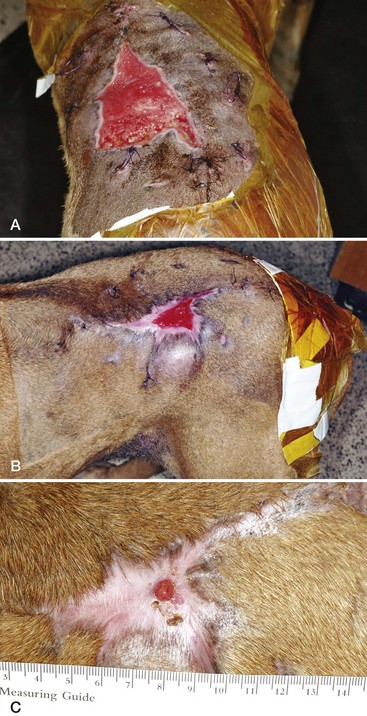
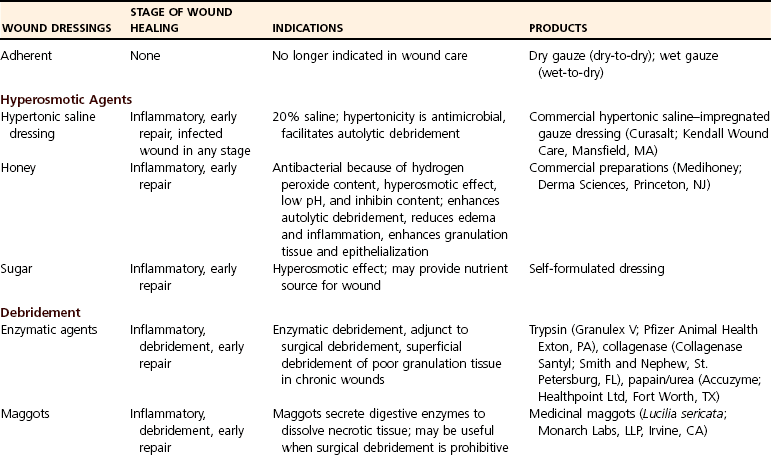
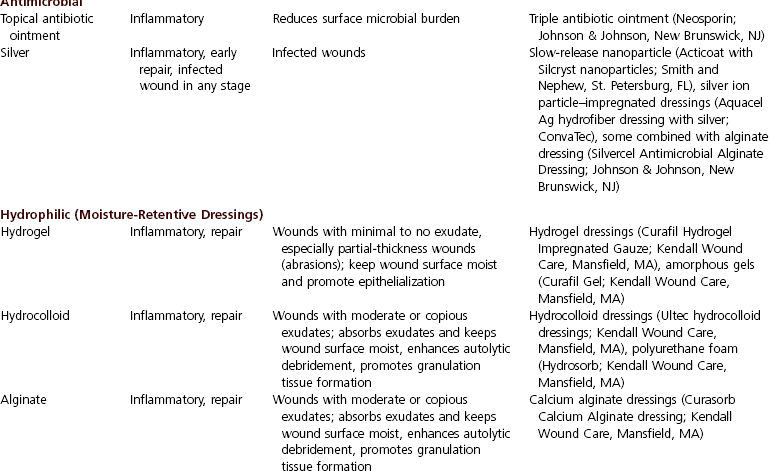
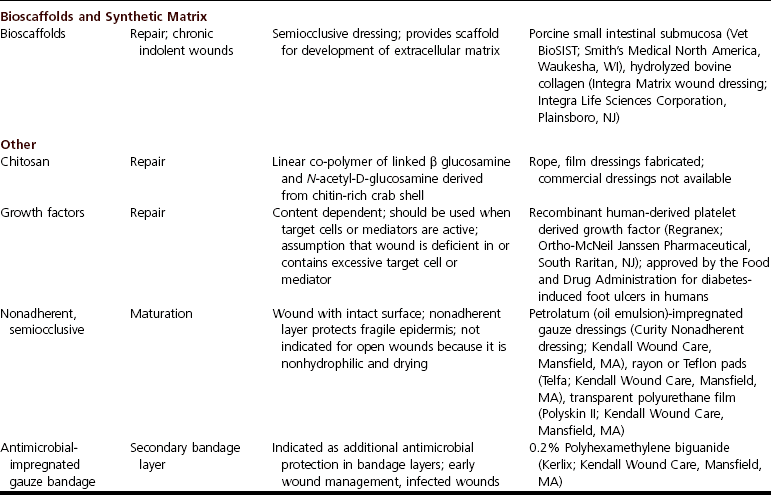
Chapter 76 A wound represents a loss in integrity of the skin and underlying tissue. Wound healing is the physiologic process that restores continuity of the tissues after injury, ultimately resulting in a continuous epithelial surface. Wound healing consists of four steps: (1) formation of a fibrin–platelet clot at the site of injury, (2) recruitment of white blood cells to protect the site from infection, (3) neovascularization and cellular proliferation, and (4) tissue remodeling. Wound healing is often described by its different phases: inflammation, debridement, repair, and maturation (see Chapter 10). These phases overlap and are affected by multiple endogenous and exogenous factors. A thermal burn is the result of close proximity or direct application of heat to the skin. Fire, cage dryers, heating pads, electrical cords, heat lamps, hot liquids, and malicious incidents are all causes. A thermal burn may have varying levels of tissue injury, depending on the severity. Deep and extensive injury can cause serious systemic compromise because of severe fluid, electrolyte, and protein loss; the risk for development of wound infection and sepsis is high. Burns have classically been described by the depth of injury as superficial partial (epithelial), deep partial (epithelial and partial dermal), and full thickness. The depth of injury is difficult to predict in the clinical situation, however, largely because of the phenomenon of delayed microvascular damage.46 Assessment of burn depth has been the subject of considerable investigation with the expectation that improved assessment will facilitate decision making in regards to treatment.41 Consequently, strict classification is no longer favored. Management of burns is described in Chapter 81. The primary goal of wound management is to facilitate wound healing without development of wound infection. A clear understanding of the differences among wound contamination, colonization, and infection is important. By definition, contamination is the presence of microbes on a surface. Contamination can lead to colonization in which surface microorganisms are replicating. Colonization can lead to infection in which there is invasion and replication of microbes within the tissue.4 Historically, as a guide to decision making, wounds have been classified according to duration, extent of tissue trauma, and degree of microbial contamination. Although these classifications gave strict time frames and considerations to the classification, the clinician’s consideration of the above factors, rather than strict classification, should dictate wound management. A burden of 105 colony-forming units (CFU) per gram of tissue has long been considered the threshold for development of infection, with the time frame required for this to occur being 6 hours or more.51 Investigation in people with burns showed the presence of more than 105 CFU/g in quantitative wound cultures correlated with histologic evidence of infection34,35,39 and was associated with a substantial mortality rate (i.e., 75%).49 Although 105 CFU/g may be a substantial burden and 6 hours sufficient to reach this number, the actual burden reached in a wound depends on other factors. These include the type and virulence of the contaminating microorganism; host factors, such as tissue trauma, systemic health, and immune compromise; and the presence of foreign material. Thus, a more relevant conceptualization of the effect of the microbial burden on the wound is: Species differences should also be considered in determining wound management strategies. Compared with dogs, the strength of primarily closed wounds is poorer in cats, and healing of open wounds is slower.10,11 In one experimental study, open wounds in cats contained significantly less granulation tissue than dogs, and the granulation tissue was more likely to have a peripheral, rather than central, distribution.11 Total wound healing was significantly lower at 7, 14, and 21 days after wounding in cats, and the percentage of epithelialization was also significantly less at 14 and 21 days. At 21 days after wounding, epithelialization and total healing were 34% and 84%, respectively, for cats and 89% and 98%, respectively, for dogs.11 Causes of these differences are unknown. Animals with open wounds that fail to progress toward healing should be evaluated for factors that may delay or interfere with the process. Potential causes include systemic disease, malnutrition, local tissue hypoxia and ischemia, bacterial colonization, altered cellular and stress response, repetitive trauma, presence of necrotic tissue, and tension. Blood work should be evaluated to rule out systemic illnesses such as uremia, hepatic disease, diabetes mellitus, hyperadrenocorticism, and feline immunodeficiency virus. Malnourished animals with severe hypoproteinemia or vitamin or mineral deficiencies may require supplemental nutritional support through use of feeding tubes until they are capable of sustaining an adequate balanced diet through normal alimentation. Normovolemia should be maintained to improve perfusion and oxygen delivery, and animals with severe anemia should receive red cell transfusions. Chronic wounds should be biopsied for histologic and microbiologic evaluation to rule out underlying local disease (e.g., sterile panniculitis or neoplasia) and persistent or resistant infections (Figure 76-1). Contraction will be delayed in wounds that are under tension or cavitated (indolent “pocket” wounds); surgical intervention may be required to reduce these effects (Figure 76-2). Necrotic or dense fibrotic tissue within the wound bed should be resected to stimulate formation of healthy, vascular granulation tissue. For wounds that are incapable of developing healthy granulation tissue, the blood supply can be improved with omental or muscular flaps or by closure with a vascular skin flap (e.g., axial pattern flap). In acute traumatic wounds, the microbial burden may be substantial. In these cases the role of irrigation is to physically remove the gross contamination. The sterility of the solution and any antimicrobial properties are not as important as its availability in copious volumes. Systematic review of clinical studies evaluating tap water and sterile saline for wound irrigation in humans showed no difference in occurrence of wound infection after tap water or sterile saline irrigation.61 This was verified by a later randomized clinical trial in 715 humans that showed no difference in risk of infection (relative risk, 1.21; 95% confidence interval, 0.5 to 2.7).44 In fact, some studies suggest that tap water reduces the risk for infection. A meta-analysis of six clinical studies in humans showed the odds of infection for wounds irrigated by tap water compared with saline was 0.722 (95% confidence interval, 0.709 to 0.735).43 Thus, initial copious irrigation with tap water is a useful technique to rapidly reduce the contamination burden. Although tap water is hypotonic, it is less so than distilled water. No difference in development of wound infection is evident with use of tap water, distilled water, or boiled water.17 Low-pressure (<5 psi), high-volume irrigation can be generated by devices such as a single-lumen port-type device spiked into a fluid bag. High-pressure irrigation is above 5 to 8 psi; an 18- to 19-gauge needle on a 35-mL syringe can generate 7 to 8 psi. Jet pressure (70 psi) is provided by commercial pulsatile or continuous irrigation devices with a single- or multi-jet tip. Level of pressure that is appropriate for irrigation is unclear. Although irrigation appears beneficial, irrigation pressure is a balance of removal of bacteria and particulate matter versus local tissue damage, lateral fluid and contaminant dissemination, and edema.62 A critical review of irrigation techniques in human and animal models using low-pressure, high-volume irrigation; high pressure; and jet pressure concluded that irrigation was useful but did not find any technique superior.16 Clinicians should balance the effectiveness of high pressure with the consequence of tissue damage when considering the pressure needed for heavily versus mildly contaminated wounds. The role of antimicrobial agents in wound management is based on the route of agent delivery. In general, topical agents are indicated early in wound management to control contamination and reduce microbial burden. Systemic agents are indicated for treatment of wound infection. Topical agents are generally broad spectrum, which is a desirable property because a contaminating microbial population is often quite mixed. Systemic antimicrobial treatment should be narrower in spectrum and is best based on results of culture and sensitivity testing of tissue from the wound. Detection of a positive tissue culture result is consistent with the definition of wound infection. Cultures from swabs of the exudate or surface of a wound are representative of contaminants. Acute wound infections are usually the result of one dominating microorganism. Chronic wound infections are often polymicrobial, and prolonged administration of broad-spectrum antimicrobials usually favors development of resistant microorganisms. In some wound infections, topical and local antimicrobial delivery are used as adjuncts to systemic therapy. Topical antimicrobial agents suitable for immediate wound management include antimicrobial ointments, silver-based dressings, and hyperosmotic dressings (20% hypertonic saline, sugar, honey) (Table 76-1). After application of a topical antimicrobial agent with a contact layer, protecting the wound with a clean, dry bandage (see Chapter 21) is indicated to prevent further contamination and reduce hemorrhage. This also stabilizes the wound area, which improves comfort for the animal and may reduce further trauma. The covering remains in place until definitive treatment can be performed. Application of gauze impregnated with 0.2% polyhexamethylene biguanide into the secondary layer may be indicated to reduce existing microbial burden and further contamination.33,45
Open Wounds
Pathophysiology
Types of Wounds
Thermal Burn
Goals of Wound Management and Wound Classification
Types of Wound Management
Decision Making
Immediate Wound Care
Irrigation Solutions
Antimicrobial Treatment
Wound Protection
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree