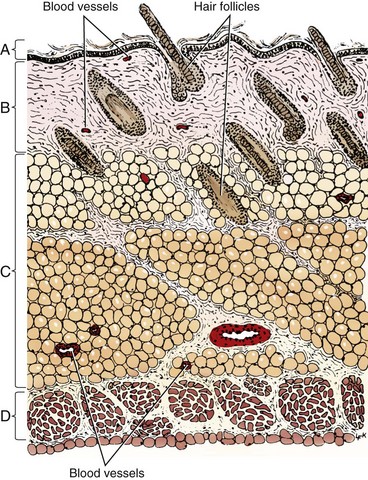
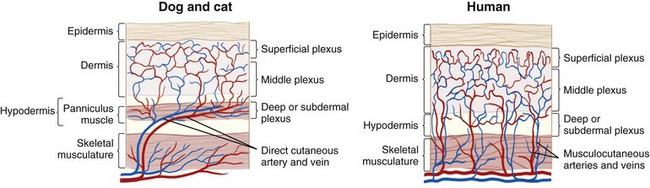
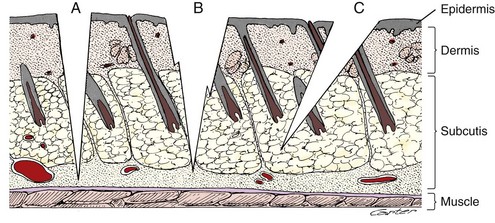
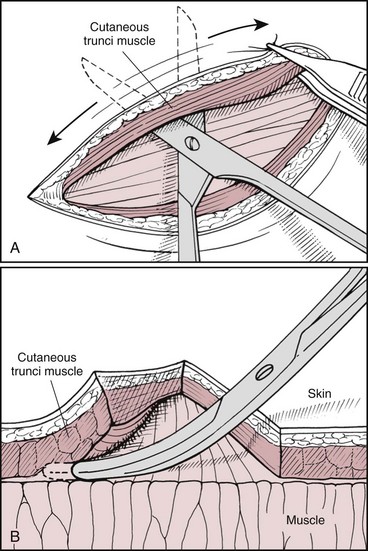
Chapter 75 The skin consists of two basic layers: the epidermis and dermis (Figure 75-1).28,29,41 Below the dermis lies the hypodermis, or subcutaneous tissue, which is often rich in adipose and loose connective tissue. The vascular supply is separated into three divisions: the superficial or subpapillary plexus; the middle or cutaneous plexus; and the deep, subdermal or subcutaneous plexus (Figure 75-2). Dogs and cats have differences in their cutaneous angiosomes. Dogs have a greater density of collateral subcutaneous vessels, at least in the trunk region.4,5 Also within the trunk region, cats have a smaller number and wider distribution of cutaneous perforators than dogs.5 Pull on the skin by cutaneous muscles and gravity produces tension along specific lines (see Figure 77-5). Because of constant tension, much of the skin’s connective tissue orients parallel to these lines.17 Skin tension lines in dogs and cats serve as a general guideline for incision creation and closure because tension will likely be reduced when large incisions are created and closed parallel to these lines.28 The anatomy and physiology of the skin vary between species, necessitating careful application of research results from other species.4,43 Fortunately, many studies published in human medical literature report research on sutured wound healing in dogs. The process of wound healing is described in detail in other chapters. Phases of healing for primarily closed wounds and those healing by second intention are the same; however, when the subcutaneous and dermal tissues are apposed by suture, healing encompasses a much smaller area.8,16 In primarily closed wounds with ideal apposition of subcutaneous tissues, the dermis, and the epidermis, healing may occur simply by reepithelialization at a rate of approximately 1 mm/d.8 A wound with perfect apposition may therefore have an epithelial seal within 24 hours.9 Collagen deposition, degradation, and reorganization also occur to some degree. After the wound has epithelialized, it is still not as strong as normal skin. Studies that compare wound closure techniques often use wound breaking strength as a measurement parameter. Most do not report the breaking strength of normal skin from the same patient; however, one study stated that tensile strength of a 5-mm-wide strip of normal dog skin was 9.9 kg.48 Wounded skin is only 5% to 10% as strong as normal unincised skin at 14 days after surgery. By 3 to 4 weeks, the strength of repair is about 25%; at several months, it reaches 70% to 80% of ultimate strength.27 Skin wounds regain tensile strength slowly, as illustrated by a study performed in rats with primarily closed skin wounds.48 Healed incisions were only 80% of normal strength at 1 year after incision.48 Sutured wounds in cats were only half as strong as those in dogs at 7 days postoperatively.5 “False healing” is described more frequently in cats than dogs. In this phenomenon, the wound appears to be healed from superficial observation, but dehiscence occurs after suture removal as soon as the stress of normal motion occurs.5 Clinical experiences led researchers to study potential differences in wound healing between cats and dogs.4,5 Based on laser Doppler perfusion imaging of primarily sutured wounds, cats had lower cutaneous perfusion for the first week after surgery followed by a more rapid gain during the second week.4 By 2 weeks, there was no difference in cutaneous perfusion in the two species. Cats also had a significantly lower wound breaking strength than dogs at 1 week postoperatively.4 Because of these differences, cats may have more wound healing problems associated with poor vascular supply or tension in the first postoperative week, and in some cats, it may be prudent to leave cutaneous sutures in place for longer than 10 to 14 days. Subcutaneous tissue (subcutis) plays an important role in wound healing by second intention.4 The role of the subcutis in healing of primarily closed wounds in dogs and cats has also been evaluated.4,5 In one study the skin of dogs and cats was incised, and subcutaneous tissues, including all tissues deep to the panniculus muscle but superficial to the thoracodorsal or lumbodorsal muscle fascia, were removed or left in place. The skin incisions were apposed by sutured primary closure. Although there were differences between species, removal of subcutis had an unexpected lack of significant effect on healing of primary wounds within species.4 It is possible that primary skin closure resulted in inadvertent apposition of the remaining subcutis in this study, allowing its continued positive influence on wound healing. Factors affecting wound healing by second intention also apply to primarily closed wounds (see Chapter 76). Healing of primarily sutured wounds can be influenced by tension, pressure, motion, self-mutilation, and patient health. Decisions regarding creation and closure of wounds should be made with consideration to skin tension. As a general rule, larger skin defects should be created and closed parallel to tension lines (see Figure 77-5). However, on distal limbs where the skin is more taut, more loose skin is available around the circumference of the limbs compared with the proximal-distal direction.28 Therefore, tension may be less for limb defects created and apposed perpendicular to illustrated tension lines. Any tension on wound edges could disrupt cutaneous perfusion and retard wound healing.28,36,39 To determine whether closure of mass excisions or traumatic lacerations will be possible, place the animal in a natural standing position, if feasible, and gently lift the surrounding skin. The desired direction of closure is that which results in the least amount of tension. Wounds in areas subject to repeated shearing forces from motion have a greater potential for complicated healing. Choices of suture material, suture pattern, and postoperative coaptation must be made with this in mind. In some patients, simple primary closure may not be the best option for such wounds.39 Please see Chapters 76 to 80 for alternative techniques. Malnutrition that results in decreased albumin and hemoglobin levels will prolong wound healing, presumably because of a shortage of substrates needed for healing. In a study of rats, effects of nutrition on skin wound bursting strength and collagen formation, as measured by hydroxyproline content, were evaluated.44 The rats were severely malnourished for 2 weeks after surgery and then reintroduced to a normal diet. By 60 days after creation of the wound, the initially malnourished rats had the same wound strength and hydroxyproline content found at 21 days postoperatively in normal rats.44 Wound healing relies on a healthy immune system and essential nutritional elements. Necessary dietary components for a healthy immune system include glutamine, arginine, zinc, n-3 fatty acids, vitamin E, and an appropriate n-6:n-3 fatty acid ratio. For wound healing in particular, methionine and cysteine are important. These are normally present in any diet that is high in protein.25 Incision with a blade is usually performed with the scalpel held in a fingertip grip, with the scalpel handle resting below the surgeon’s palm and blade stability and incision depth controlled by pressure from the index finger (see Chapter 18). A pencil grip can be used for finer dissection or small incisions. The technique and amount of pressure applied to the blade affect the quality of the incision (Figure 75-3) and thus the ability to achieve adequate apposition of tissue layers during closure. Practice on models of different density such as fabrics, avocado or banana skin, and hot dog or sausage skin help improve technique. Scalpel incisions made too timidly will result in greater tissue trauma by creating multiple or jagged cuts. Incisions made too boldly may inadvertently damage underlying tissues. Beveled incisions are difficult to close cosmetically with cutaneous or intradermal sutures because of the asymmetric nature of the wound edges. Edges of incisions may require undermining to improve exposure or reduce tension before closure. Undermining is performed with a combination of blunt and sharp dissection with Metzenbaum scissors (Figure 75-4). Use of a scalpel blade for undermining is more likely to cause tissue trauma or a jagged incision. Advantages of laser and electrocautery for incisions include hemostasis and lymphatic sealing.2,45 In dogs and cats, however, sharp dissection is considered more ideal for skin incision than either modality. If used incorrectly, laser and electrocautery may result in thermal damage to the wound that affects cutaneous perfusion and delays wound healing. When skin is incised by radiowaves, CO2 laser, or monopolar electrocautery, char will penetrate skin peripheral to the incision edge 0.171, 0.215, or 0.255 mm, respectively.35 In experimental studies in dogs, incisions made by sharp dissection with a scalpel blade had approximately twice the wound strength at 10 to 12 days after surgery as those made with electrocautery.21 Scalpel incisions produced less drainage than laser and electrocautery incisions and had faster and stronger healing.13 Results must be interpreted with caution, however, because details of electrocautery and laser settings were not reported. Compared with other wound management techniques, primary wound closure provides simpler wound care, less need for bandages, faster wound healing, reduced pain, less scarring, protection of vital underlying structures, and more cosmetic or esthetically pleasing results. For these reasons, primary wound closure is always ideal if the patient and wound qualify (Figure 75-5). Planning primary wound closure should involve consideration of patient and wound characteristics. This is the “art” of medicine and surgery that is developed with experience. As discussed earlier, patient factors can have a significant effect on wound healing and must be considered when deciding the location of any incision, type of wound management, and closure technique. For example, interrupted ventral midline skin sutures are often avoided in nursing animals because of local skin irritation and potential interference with suckling. The temperaments of some patients (e.g., stray or exotic animals or wildlife) may limit the clinician’s ability to provide appropriate aftercare; therefore, primary wound closure is preferred. If exercise restriction is not possible, wound closure techniques must take into account extra activity and stress that will be placed on the incision and potentially limited access for suture removal or aftercare. For a patient with uncontrolled hyperadrenocorticism, wound healing can be delayed and the immune system’s ability to fight infection can be impaired; therefore, primary wound closure is preferable over second intention healing or grafting. Wounds located in a region where contamination, pressure, motion, or tension is likely might be managed more effectively if left open or closed with other reconstructive techniques. Absorbable suture materials that maintain strength for long periods may be preferred in patients with uremia, excess glucocorticoids, or advanced age because of concern for delayed healing potential.39 In these patients and animals with traumatic or contaminated wounds, use of suture material impregnated with antimicrobial agent might be considered. Freshly incised, clean or clean-contaminated wounds are most often reapposed with primary closure. A traumatic wound may be considered a candidate for primary closure if it has occurred within 3 to 6 hours and the wound edges appear fresh and vascularized. There should be no evidence or history of crushing injury or devitalization and no visible contamination or debris after wound irrigation. Additionally, the patient should be healthy with no malnutrition or underlying disease affecting wound healing.8,46 Within a “golden period” of 3 to 6 hours, bacteria within a minimally contaminated wound can multiply to 105 per gram of tissue or milliliter of exudate, at which point the risk of infection increases dramatically. A much smaller number of bacteria present within a wound can also cause infection, depending on the type of bacteria and host and local environmental factors.46 Primary wound closure may be feasible in patients with wounds of several hours’ duration or that have local factors (e.g., pyoderma) that increase the risk or rate of wound contamination if wound bacterial loads can be reduced with irrigation and, when indicated, systemic antibiotics. Open wound management should be considered in wounds near dirty regions (e.g., perineum) if the incision is likely to be contaminated after closure. Wounds located in areas where skin is particularly mobile or undergoes shearing with motion may require additional layers of sutures for added security or to relieve tension. Areas of particular concern are the axillary and inguinal regions, skin over joints or bony prominences, and skin near the tail base or mouth. Tension on individual layers may be reduced by three-layer closure with apposition of deep and superficial subcutaneous tissues and skin or placement of subcutaneous, intradermal, and cutaneous sutures. Alternatively, stent sutures, tie-over bandages, and other tension-relieving techniques or postoperative immobilization may be used (see Chapter 77). In some mobile areas (e.g., the axilla), skin sutures with large knots may retain moisture or debris trapped within local skin folds or cause mechanical trauma as opposing skin rubs against the sutures. Affected animals may require an alternative closure type or more attentive postoperative care. Instruments for primary wound closure include tissue forceps, needle holders, and suture-cutting scissors. Tissue-dissecting scissors should not be used to cut sutures because they will dull the blades. Instruments that combine a needle holder and scissor function (e.g., Olsen-Hegar, Gillies) require expertise to prevent inadvertent cutting of the suture. Common types of thumb forceps include DeBakey, Brown-Adson, and Adson. The teeth on Brown-Adson and Adson thumb forceps provide a secure tissue grip and, on the Brown-Adson, a secure needle grip; however, both are more traumatic to tissues than DeBakey forceps.47 Cutaneous tissue is usually closed with nylon (Ethilon) or polypropylene (Prolene). The most common materials for absorbable subcutaneous or intradermal suture patterns are poliglecaprone 25 (Monocryl), glycomer 631 (Biosyn), polydioxanone (PDS), polyglyconate (Maxon), polyglactin 910 (Vicryl), and polyglycolic acid (Dexon). In one study comparing poliglecaprone 25 with polyglactin 910 in dogs, use of polyglactin 910 for buried continuous intradermal closure resulted in significantly more incisional swelling and redness early in the wound healing process. Later there was no difference between the two materials, and both groups went on to heal without complication.20
Primary Wound Closure
Skin Anatomy
Skin Physiology
Rate of Healing
Wound Strength
Species Differences
Subcutaneous Tissues and Healing
Skin Pathophysiology
Tension
Motion
Patient Health
Primary Wound Creation
Electrocautery and Laser
Patient Selection for Primary Wound Closure
Patient Characteristics
Wound Characteristics
Primary Wound Closure Techniques
Suture Selection
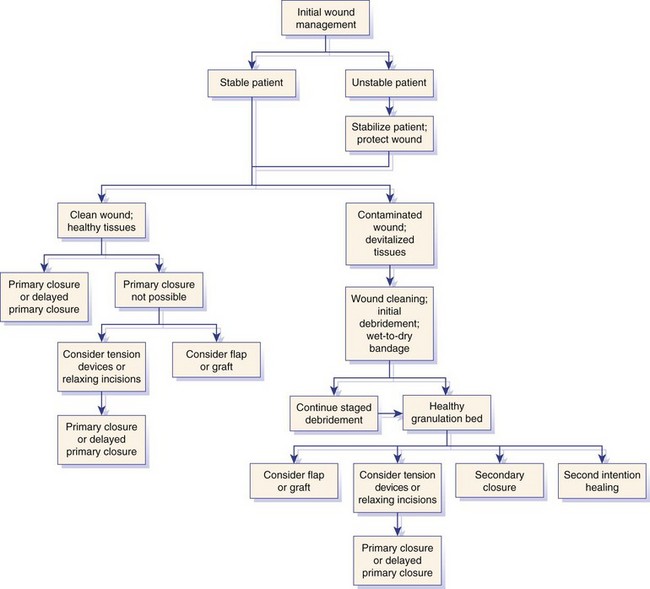
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree