44 Primary canine glaucoma
CLINICAL EXAMINATION
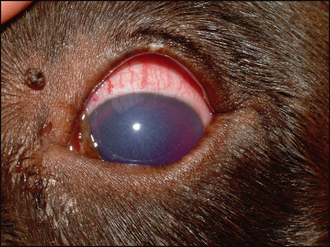
The affected eye is likely to be blind, or with severely reduced vision, demonstrated by a reduced or absent menace response. Corneal oedema will manifest as a blue–grey corneal discolouration. In addition to the clouding, the eye will also be red – episcleral congestion is usually marked and peripheral corneal vascularization develops which manifests as a red fringe around the limbus (ciliary flush) (Figure 44.1). The pupil can be assessed using a bright light source and is usually mid sized or dilated with very limited constriction when illuminated. A dazzle reflex remains if the pressure has not got too high. The indirect or consensual pupillary light reflex should be assessed and this can help with the prognosis regarding any return of vision – if there is no constriction of the fellow pupil there is less chance of a return of any useful eyesight in the affected eye.
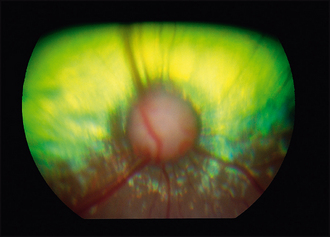
Detailed intraocular examination is hampered by the corneal oedema but the use of indirect ophthalmoscopy will be more informative than direct ophthalmoscopy since it provides better imaging through semi-opaque media. Thus, on fundus examination, cupping of the optic disc might be appreciated – seen as a small, dark disc with the blood vessels seeming to dip down into it from the retina (Figure 44.2). Peripapillary retinal degeneration is sometimes seen, along with more widespread hyper-reflectivity and blood vessel attenuation in advanced cases.
Measurement of intraocular pressure is essential to reach a definitive diagnosis, to provide prognostic advice, to draw up a treatment plan and to monitor the effectiveness of the treatment. Without tonometry it is very difficult to assess the patient properly. If a tonometer is not available, then referral for pressure measurement should be considered. The technique for tonometry, using a Schiotz tonometer, Tonopen or TonoVet, is detailed in Chapter 1. Remember that there are several factors which can affect the intraocular pressure readings (Table 44.1).
Table 44.1 Factors that can affect intraocular pressure (IOP) readings
| Factor | Effect |
|---|---|
| Breed | Higher in terriers and fluctuates more in these breeds as well |
| Age | Decreases with age |
| Degree of restraint required | Pressure around the neck will result in higher readings |
| Position of head | Higher with the head back and elevated |
| Instrument used | Slight variations between types of tonometer |
| Amount of pressure used to measure IOP | Pressure on the globe (including the forced lid opening required to access the cornea) will increase readings |
Breeds affected by goniodysgenesis (UK list) include:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree