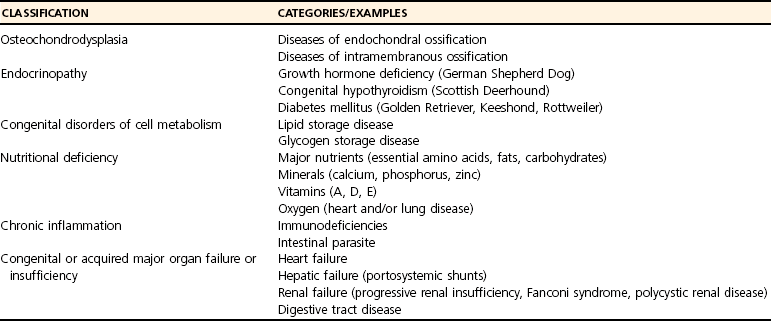
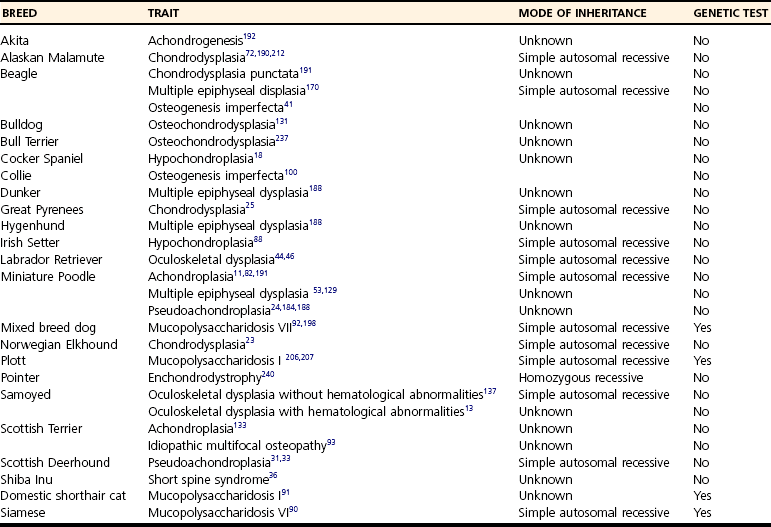
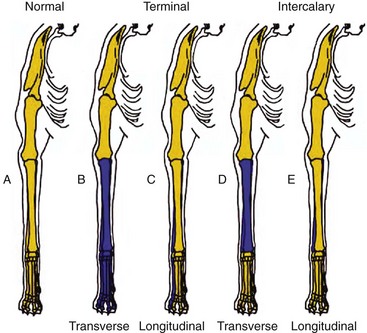
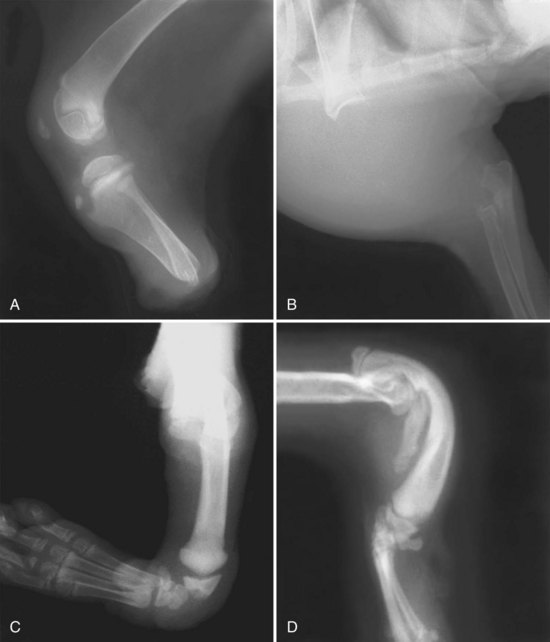
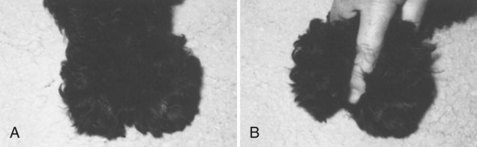
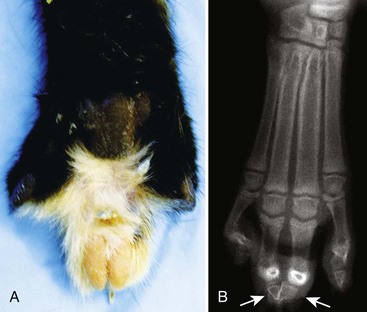
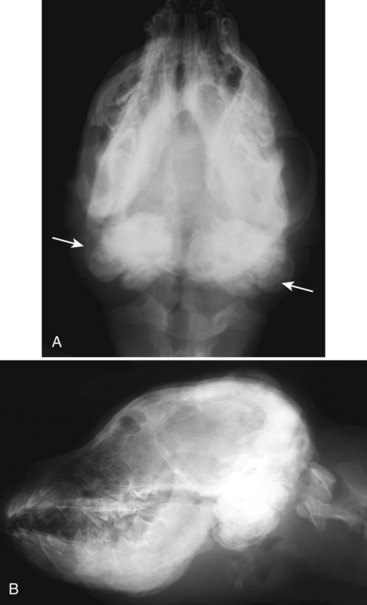
Chapter 69 Constitutional bone and cartilage diseases are identified at or shortly after birth and often have a heritable etiology. They can be broadly classified into osteochondrodysplasias (developmental disorders of chondro-osseous tissue; diseases of endochondral and/or intramembranous ossification) and dysostoses (malformation of individual bones; diseases of mesenchymal bone formation).36,218 Osteochondrodysplasias are a group of heritable bone and cartilage diseases characterized by abnormal endochondral and/or intramembranous ossification. Puppies affected with this condition have retarded growth and a small stature (dwarfism) when they reach skeletal maturation. The term dwarfism refers to small stature. Animals with retarded growth/dwarfism can be proportionate or disproportionate; they are called disproportionate if their legs or trunk is relatively short or long.180 Affected patients must be differentiated from patients with retarded growth/dwarfism secondary to endocrinopathies, congenital disorders of cell metabolism, nutritional deficiencies, chronic inflammation, and congenital or acquired major organ failure or insufficiency (Table 69-1).130 Most endocrine, metabolic, and polysystemic diseases result in proportionate retarded growth/dwarfism, whereas osteochondrodysplasias and nutritional diseases usually result in disproportionate retarded growth/dwarfism.130,180 A minimum database for patients with retarded growth or dwarfism should include a family and nutritional history, complete blood count (CBC), serum chemistry panel, urinalysis, and fecal analysis (parasites). A complete physical examination should be performed to detect concurrent congenital defects. Radiographs of the radius/ulna and lumbar spine are indicated to determine delayed development of epiphyseal growth centers, abnormal growth plate morphology, and reduced length growth of the appendicular and/or axial skeleton. If an endocrinopathy is suspected, serum thyroxine (T4), a thyroid-stimulating hormone (TSH) test, a growth hormone (GH) stimulation test, and/or determination of insulin-like growth factor (IGF)-1 serum concentrations may be indicated.37,180 The presumptive diagnosis of osteochondrodysplasia is usually based on family history, clinical presentation, and radiographic evidence of abnormal endochondral and/or intramembranous ossification. Often multiple littermates are affected. There may be evidence of sex predilection and a history of relatives being affected as well. A hallmark of most osteochondrodysplasias is disproportionate short limbs and retarded growth/dwarfism. Radiographic evidence of a disturbance of endochondral ossification includes delayed ossification of the epiphyseal ossification centers and reduced length growth. Because development of the appendicular and axial skeleton is regulated independently, both sites should be evaluated. Indeed, some osteochondrodysplasias affect only the appendicular skeleton, others affect only the axial skeleton, whereas still other osteochondrodysplasias affect both the appendicular and the axial skeleton. Growth plate histopathology (rib resection, percutaneous growth plate biopsy or postmortem specimen) may confirm or demonstrate growth plate involvement and thus facilitate the establishment of a definitive diagnosis.30,37,180 The underlying genetic defect of osteochondrodysplasias in dogs and cats is rarely known, and a genetic test is available only for mucopolysaccharidosis.162 Thus, molecular diagnostic cues are rarely available to the attending clinician. Because most mutations resulting in osteochondrodysplasias are restricted to a single dog or cat breed, it is more useful to research whether dwarfism in the breed of interest has been reported previously. If dwarfism has been reported, the clinician should then determine whether the patient’s osteochondrodysplasia is similar to the one previously described. Osteochondrodysplasias reported in detail in the veterinary literature are listed in Table 69-2. Canine and feline osteochondrodysplasias reported in other sources are listed in the references (Websites,39,55,156,157 book chapters,36,109,113,191 and lay books51,52). The clinician also may contact the health committee representing the breed of the affected patient.9,10,47 Dysostoses are a group of bone dysmorphologies characterized by abnormal development of individual bones or parts of bones.36 They are caused by failure of the mesenchymal bone model (anlagen) to form, failure of the model to transform into cartilage, or failure to convert from cartilage into bone.154 Many reports have described dysostoses in domesticated animals, but these studies are usually case reports or short case series. Because many dysostoses are not diagnosed, and if diagnosed are not reported, it is difficult to determine the exact incidence of dysostosis in dogs and cats. However, it is clear that the incidence of dysostosis in dogs and cats is low.218 Dysostoses can be broadly separated into appendicular and axial dysostoses. Axial dysostoses include hemivertebrae, block vertebrae, transitional vertebrae, spina bifida, facet aplasia, and dens malformation; axial dysostoses will not be discussed in this chapter.15,239 Examination of a patient with appendicular dysostosis should include a detailed history. The age at which the defect became visible should be determined. The owner should be queried about other affected littermates or affected puppies or kittens from previous litters (including male-to-female ratio) and whether related dogs or cats were affected. Information regarding possible exposure to drugs, maternal disease, or radiation during the first and second trimesters of the mother’s gestation should be obtained, and a nutritional history established. A complete physical examination should be performed because dysostoses may occur in combination with other congenital abnormalities.127,218 The diagnosis of dysostosis is simple and usually is based on clinical and radiographic findings, but sometimes the diagnosis can be challenging. The ability to recognize and differentiate between dysostoses is important because many have treatment options, and in most cases the presence of a dysostosis is compatible with a good quality of life. Early diagnosis may be important for preserving the possibility of effective treatment and reducing secondary complications. It also may be important for preventing further propagation of the condition.218 Following is a nonexhaustive list with description of reported canine and feline appendicular dysostoses. Amelia is the congenital absence of one or more limbs. Monobrachia and abrachia refer to agenesis of one or both thoracic limbs, respectively. Monopodia and apodia indicate absence of one or both pelvic limbs, respectively.99 The diagnosis of amelia is based on physical examination. Radiographs may be used to differentiate between true amelia and a proximal terminal transverse hemimelia (see later). Dogs and cats affected with amelia and reported in the veterinary literature all had concurrent life-threatening conditions. All patients either died spontaneously soon after birth or were euthanized. The trait may be heritable in Beagles.67 Hemimelia is the congenital complete or partial absence of one or more bones. All appendicular bones can be affected, and many variations of this condition have been recognized (Figures 69-1 and 69-2). If all or some of the bones of a limb are absent distal to a certain point, the hemimelia is called terminal (Figure 69-1, B–C). If all or some of the bones of a limb are absent, with the bones proximal and distal to the defect being present, it is an intercalary hemimelia (Figure 69-1, D–E). Each of these two main groups can then be subdivided into transverse hemimelia (complete absence of one or more bones across the limb’s width; see Figure 69-1, B and D) and longitudinal hemimelia (absence of one or more bones along the preaxial [medial] or postaxial [lateral] side of a limb; see the lateral side in Figure 69-1, C and E).77,158 Both terminal8,114,201 and intercalary3,8,127,161 forms of canine3,8,127 and feline 8,127,213 hemimelia have been documented. Most reported hemimelias are single case reports and appear nonhereditary, except for bilateral terminal preaxial pectoral limb hemimelia in Chihuahuas (autosomal recessive trait)8 and perhaps radial hemimelia in Siamese and domestic shorthair cats.103 Radial hemimelia in dog and cats is usually of a preaxial longitudinal intercalary type.109,177 This condition is usually unilateral, but bilateral absence may occur.109 The entire radius or part of it may be absent, and parts of the ulna are sometimes missing as well. Clinical presentation may depend on the type of hemimelia present. The condition may go unnoticed if part of a non–weight-bearing bone such as the fibula or ulna is missing.127 Radial hemimelia is usually noticed soon after birth. Affected patients may exhibit a marked varus and flexure deformity of the elbow and carpus because of the inability of the ulna to support the animal’s full weight and because of an imbalance between flexor and extensor muscles. Over time, the flexor muscles may become permanently contracted.3,49 Pain upon palpation of the distal ulna, lack of forelimb flexion or extension, bone deformity, severe muscle atrophy, and muscle contraction over the entire length of the forelimb may also be noted.3,49 Because of the additional loading, the ulna may assume a larger than normal diameter.49 Concomitant fractures may also be present.3 Radiographs of affected limb(s) will confirm the diagnosis (Figure 69-2).127 Early recognition and treatment of radial hemimelia may prevent muscle contracture, bone deformity with subsequent varus deformity, and/or limb disuse. If a limb deformity can be reduced and the patient is younger than 4 to 5 months of age, we recommend stabilization of the radiocarpal joint in a reduced position with a fortified Robert Jones (splint) or spica bandage.37 The splint is applied to prevent further bone and limb deformity, to allow ankylosis of the radiocarpal joint in a weight-bearing position, and to prevent disuse. If, at 4 to 5 months of age, the function of the affected limb is acceptable and the deformity is minimal, no further care is indicated. If limb function is unacceptable because of the severity of the deformity, or if the patient is older than 4 to 5 months, further conservative or surgical treatment should be considered. Because this condition by itself is not painful, patients treated conservatively usually do not require long-term analgesics. Surgical treatment may consist of declawing of selected digits (if the affected limb is rotated and offending nails get caught in carpet or cause other problems), reconstruction (carpal arthrodesis and repair of the radial defect), or amputation.* Fusion of the defect and carpal arthrodesis have been accomplished successfully using an autogenous rib graft stabilized with a small Kirschner wire or Steinman pin,20,161 and distraction osteogenesis has been used to repair the radial defect.169 Amputation has been suggested for unilateral hemimelia for medical reasons (ulceration, fracture), for financial reasons, or for improved cosmetic appearance. With early diagnosis and appropriate treatment, most patients with unilateral and even bilateral hemimelia will have a very good quality of life.218 Dimelia is the congenital duplication of the whole or part of a limb. Dimelia has been reported in the dog, but not in the cat.119 The diagnosis of dimelia is easily made during physical examination (Figure 69-3). Radiographs are necessary to determine the extent of the bony abnormalities. Paw pressure analysis may help determine which paw is functional and guide surgical planning.119 In patients with minimal or no clinical signs, conservative management, consisting of supportive care, may be the preferred treatment. Surgical treatment of dimelia may depend on the type of duplication that is present. Amputation of the nonfunctional portion of the limb or of the entire affected limb may be considered.119 Ectrodactyly (split-hand deformity, cleft hand, lobster-claw deformity, oligodactyly, or hypodactyly) is a congenital digital cleft formation extending between metacarpal bones (Figure 69-4). In cats, ectrodactyly may be inherited as an autosomal dominant defect with variable expression with no apparent breed or sex predilection.203 No evidence indicates that this trait is heritable in dogs.107 In dogs and cats, most clefts have been reported between the first and second metacarpal bones, but clefts between other metacarpal bones may occur.45 Associated elbow joint incongruity or luxation has been reported.45,107,118 Carpal bones may be hypoplastic or missing, and the ulna may be short. One or more digital rays (metacarpal bone and associated phalanges) may be absent as well. Syndactyly (incomplete separation of interdigital clefts; see later) and digital contractures may be present.45,140 Ectrodactyly is a unilateral disease, affecting only the pectoral limb. Clinical signs vary from mild deformity without lameness to severe deformity and non–weight-bearing lameness. The condition is present at birth, but lameness and deformity may become more severe with age. The malformed limb may be relatively short and may be abducted at the elbow and supinated at the carpus, leaving the carpal dorsum as the weight-bearing surface.79 Carpal laxity may be noticed during examination, and one or more digits, metacarpal bones, and/or carpal bones may be absent. Radiography will confirm the diagnosis, will help determine the extent of the bone abnormalities, and will facilitate the development of a treatment plan.45,79 Early recognition and splinting until the patient is 4 to 5 months of age may facilitate prevention of muscle contracture, bone and limb deformity, and limb disuse, and may promote ankylosis of the radiocarpal joint (see hemimelia).37 If after this treatment limb function is unacceptable, conservative or surgical treatment may be considered. Conservative management may be indicated in mild cases, or if the owner does not want to pursue surgical treatment. With conservative management, patients usually have a good quality of life, and analgesics usually are not needed. Surgical management consists of amputation or reconstruction. Reconstruction may include carpal and metacarpal stabilization with bone grafting; reconstruction of the antebrachium, manus, and soft tissues; and ulnar lengthening.107,110,118 The extent of the malformations will determine the choice of treatment, and multiple corrective surgeries may be required. Results of reconstructive surgery have been encouraging, and reconstruction may be a viable treatment option.107 However, amputation is often selected as the primary method of treatment because of progressive degenerative joint disease, finances, cosmetic reasons, or concurrent neurologic abnormalities.107,110 Prognosis varies depending on the severity of the defect and the treatment options chosen. Polydactyly is defined as the presence of one or more extra digits. Additional digits on the medial side of the extremity are called preaxial, and additional digits on the lateral side of the extremity are called postaxial. Multiple dewclaws are an example of preaxial polydactylism.74,109,205 In most dog breeds, preaxial polydactyly is inherited as an autosomal dominant trait with variable expression.70,74,109 In Saint Bernards and Collies, preaxial pelvic limb polydactylism presumably is an autosomal recessive trait.70,231 Polydactylism in cats is also an autosomal dominant trait with variable phenotypic expression.74 Polydactylism is of clinical significance only if the extra digits become infected or ingrown or catch and tear at the adjoining skin. Amputation of the extra digit(s) may solve such a problem.74 Syndactyly, the congenital lack of differentiation between two or more digits, has been reported in both dogs and cats.78,104,201,203,220 The condition can be classified as simple or complex, and as complete or incomplete.214 In simple syndactyly, the interconnection between adjacent digits on the dorsal surface consists only of skin and fibrous tissue; digital pads on the palmar or plantar surface of the paw may be joined. With complex syndactyly, both soft tissue and bones are fused. Complex and simple syndactyly may be called complete if the digits are connected throughout their entire length (phalanges 1 to 3), or incomplete if the digits are only partially connected throughout their length (Figure 69-5).179,214 Complex syndactyly is also classified as complicated or uncomplicated. Complicated complex syndactyly is associated with other defects, whereas uncomplicated complex syndactyly is not.120,220 Simple syndactyly may cause lameness when the skin on the dorsum of the paw is stretched taut as the digits attempt to spread during weight bearing.179 Complex syndactyly is usually asymptomatic.219,220 The diagnosis is based on orthopedic and radiographic evaluation. Lameness due to simple syndactyly may be treated with surgical separation of the weight-bearing digits. The digits can be separated with large dorsal and palmar skin flaps, and an interdigital commissure can be created; full-thickness skin grafts may be used to cover the exposed axial and abaxial surfaces of the digits.179 No treatment is needed for complex syndactyly.219,220 Hypertrophic osteodystrophy (HOD) is a developmental bone disease in young, rapidly growing dogs. The disease has been referred to as metaphyseal osteopathy, skeletal scurvy, juvenile scurvy, infantile scurvy, Moller Barlow’s disease, and osteodystrophy II.86 The incidence per 100,000 cases has been estimated as 2.8.146 Patients usually present between 2 and 6 months of age.86,146,236 Hypertrophic osteodystrophy predominantly affects large to giant breeds, but any breed can be affected. Great Danes, Chesapeake Bay Retrievers, Irish Setters, Boxers, German Shepherd Dogs, Golden Retrievers, Labrador Retrievers, and Weimaraners are at increased risk.121,146 Male dogs are 2.3 times more likely to develop hypertrophic osteodystrophy than female dogs.146 The incidence of hypertrophic osteodystrophy was found to be highest in the Northeastern United States, and was highest in the fall and lowest in the winter.146 Histologic evaluation of a longitudinal slab of an affected bone reveals a zone of disrupted trabeculae in the metaphysis immediately adjacent and parallel to the growth plate, corresponding with the metaphyseal lucency seen on radiographs. A collar of bone may be noted around the metaphysis. At higher magnification, the growth plate may have an irregular thickness. The zone with trabecular disruption is characterized by hemorrhage and hemosiderin deposits, necrotic trabeculae, inflammatory cells, and fibrosis. Subperiosteal hemorrhage with or without reactive formation of new bone may be seen.86,124,145 Proposed causes include vitamin C deficiency, overnutrition, heritability, infection, and vaccinations. The original reports on vitamin C deficiency and overnutrition were largely circumstantial136,236 and have been refuted in later studies.86,243 Heritability has been suggested as an etiologic factor in breeds at increased risk for hypertrophic osteodystrophy.1,19,89,146,243 Hypertrophic osteodystrophy has been reported in a litter of Weimaraners; the estimated heritability was 0.68.1 It also has been suggested that infection is associated with hypertrophic osteodystrophy because many patients have a history of or have systemic illness in addition to leukocytosis. In one dog diagnosed with hypertrophic osteodystrophy, positive blood cultures for Escherichia coli were demonstrated.199 However in most studies, an infectious process was not identified.101,146,236 Canine distemper virus transcripts have been detected in the metaphyses of dogs with hypertrophic osteodystrophy, suggesting an association between hypertrophic osteodystrophy and canine distemper virus.135 In a large, multi-institutional study involving 16 veterinary teaching hospitals, the finding of only 2 of 131 cases with concurrent disease and the dissimilarity of risk factors for hypertrophic osteodystrophy and canine distemper virus did not support a direct relationship between hypertrophic osteodystrophy and canine distemper virus.146 Systemic hypertrophic osteodystrophy was demonstrated in 5 of 6 Weimaraner puppies, among which 5 of the puppies were genetically related. All puppies developed clinical signs within 10 days of administration of a modified live vaccine containing canine distemper virus and canine adenovirus type 2.1 Results of a later study in Weimaraner puppies suggested that the vaccination protocol affected the pattern of appearance of hypertrophic osteodystrophy.56,89 It has been hypothesized that hypertrophic osteodystrophy in Weimaraners is due to an inherited immunodeficiency with low concentrations of circulating immunoglobulins.56,73 Thus, hitherto no single unifying cause of hypertrophic osteodystrophy has been determined.5,86,146 Diagnosis is based on signalment, history, and clinical signs, and is confirmed by radiographs. The disease can affect any bone. The distal radius, ulna, and tibia are the most commonly affected bones, but hypertrophic osteodystrophy has also been identified in the mandible, maxilla, skull, vertebra, scapula, humerus, femur, and ribs.101,146 Clinical signs include swelling of the metaphyseal region(s) of affected bone(s); lesions often are bilateral.86 The swellings can be warm upon palpation and are accompanied by varying levels of discomfort and lameness. Patients can range from mildly lame to reluctant to walk or stand.5 Systemic clinical signs may include hyperthermia, depression, inappetence or anorexia, and diarrhea.5,86,146,236 In severely affected dogs, particularly immunosuppressed Weimaraner puppies, blood culture to detect possible bacteremia is indicated.1,199 The diagnosis is confirmed radiographically. Pathognomonic radiographic signs include a lucent line in the metaphysis parallel to a narrow zone of increased radiodensity immediately adjacent to the physis. Periosteal and endosteal proliferation may be observed. In more advanced stages, radiographs may demonstrate excessive enlargement of the metaphyses, which also has been referred to as flare and metaphyseal collar of bone. Although the epiphysis and growth plates are usually normal, irregular widening of the growth plate can occur as the disease progresses (Figure 69-6).* Differential diagnosis includes secondary nutritional hyperparathyroidism, septic polyarthritis, trauma, retained cartilaginous cores, and hypertrophic osteopathy. For Newfoundlands, metaphyseal dysplasia with irregularities of the radial and ulnar growth plates also should be considered.221–223 In most cases, hypertrophic osteodystrophy is self-limiting within days to weeks but may persist for months. The prognosis is good to excellent in mild cases, but in severe cases, death can occur.5,146 In mildly affected dogs, analgesics are indicated and a balanced canine diet should be provided. In more severely affected dogs, treatment consists of supportive care, especially for patients that are reluctant to eat, recumbent, and hyperthermic. It has been suggested that Weimaraners with severe systemic hypertrophic osteodystrophy without bacteremia may respond better to corticosteroids than to nonsteroidal antiinflammatory drugs (NSAIDs).1 Blood cultures and treatment with antibiotics are indicated in dogs with bacteremia. One or more recurrences can develop weeks to months after an episode.5,19,124 As the condition regresses, the radiolucent zone and the periosteal reaction remodel and resolve. However, with recurrence, a new radiolucent line and periosteal reaction will appear.5 In severe hypertrophic osteodystrophy cases, carpal or tarsal valgus limb deformity may develop. Deformity is probably secondary to excessive metaphyseal bone formation with subsequent bridging of the physis or synostosis between radius and ulna. Thus, in severe cases, owners should be warned of the possibility of angular limb deformity.19,124,223 Panosteitis is a self-limiting inflammatory disease of the bone marrow of long bones. Panosteitis is also referred to as enostosis, eosinophilic panosteitis, and shifting leg lameness.27 The incidence of panosteitis has been estimated as 2.6 per 1000 patients.111 In a case-control study of 1220 cases and 6100 controls using records from 16 veterinary teaching hospitals over a 10-year period, breed, age, weight, gender, and season were identified as risk factors.32 Breeds at increased risk include Airedale Terriers, Irish Setters, German Shorthair Pointers, Doberman Pinschers, Afghans, Great Danes, Saint Bernards, Bernese Mountain Dogs, Newfoundlands, Mastiffs, Bassett Hounds, Rottweilers, American Cocker Spaniels, Chinese Shar Peis, Golden Retrievers, Labrador Retrievers, German Shepherd Dogs, and mixed-breed dogs.27,32,121,208,226 Thus, panosteitis is predominantly a disease of large- to giant-breed dogs, but the condition has been reported to affect smaller breeds, such as the Miniature Schnauzer and the Scottish Terrier. Most panosteitis patients are between 5 and 12 months of age; however, age can vary from 2 months to 5 years.27,32 The mean age at the time of diagnosis in a study of 100 affected dogs was 12.4 months.27 Males are affected more frequently than females by a ratio of 4 : 1.27 Among young dogs that weighed over 23 kg, females were at three times and males at five times increased risk compared with young dogs weighing less than 23 kg.32 The incidence of panosteitis was higher in the North Central and Northeastern regions of the United States, and highest in summer and fall.32,126 The first histologic changes of panosteitis consist of empty spaces in the adipose bone marrow, vascular proliferation, and local bone formation around the nutrient foramen.226 These changes are associated with vascular congestion and increased intraosseous pressure (25 to 54 mm Hg; normal value, 6 to 24 mm Hg).193,226,242 Congestion results in further local bone formation, secondary periosteal bone formation, and enlargement of the haversian system. Over time, areas of local bone formation coalesce and become connected to the endosteum. Then, remodeling of newly formed bone commences and hematopoietic bone marrow reappears, followed by replacement with adipose bone marrow.226 The origin of panosteitis is poorly understood, but it has been suggested that increased intraosseous pressure is due to protein accumulation.193,194 Diagnosis is determined by signalment, history, and clinical signs; radiographs add supporting evidence. Hallmarks of this condition include shifting leg lameness and pain on palpation of affected long bones.126,226 Clinical signs vary from mild lameness to inability to walk. The lameness can be acute, and there is no history of trauma. The ratio of forelimbs to hindlimbs affected is 4 : 1.32,226 Bones commonly affected include ulna (42%), radius (25%), humerus (14%), femur (11%), and tibia (8%).226 Firm palpation of affected bones, with care to avoid compressing muscles or nerves, often elicits marked pain. Multiple bones can be affected at the same time, and owners often report “shifting” leg lameness that can resolve without an apparent cause.226 Radiographs are necessary to differentiate this condition from other common conditions of young growing canines that can occur concomitantly, such as hypertrophic osteodystrophy, osteochondritis dissecans, hip dysplasia, or elbow dysplasia. Radiographic signs depend on the stage of the disease. In the early stage of the condition, radiographs may be normal, or a decrease in radiodensity may be evident in the medullary cavity near the nutrient foramen. This is rarely seen. The next stage involves an increase in medullary opacity with a granular pattern or with loss of the normal trabecular pattern (Figure 69-7). Periosteal bone formation, laminar or smooth, may be observed as well. As the lesion progresses, the medullary canal becomes more diffuse and homogenous. After 4 to 6 weeks, the densities regress, leaving a trabecular pattern that is coarser than normal. Generally, no association is noted between radiographic severity, patient discomfort, and degree of lameness.27,211,126,226 Angiography, thermography, scintigraphy, and magnetic resonance imaging (MRI) also have been used to study panosteitis.117,180,193 Treatment does not appear to influence eventual outcome. Treatment consists of rest and analgesics. It has been reported that in a pilot study, treatment with a proteolytic substance called benzopyron resulted in normalization of intraosseous pressure and clinical remission within days.193 However, these findings have not been substantiated, and this drug is not available in the United States. Recurrence of clinical signs is possible, but the severity of the episodes usually decreases while the intervals increase.27,126,180 Craniomandibular osteopathy is also referred to as craniomandibular osteoarthropathy, craniomandibular osteodystrophy, mandibular periostitis, lion jaw, Westie jaw, and Scotty jaw. The incidence of craniomandibular osteopathy has been reported as 1.4 per 100,000 cases, with the incidence being higher in the Western region and in the Southern plains of the United States.146 No evidence indicates seasonal fluctuation of the incidence of the disease. Male and female dogs are at equal risk for the disease, and weight at the time of initial diagnosis does not appear to be a risk factor. Puppies younger than 6 months of age are at highest risk. Most patients are younger than 12 months of age, and a decrease in the incidence of craniomandibular osteopathy occurs with increasing age.146 Cairn Terriers, West Highland White Terriers, and Scottish Terriers have been most commonly diagnosed and are at increased risk.121,146 A nonexhaustive list of other affected breeds includes Boxers, Labrador Retrievers, Great Danes, Boston Terriers, Shetland Sheepdogs, German Wirehaired Pointers, German Shepherd Dogs, Great Danes, and Doberman Pinschers.* Strong breed predispositions suggest a heritable etiology, and an autosomal recessive mode of inheritance has been demonstrated in West Highland White Terriers.61,160 Craniomandibular osteopathy is characterized by unilateral or bilateral symmetric irregular osseous proliferations of mostly the mandibles and/or tympanic bullae. Temporal bones and/or other cranial or long bones also may be affected.61,183,238 Osteoclastic resorption of lamellar bone is followed by the presence of primitive bone that expands beyond the periosteum of the affected bone. Normal bone marrow is replaced by a highly vascular fibrous-type stroma. The borders of the lesions are invaded by inflammatory cells (lymphocytes, plasma cells, and neutrophils), and adjacent connective tissue and muscle fibers are destroyed.185 Clinical signs vary from minor difficulty prehending and chewing to complete inability to open the mouth and inability to eat and drink. Additional clinical signs include salivation, intermittent hyperthermia, depression, weight loss, salivation, inappetence to anorexia, variable levels of pain while eating, exophthalmia, and strabismus.60,132,200 During physical examination, enlargement or irregularity of the mandibles may be palpated, and the patient’s mouth may be able to be opened only partially or not at all because of enlargement/fusion of the angular processes of the mandible and tympanic bullae.183 Mandibular lesions can be unilateral or bilateral.238 Diagnostic evaluation includes CBC, serum chemistry panel, urinalysis, radiography, and fine needle aspirate/biopsy for histopathology and culture. CBC and serum chemistry profile are often unremarkable. Diagnosis is based on signalment, clinical findings, and demonstration of bony proliferation on the mandibles or tympanic bullae, which may require oblique radiographic views of the skull. The teeth are unaffected. Temporal bones, frontal bones, maxillary bones, and/or other cranial or long bones also may be affected (Figure 69-8).146,200 Computed tomography may be used to identify lesions at an earlier stage of disease and to better delineate the lesions.105 Bony proliferation is nonneoplastic on cytology and/or histopathology results.160 Differential diagnosis includes metabolic bone disease (see later), osteomyelitis, and neoplasia. The disease may become self-limiting when the dog is approximately 11 to 13 months of age. However, patients may need variable levels of supportive care, which may include feeding of soft food, gruel food, or syringe-fed food and/or placement of a feeding tube to overcome the period of incapacitation. Nutrition and hydration must be carefully monitored. Analgesics are often indicated. Patients may be treated concurrently with antibiotics and steroids or NSAIDs during febrile episodes. The benefit of these treatments is variable and is potentially coincidental with natural regression of the disease.61 Over time, bony proliferations often regress completely or partially. Surgical excision of the proliferation has been attempted, but lesions can return within 3 weeks.165 Rostral hemimandibulectomy has been used as a salvage procedure in a patient unable to open her mouth because of chronic bilateral involvement of the mandibles and tympanic bullae. The procedure facilitated lapping of food and subsequently allowed weight gain.238 Euthanasia has been performed for patients with uncontrollable discomfort and with lesions that do not resolve sufficiently to allow the patient to eat, as well as in cases where owners were unable to provide supportive nutritional care and palliative analgesia.183 Retained ulnar cartilaginous cores are cones of growth plate cartilage that project from the distal ulnar growth plate into the distal metaphysis. They are also called retained endochondral cartilage cores132,182,211 and consist of viable hypertrophic chondrocytes. Retained hypertrophic chondrocytes represent failure of the growth plate cartilage to convert to metaphyseal bone. This condition occurs predominantly in large to giant, immature canines.112 It has been suggested that this condition is a growth plate manifestation of osteochondrosis.155,248 If a retained cartilage core is associated with reduced ulnar length growth, cranial bowing of the radius, rotation and valgus deviation of the forepaw, and subluxation of the carpal and elbow joints may be seen. Patients may suffer identical forelimb deformities as are seen with premature closure of the distal ulnar and radial growth plates.110,112,182 Radiographs are indicated to determine the cause of the deformity.110,112 No correlation has been noted between size of the lesion, histopathology, and severity of forelimb deformity. Radiographs reveal a radiolucent core (triangle) of cartilage in the distal ulnar metaphysis that may be surrounded by a zone of sclerosis.110,112 The core can extend 3 to 4 cm proximally into the metaphysis (Figure 69-9).182
Miscellaneous Orthopedic Conditions
Constitutional Bone and Cartilage Diseases
Osteochondrodysplasias
Dysostoses
Amelia
Hemimelia
Dimelia
Ectrodactyly
Polydactyly
Syndactyly
Pediatric Bone Diseases
Hypertrophic Osteodystrophy
Panosteitis
Craniomandibular Osteopathy
Retained Ulnar Cartilaginous Core
< div class='tao-gold-member'>
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Miscellaneous Orthopedic Conditions
Only gold members can continue reading. Log In or Register to continue