow joint capsule is singular and common to all three bones. The medial and lateral collateral ligaments of the elbow joint also tether the radius and ulna together. Each arises from its respective epicondyle of the humerus and bifurcates into two crura: a cranial division, which attaches to the proximal radius, and a caudal crus, which attaches to the ulna. The annular ligament of the radius is a transverse circumferential band around the radial head attached to the medial and lateral radial incisures of the ulna. The biceps brachii and brachialis muscles each have tendons of insertion that bifurcate and insert on the medial surface of the radius and the ulna. Distal to the elbow joint, the radius and ulna are joined by the dense interosseous ligament, which is flanked proximally and distally by the thinner interosseous membrane. The ligament proper terminates distally about midshaft of the antebrachium, where the two bones diverge medially and laterally as they cross one another. Several muscles share their origination between radius and ulna at the level of the mid-diaphysis and include the pronator quadratus, deep digital flexor, and abductor pollicis longus muscles. Distally, the joint capsule of the antebrachiocarpal joint arises from both the radius and the ulna. Fibers of this joint capsule are confluent with the distal extremity of the interosseous membrane and form a stout attachment between the distal ulna and radius referred to as the radioulnar ligament. Both the radius and the ulna possess physes proximally and distally that contribute to growth of each bone. Great differences exist, however, with respect to relative contributions to total longitudinal growth from the physes of each bone. Whereas both radial physes contribute substantially to longitudinal growth of the radius, 100% of ulnar growth distal to the elbow joint occurs at the level of the distal ulnar physis.6 The amount of contribution to longitudinal growth from the radial physes has been studied, with estimates for the proximal physis ranging from 30% to 50%, depending on the study.6 The proximal ulna possesses a physis that is responsible for olecranon elongation only.18 Further, the anconeal process arises from a separate ossification center, as documented in German Shepherd Dogs and Greyhounds.56 Because the entirety of ulnar length results from growth from the distal ulnar physis, and this length must match that of the radius growing from both the proximal and distal physes, the two bones change their positional relationship to one another during development. This phenomenon was elegantly demonstrated in a study utilizing radiopaque markers placed in both radius and ulna of juvenile dogs, which were then observed radiographically over time; movement between the radius and the ulna during skeletal maturation was documented.6 The age for physeal closure varies depending on the breed, but has been determined to range between 222 and 250 days in the Beagle.7 Recently, research has focused on understanding the alignment of the canine radius and ulna with respect to the elbow and carpus in an attempt to improve our understanding of “normal.” Bone alignment can be objectively quantified by determining the orientation lines for the joints above and below the bone in question, and then determining a particular axis of the bone between the joints in both frontal and sagittal planes (see Chapter 47). This was studied in the dog by radiographic assessment of 20 limbs of a variety of nonchondrodystrophic breeds.17 In the frontal plane, joint orientation lines of the elbow can be determined by drawing a straight line from the proximal-lateral-most aspect of the radial head to the proximal-most aspect of the medial coronoid process (Figure 55-3, A). For the radiocarpal joint in the frontal plane, the orientation line can be drawn tangentially across the distal radial articular surface, while disregarding the radial styloid process (Figure 55-3, B). The frontal plane radial anatomic axis is then drawn as the straight line that bisects the radial diaphysis (Figure 55-3, C). The anatomic axis of the radius and the joint orientation lines intersect and give rise to joint orientation angles both proximally and distally (Figure 55-3, D). This process can also be completed in the sagittal plane, where the joint orientation lines are generated from the most proximal aspects of the radial head, both cranially and caudally, for the elbow joint, and upon the most cranial and caudal distal aspects of the radius for the radiocarpal joint (Figure 55-4, A, B). Because the canine radius is bowed slightly, or possesses procurvatum, the anatomic axis must be determined for both the proximal and distal segments of the bone separately (Figure 55-4, C). The intersection of these segmental axes, in addition to the joint orientation angles in the sagittal plane, can be used to calculate the degree of procurvatum of the radius (Figure 55-4, D). Calculation of the joint orientation angles in both frontal and sagittal planes has utility in allowing the generation of a set of normal reference ranges with which to compare dogs whose bone alignment may be pathologically affected, as with angular limb deformities. In a recent study, the corresponding mean joint orientation angles were calculated in both frontal and sagittal planes from 50 Labrador Retrievers (Table 55-1).14 Table • 55-1 From these values, it should be noted that the canine radius does not sit perpendicularly to the elbow and carpus joint orientation lines. In the sagittal plane, the mean overall procurvatum, or sagittal plane alignment, was calculated by adding the difference between the anatomic caudal proximal radial angle (aCdPRA) and 90 degrees, the angular difference (θ; see Figure 55-4, C) between the two segmental anatomic axes, and the difference between the anatomic caudal distal radial angle (aCdDRA) and 90 degrees, because each of these angular relationships contributes to the procurvatum of the normal radius. This mean value was determined to be 26.6 degrees (range, 14 to 39 degrees). Thus it can be seen that in the sagittal plane, a wide range of procurvatum is present normally. Conditions affecting the juvenile canine radius and ulna can be subdivided into congenital conditions such as the dysostoses (discussed in Chapter 69), and developmental or acquired conditions. Various disturbances in appropriate physeal development of the radius and ulna have been widely reported and can result in asynchronous growth of the radius and ulna with concurrent shortening and angulation of one or both bones, depending on the timing of the disturbance, which physes are involved, and whether the physis in question has been damaged symmetrically or asymmetrically. Similarly, anything that prevents the ability of the radius and ulna to slide upon one another during development, as previously discussed, can result in asynchrony and maldevelopment. Asynchronous growth of the radius and ulna is most commonly observed as relative shortening of one bone with respect to the other, and may or may not be accompanied by angulation. Symmetric premature closure of the distal radial physis has been created in juvenile dogs experimentally through irradiation, thus serving as a model for the clinical scenario.40 Through this study, it was determined that when the distal radial physis is symmetrically insulted, the proximal physis assumes the majority of longitudinal growth in the radius, as the amount of elongation of the distal radius slows dramatically. However, this compensatory increase in growth at the level of the proximal radius falls short of maintaining appropriate overall radial length, and the radius subsequently shortens to the point where humeroradial and humeroulnar subluxation occur. With increasing space between the radial head and the capitulum of the humeral condyle, the condyle becomes cranially displaced, putting pressure on the coronoid processes of the ulna (Figure 55-5). The rapid decline in growth that occurs at the level of the distal radius also slows growth at the distal ulnar physis. The decrease in pressure on the radial head from lacking humeroradial contact results in thickening of the articular cartilage and increased growth from the proximal radial epiphysis. Although most of the dogs in this study did not develop angulation secondary to the uniform insult to the distal radial physis, concomitant distal displacement of the ulnar styloid process resulted in a varus deformity with internal rotation of the carpus in 3 of 8 dogs.40 Despite the fact that the proximal radial physis contributes less to longitudinal radial growth than the distal physis does in normal dogs,8 premature closure of the proximal radial physis can result in overall radial shortening. Radial shortening can range from being extremely pronounced to very subtle. Diagnosing and quantifying the condition can be challenging if the degree of shortening is very slight. Most imaging modalities focus on examining the radioulnar relationship at the level of the elbow joint to document the presence and severity of radial shortening. Utilizing a cadaver model, Mason et al.34 determined the sensitivity and specificity of lateral radiographic projections to be 78% and 86%, respectively. They further concluded that the amount of radial shortening required to achieve 90% diagnostic sensitivity with radiographs was between 1.5 mm and 4.0 mm. Although conflicting sentiment is seen in the literature regarding the use of radiography, with some reports suggesting high sensitivity and specificity,3 the consensus resulting from most research is that more sensitive diagnostics are required to adequately assess radioulnar congruity. Conventional computed tomography (CT) has been reported to allow accurate determination of radioulnar incongruence,22,25 but a recent report comparing both radiology and CT to arthroscopic examination of the elbow joint found the latter to be most sensitive and specific (94% and 81.9%, respectively), with the highest amount of agreement noted between individuals interpreting the images (89.8%) when diagnosing the condition of a shortened radius.57 Attempts to mimic gross examination of the radioulnar relationship for evidence of radial shortening in a manner less invasive than arthroscopy have been investigated with the use of three-dimensional (3D) image rendering based on CT.4 This study determined that 3D modeling was readily achievable, and allowed the diagnosis of radioulnar incongruence when the radius was shortened by as little as 1 mm, with a sensitivity of 82%, a specificity of 100% and interobserver agreement of 87%. Thus 3D modeling can serve as a diagnostic alternative to arthroscopy. In general, gradual, dynamic elongation following the principles of distraction osteogenesis (discussed in greater detail in Chapter 41) has advantages in the young animal, as these techniques allow some adjustability to adapt to the dog’s continued growth. Semi-controlled, gradual elongation of a shortened radius (due to symmetric closure of the distal radial physis) in young dogs was reported by Mason and Baker.35 This report described a transverse osteotomy of the proximal radius and the placement of separate pins in the radial metaphysis and across the humeral condyle. Elastic material was placed between the pins, thus applying a traction force on the proximal radius. Over a period of 14 days, the radial head was able to slide proximally, eventually matching the coronoid process and reestablishing contact with the humeral capitulum. Subsequent bone regeneration occurred at the osteotomy gap.35 The main advantage of this technique is that there appears to be little risk that the radial head will reposition itself too far proximally, as it should cease its migration when the articular cartilage contacts the humeral capitulum. What remains unknown is how large of a defect can be treated successfully this way. More controlled methods of gradually elongating the radius are possible and were first reported with the use of a Stader apparatus. The Stader apparatus is a type of external skeletal fixation device with a threaded connecting bar. This apparatus allows controlled distraction at the level of the osteotomized radius.38 More recently, radial distraction osteogenesis has been completed with circular external skeletal fixators, and lengthening of up to 50% of the original radial length has been achieved.45 Advantages of controlled distraction include the ability to adjust the latency, rate, and rhythm of the distraction according to the patient’s signalment and the radiographic appearance of bone regeneration within the osteotomy gap. The main disadvantage is that the proximal repositioning of the radial head is under the direction of the surgeon, and its final relationship to the ulna and humeral condyle must be confirmed through some type of imaging modality. Acute elongation techniques involve an osteotomy of the radius, the use of bone spreaders for radial distraction, and subsequent stabilization with a bone plate or an external skeletal fixator. If a transverse osteotomy has been performed, a large bone gap and lack of load sharing with the implant may result, unless a cortical bone graft of identical size is inserted into the distracted osteotomy. An alternative technique, which provides acute radial elongation while preserving load sharing, is the completion of a sagittal sliding (or “stairstep”) osteotomy. The osteotomy is stabilized with screws placed, in lag fashion, transverse to the sagittal portion of the osteotomy. Sagittal sliding osteotomy can be performed with or without the application of a neutralization plate or external coaptation (Figure 55-6).55 Irrespective of the technique used to perform an acute correction, confirmation that the final position of the radial head is appropriate requires radiography or, optimally, arthroscopy, following distraction. An alternative to radial lengthening is shortening of the ulna by completion of an ulnar ostectomy.19,46 The advantage of this technique is that, if the ulnar ostectomy is completed in a dynamic fashion (without rigid fixation), the dog’s humerus will compress the ostectomized ulna to a level where the coronoid processes match the radial head during weight bearing. This technique obviates the need to move the radial head to a specific position, as occurs with any of the radial lengthening procedures. Ulnar shortening is predominantly recommended for skeletally mature animals. If attempted in puppies, the risk exists that the narrowed ostectomy gap may heal before cessation of longitudinal growth (even if slowed) of the radius, resulting in loss of elbow joint congruence yet again. A recent study suggests that when ulnar shortening is performed, the ulnar ostectomy should be performed proximal to the interosseous ligament, and an intramedullary pin should be applied to the ulna to optimize normalization of contact patterns in the elbow joint and avoid subsequent varus deformity.46 Premature closure of the distal ulnar physis has been reported to be the most frequent growth plate injury in dogs, accounting for 63% of all physeal insults.48 It is well accepted that the geometric configuration of the distal ulnar growth plate is the primary reason why the distal ulna is affected by premature physeal closure. Most physes, such as the proximal and distal radial physes, are relatively flat and thus are predisposed to shear fractures. Longitudinal growth may continue uninterrupted from these relatively flat physes, as long as the germinal cells are uninjured and remain attached to the epiphysis. However, the distal ulnar physis is conical in shape and thus is unable to shear, regardless of whether the offending force is axial or lateral in nature. Thus, excessive force applied from any direction can cause compression of one side of the conical physis, resulting in injury to the germinal cells and subsequent retardation or cessation of ulnar growth.18 Although trauma is a frequent cause of premature closure of this growth plate, the heritability of premature ulnar physeal closure as related to conformational development of specific breeds has also been reported.28 Because 100% of ulnar growth distal to the elbow joint arises from the distal ulnar physis, injury to this physis frequently results in greater alteration in antebrachial morphology than injury to either of the radial physes. Retardation of growth of the distal ulnar physis can result not only in a shortened ulna but, because of intimate attachments between radius and ulna, in conformational changes in the radius. Although this is not always the case, typical changes seen in the radius subsequent to premature closure of the distal ulnar physis include shortening, procurvatum, distal valgus, and torsion. These changes occur as the radius continues to grow “around” the distal ulna, which is located caudolateral to the distal radius. The severity of these changes is dependent on the degree of ulnar growth retardation and growth potential remaining at the time of the insult. In addition to its effect on the radius, shortening of the ulna can cause humeroulnar incongruity, resulting in alteration of the trochlear notch and placement of excessive biomechanical loads on both the radial head and the anconeal process (Figure 55-7). These changes may ultimately lead to elbow joint osteoarthritis. Pure shortening of the ulna at the level of the elbow joint can occur in the absence of closure of the distal ulnar physis. Any condition that results in radioulnar synostosis before closure of the proximal radial physis may produce a shortened ulna.39 In the absence of antebrachial angulation, the main surgical treatment for a shortened ulna is a lengthening procedure. Similar to radial lengthening, surgical options include both acute and gradual techniques. Following ostectomy, the proximal ulna can be guided in a semi-controlled or controlled fashion. Executing a dynamic ulnar ostectomy just distal to the coronoid processes alone utilizes a semi-controlled method, as contraction of the triceps brachii muscle group, which inserts on the olecranon, exerts a traction force on the proximal ulna and thus pulls the articular surface of the ulna into congruency with the humerus. However, numerous complications can arise with this procedure and must be considered. It is important to recognize that the pulling force of the triceps brachii muscle is not perfectly axial, but rather the triceps brachii muscle pulls on the olecranon at an angle, thereby exerting a bending moment at the level of the ostectomy. This causes bending and caudal displacement of the proximal ulna, in addition to its proximal distraction, and can result in the formation of an iatrogenic recurvatum deformity of the ulna. Two methods to counteract this bending at the proximal ulnar ostectomy site can be used, while still allowing dynamic movement of the proximal ulna. For the immature patient, the most important technique utilizes the placement of an intramedullary pin in the ulna, thus combating bending at the ostectomy site. Although used more frequently in skeletally mature patients with a simple osteotomy (discussed later), an oblique ostectomy can also be completed in a proximocaudal-distocranial fashion, such that the geometry of the ostectomy will prevent excessive displacement (Figure 55-8). Important to note with this technique, however, is that with more aggressive ostectomies (in younger patients), or with cases of more severe ulnar shortening (where the resulting gap will be larger), the resulting gap may be so great as to prohibit the ends of an oblique osteotomy from contacting one another, thus rendering the technique to combat bending nonuseful. If completing the ostectomy with a pneumatic or battery-powered sagittal saw, it is easy to be overzealous and accidentally score the caudal cortex of the radius, which could result in the formation of a synostosing callus between the two bones. Placement of Hohmann retractors around the ulna will isolate the ulna and protect the radius while the ostectomy is completed. Further, sawing may be ceased before cutting entirely through the cranial ulnar cortex, thus allowing the ostectomy to be completed with an osteotome, again protecting the disruption of the periosteum or cortex on the caudal aspect of the adjacent radius. Despite creating an oblique ulnar ostectomy and placing an intramedullary pin, inherent instability can persist. Instability may result in the formation of an exuberant callus, which has the potential to form a bridging synostosis with the radius and to be a source of irritation because of the sparse soft tissue coverage overlying the caudal aspect of the ulna (Figure 55-9). Other complications involving the intramedullary pin include pin migration, irritation of the tendon of insertion of the triceps brachii muscle, and pin failure (Figure 55-10). Another method used to avoid instability and recurvatum of the ostectomized ulna is completion of an ostectomy of the distal ulnar diaphysis or removal of the physis itself. This technique allows the interosseous ligament to help stabilize the ulna from the bending force created by the triceps brachii muscle, while still allowing the ulna to slide proximally. What remains unknown is the comparative efficacy of low versus high dynamic ulnar ostectomies in the skeletally immature dog in reestablishing humeroulnar congruence. When applied in vitro to compensate for the opposite condition of radial shortening, ostectomy of the ulna distal to the interosseous ligament did not allow adequate movement of the ulna in one study. Important to distinguish in this study was that the ulna was being encouraged to move distally under the weight of the dog, rather than proximally under the pull of the triceps brachii muscle, as is the desired outcome with ulnar shortening. However, another study has reported clinical success with low ulnar osteotomies for treatment of premature closure of the distal ulnar physis.21 When treating the skeletally immature patient with a semi-controlled dynamic ulnar ostectomy, the goal is to allow unrestricted longitudinal bone growth of the radius. Therefore, bone regeneration at the ulnar ostectomy site, before the patient reaches skeletal maturity, may limit the corrective benefit of the ostectomy procedure, and in some instances may necessitate additional surgery. Using a method to prevent premature bone regeneration at the ostectomy site may be valuable. Methods used to try to prevent the ostectomy site from healing too quickly include creation of an ostectomy gap greater than 1.5 times the diameter of the bone,*,54 removal of all periosteum in the vicinity of the ostectomy,10 and insertion of a fat graft.9 Semi-controlled and controlled systems of guiding the movement of the proximal ulna are similar to what was previously discussed for the radius, including older methods of distracting fixators and using pins in both the humerus and the proximal ulna connected by an elastic band.35 These methods have largely been replaced by the use of circular external skeletal fixators. Other older techniques to deal with a prematurely closed distal ulnar physis in the skeletally immature dog include distal radial physeal stapling48 and ulnar styloid transposition with aggressive distal ulnar ostectomy.13 The basic principles employed with any of the dynamic ulnar ostectomy (semi-controlled and controlled) procedures can also be used for the skeletally mature animal diagnosed with humeroulnar incongruity due to a shortened ulna. However, osteotomies, rather than ostectomies, are commonly performed when the patient is mature, as early osseous union is encouraged in this situation. In addition, acute, one-stage static lengthening techniques may be used. All one-stage lengthening techniques utilize a distracted osteotomy, where the gap is maintained with a bone plate placed in bridging or buttress function, or where the gap is filled by the insertion of an autologous or autogenous cortical bone graft before plate placement. This author has also utilized a sagittal sliding osteotomy with subsequent placement of transverse cortical screws in lag fashion (Figure 55-11). As with radial lengthening, performing static ulnar elongation requires confirmation of appropriate elbow joint congruity, as the movement of the proximal ulna is under the direction of the surgeon. Making these treatment decisions can be challenging, and each case must be evaluated independently with consideration of the patient’s age and growth potential, and the nature of the angulation. For example, if a young patient is presented with premature closure of the distal ulnar physis with subsequent radial angulation, an ulnar osteotomy can be attempted to try to improve elbow joint incongruity and to release the bowstring effect of the affected ulna on radial development. However, the success rate of ulnar ostectomy as the sole treatment for premature distal ulnar physeal closure of juvenile dogs is relatively unknown. The influence of the procedure with respect to reestablishing normal antebrachial bone and joint alignment, or on the resolution of associated lameness, has never been prospectively studied in a large number of juvenile dogs. Recommendations of one small retrospective study suggest that despite diagnosing and treating affected animals at a young age (5 months), the technique was still frequently unsuccessful. Preoperative distal radial valgus greater than 25 degrees was detected in most cases unsuccessfully treated with distal ulnar ostectomy alone in this study and necessitated additional surgery, whereas those treated successfully possessed distal radial valgus less than 25 degrees.21 Thus, whereas ulnar ostectomy is a relatively less invasive procedure than osteotomies/ostectomies of the radius and ulna, its utility as the sole corrective procedure appears to be limited to those cases where radial valgus, procurvatum, and torsion are attributable to premature closure of the distal ulnar physis, and the radial angulation is not severe. For cases of more severe radial valgus, or when the angulation is not as previously described, but rather appears as varus, recurvatum, or internal rotation of the distal radius, then radial corrective measures are necessary. In these latter situations, it is highly likely that the distal radial physis has been damaged, thus resulting in more complex angular configurations. Antebrachial Angular Limb Deformity Surgical Planning.: Regardless of the age of the affected dog or the method of surgical correction and fixation used, accurate localization and quantification of angular limb deformities is critical in optimizing clinical outcomes. This author has performed such localization and quantification utilizing a method of presurgical planning called the center of rotation of angulation method. The center of rotation of angulation method is discussed in Chapter 47, and that information should be used to supplement the following discussion regarding antebrachial angular limb deformity planning and correction. The primary goal of this technique is to determine the apex of the deformity or deformities (also referred to as CORAs) using the radial anatomic or mechanical axis in conjunction with the joint orientation angles as determined by orthogonal radiographs in a step-by-step process. Step 1: If the dog has a normal contralateral antebrachium, the joint orientation lines, anatomic axis, and intersecting joint orientation angles are measured as outlined in the first section of this chapter (Figure 55-12, A) for the frontal plane. If the contralateral limb is abnormal, mean joint orientation angles (see Table 55-1) are used.
Radius and Ulna
Anatomy and Development
Growth and Development
Bone Alignment and Breed Conformation
Pathologic Conditions
Radial Shortening
Ulnar Shortening
Asymmetric Physeal Disturbance and Angulation During Development
< div class='tao-gold-member'>
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree