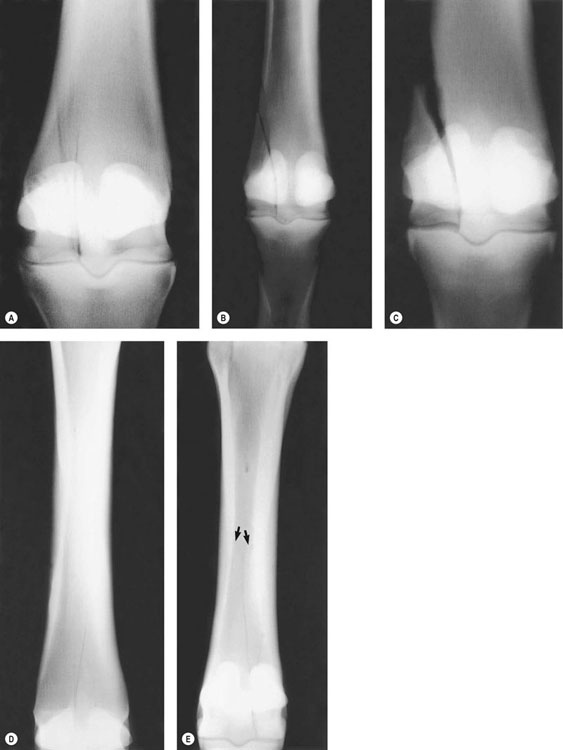
• These problems are common in young Thoroughbreds and Quarter Horses in early race training. • Bilateral dorsal metacarpal swelling, heat and pain, with stiffness/soreness or ‘choppy-gaited’ lameness are common symptoms. • Acute onset may follow a high-speed workout (‘breeze’) or first race. • Treatment involves anti-inflammatory therapy, rest and controlled exercise, and modified training. • Prevention involves modification of the training regimen. • Prognosis is generally very good to excellent and recurrence is rare in skeletally mature horses. • Horses that develop clinical ‘bucked shins’ are at risk for dorsal cortical stress fractures in the future. Horses with ‘bucked shins’ exhibit variable degrees of soft tissue swelling, heat and sensitivity on palpation over the dorsal diaphyses of MC-III. When viewing the metacarpi from the lateral aspect, there is often a distinct dorsal convexity. Firm digital pressure in this location will elicit a painful response. These signs are particularly pronounced in the acute stages, but after a period of rest and anti-inflammatory treatment, there is generally considerable improvement. The exceptions are horses that have progressed to the chronic or ‘recurrent’ category and have developed a marked periosteal reaction along with chronic inflammation and associated soft tissue swelling. Less commonly, a more focal area of swelling may be present at some point along the dorsal diaphysis,1 which must be differentiated from a true stress fracture (see section below). Horses with acute ‘bucked shins’ typically exhibit a bilateral stiff or choppy forelimb gait at a trot (sometimes mimicking a foot or carpal lameness), but in those in which one metacarpus is more severely affected than the other, a distinct head nod may be evident. Lameness in these horses ranges from grade 1 to 3.2 The most severely affected horses may acutely exhibit mild lameness at the walk. The severity of the lameness will vary greatly with the stage of the disease and the timing of the examination in relation to the last speed work. Radiographic findings vary with each case and the stage of disease. Radiographs in mildly affected horses or in the very early stages of the disease (subclinical) are often negative or equivocal for osseous abnormalities. In more severely affected horses, diffuse subperiosteal osteolytic change in combination with smooth, low-density periosteal proliferative reaction is typically seen along the dorsal and dorsomedial diaphysis of MC-III (Fig. 16.2). High-detail digital radiographs are superior for detecting the subtle abnormalities. Soft tissue swelling, when present, will also be evident radiographically in this location. The use of NSAIDs for their anti-inflammatory and analgesic effects in patients with inflammatory bone disorders is controversial in light of the gathering body of evidence that these drugs, when used chronically at high doses, may impair bone healing in horses.5 However, it is this author’s opinion that a brief period (i.e. a few days) of NSAID treatment during the acute stage of ‘bucked shins’ is warranted in horses with moderate-to-severe signs. Phenylbutazone or flunixin meglumine at standard doses is generally effective. Long-term NSAID treatment is contraindicated, in this author’s opinion, for the reasons noted above. The key to preventing ‘bucked shins’ is to stress the dorsal cortices of the developing metacarpi in such a way as to stimulate adaptation to the cyclic compressive loads under conditions that are similar to those experienced during a race, i.e. to train at racing speeds.6 Traditional training strategies for flat-racing Thoroughbreds have employed a basic scheme of daily galloping exercise for extended distances (e.g. 1–2 miles) with speed work or ‘breezes’ at shorter distances (e.g. 2–6 furlongs) weekly to every third week. In immature (untrained) horses the timing (too infrequent) and distance (too long) of the high-speed work sets up a state of maladaptive remodeling in which bone resorption outpaces apposition and fibrous periosteal new bone predominates.6 Eventually, this inferior bone develops microfractures and resulting inflammation, which manifests clinically as periostitis or ‘bucked shins’. To prevent or mitigate the potential for this vicious cycle, horses should be trained in such a way as to increase the frequency of high-strain cyclic compressive loading (high-speed exercise or ‘breezes’) and decrease the total distance at which they are galloped.6 It is recommended that horses be worked at or near racing speed at least twice a week, initially at very short distances, for example one furlong. The distance of the speed work is increased gradually (e.g. adding one furlong every 1–2 weeks) and then as the horse is asked to go faster, the distance is reduced and the process repeated until the horse is conditioned to race. Throughout this process, daily galloping is limited,6 for example to no more than one mile/day. Upon resumption of training, horses are continually monitored for signs of ‘shin soreness’, lameness or dorsal metacarpal swelling and exercise intensity should be modified accordingly. The prognosis for the vast majority of horses with ‘bucked shins’ is generally very good if appropriate intervention is undertaken and adhered to. Recurrence is rare; however, a variable proportion of horses will experience repeated episodes or ‘chronic’ DMD. Horses not given adequate convalescence and those that have not had their training protocol modified (see above) are at high risk for recurrence. ‘Bucked shins’ is quite rare in older horses (>4 years of age)7 once the immature bone has remodeled and changed its inertial properties in response to the demands of high-speed exercise. However, horses that have experienced clinical ‘bucked shins’ as two or three year olds are in the high-risk group for dorsal cortical stress fractures (see section below).8 Historically, DMD and, more specifically, ‘bucked shins’ have been and continue to be an extremely common problem in young flat-racing horses in early training. In the US, a prevalence of 65–70% in Thoroughbreds has been reported12,13 and in Australia the prevalence has been estimated at 42–80%.14–16 Similarly, estimates of 5–50% have been given for the prevalence in racing Quarter Horses in the US.17 DMD also affects racing Arabians. In contrast, the incidence of DMD is comparatively low in the UK, with an estimate of 17% in young Thoroughbreds in one large study.10 This difference could be attributed to a number of variables, but differences in training surface (predominantly grass in the UK and predominantly dirt in the US) are regarded by many to be a primary factor.9 In stark contrast is the very low incidence of DMD in Standardbred racehorses.12 This has been attributed to differences in speed and gait between Standardbreds and Thoroughbreds, which result in different strains imposed on MC-III, and not to an inherent difference in bone material properties between the breeds.18 The most effective way to prevent or decrease the incidence of ‘bucked shins’ is to modify the training scheme as outlined previously (see under Therapy). Essentially, this involves decreasing the daily distance worked at a gallop and increasing the frequency of short intervals of high-speed work or ‘breezes’. The distance of the speed work is initially very short and is increased gradually.19,20 Different training surfaces may also affect the incidence of ‘bucked shins’. Training on woodchip-based surfaces or grass appears to be superior to the traditional dirt of most tracks in the US.9,10 For example, in one two-year study of Thoroughbred racehorses, 55.8% of those trained on dirt experienced ‘bucked shins’ compared to only 26.1% of those trained on a woodchip-based surface.9 This study did not rigidly control for differences in training methods, however. Prevention also involves close monitoring of the horse for signs of impending shin problems. Along with physical examination for shin soreness, thermography and scintigraphy are useful imaging modalities for screening high-risk horses. In one study, pre-race detection using physical examination to screen horses for signs of DMD resulted in reduction in post-race diagnoses of lameness attributable to DMD, and more predictable race results, on Thoroughbred tracks in Australia.11 More recent work has demonstrated significant increases in biochemical markers of bone turnover in horses in early training that ultimately developed signs of DMD.21 However, the use of these measurements in the clinical setting remains only theoretical at this point. • Fatigue fractures are seen in racing Thoroughbreds, Quarter Horses and Arabians. • Horses experiencing previous ‘bucked shins’ are at high risk. • Short, oblique, intracortical fracture are seen most commonly in the mid-diaphysis of the left MC-III (in Thoroughbreds in the US). • Acute onset of moderate-to-severe lameness may follow high-speed work (‘breeze’) or a race. • Fractures are often slow to heal and chronic or recurrent. Fractures are common if initially undiagnosed or mismanaged. • Surgical treatment is preferred for the majority of fractures and involves osteostixis, screw fixation, or a combination of the two. • Prognosis is generally very good for return to racing. Some horses may become sound enough to train or even race after extended rest, but continue to be plagued by recurrent lameness and poor performance. This is a common scenario for those with chronic stress fractures that have gone undiagnosed. Almost all horses with dorsal cortical stress fractures of MC-III will have a history of clinical ‘bucked shins’ in the 6–12 months preceding the fracture.20 For horses with acute fracture, physical examination will classically reveal a focal area of soft tissue swelling along the dorsum of the metacarpus at the site of the fracture, with a corresponding bony ‘knot’ or periosteal irregularity (hard swelling or exostosis) along the dorsal or dorsolateral diaphysis of MC-III. Firm digital pressure at the fracture site will consistently elicit a painful response. These signs are less dramatic in horses with chronic or subacute fractures. Horses with multiple fractures may have signs more suggestive of ‘bucked shins’ (i.e. diffuse pain and swelling along the diaphysis). Fractures are almost always unilateral in Thoroughbreds (in contrast to ‘bucked shins’) and involve predominantly the left forelimb in the US.22–25 Bilateral fractures occur, but are rare. Acutely, horses exhibit a moderate-to-severe lameness on the affected limb, which is typically grade 3–4.2 Many are lame at a walk and all are profoundly lame at a trot. With a brief period of rest (a few days to a few weeks), horses generally walk comfortably but exhibit a mild-to-moderate lameness at a trot in-hand (grade 2–3). Horses with chronic fractures may exhibit only mild lameness at a trot in-hand. Firm pressure applied over the fracture site will exacerbate the lameness in most acute and subacute cases. Bone-phase (delayed-phase) nuclear scintigraphy will reveal a focal (or multifocal in horses with multiple fractures) area of moderate-to-intense abnormal increased radiopharmaceutical uptake in the dorsal diaphysis of the affected MC-III in acute and subacute cases (Fig. 16.3). The intensity of radiopharmaceutical uptake will be less intense in chronic cases and will vary with the time course of the injury.3 The classic radiographic abnormality is a short, oblique intracortical (unicortical) fracture line in the dorsal or dorsolateral cortex of MC-III (Fig. 16.4). Most commonly the fractures are diaphyseal and are oriented dorsodistal to palmaroproximal at a 30–45° angle with the dorsal cortex. Most extend to the junction of the middle and palmar third of the dorsal cortical width and do not enter the medullary cavity. Occasionally, a complete fracture will extend proximodorsally out through the dorsal cortex (a true saucer fracture’). Metaphyseal fractures, those that begin and propagate in a dorsoproximal-to-palmarodistal direction, and those that enter the medullary cavity are less common. A full series of radiographs (four views: lateral, dorsopalmar, DMPLO and DLPMO) of the entire MC-III should be taken. Multiple fractures are sometimes present. In rare cases fracture lines may propagate or radiate away from the primary fracture site.26 The majority of fractures are oriented in a frontal or near-frontal plane, but occasionally sagittally oriented fractures are seen.27 Variable degrees of periosteal and endosteal callus may be present, as will soft tissue swelling and more diffuse osteolytic and proliferative periosteal reaction associated with previous ‘bucked shins’ in many horses. There is debate among clinicians regarding the merits of surgical and non-surgical management of dorsal cortical stress fractures of MC-III. These fractures are notorious for being slow to heal or for following an unpredictable course between horses.12,19 Fractures in younger horses (two and three year olds), those that enter the medullary cavity or that involve the metaphyseal regions are the most likely to heal expediently without surgical intervention. In general, this involves a period of 3–4 months of controlled exercise; however, it is not unusual for some fractures to require 4–6 months or longer for satisfactory healing.28 When non-surgical management is chosen, 4–6 weeks of stall confinement with daily hand-walking is recommended. This is followed by 6–8 weeks of controlled exercise in the form of small paddock turnout or very light jogging. Some form of controlled exercise is important to stimulate remodeling and fracture healing.22,23 Complete cessation of exercise for a prolonged period (e.g. long-term stall confinement) favors the development of a chronic fracture (i.e. a delayed or non-union). Follow-up radiographs should be taken every 4–6 weeks to assess healing before increasing the intensity of exercise or for determining whether surgical intervention is warranted (to overcome delayed healing). Follow-up scintigraphic scans can also help in making these decisions.3 A radiographically visible fracture exhibiting low or diminishing scintigraphic activity would warrant strong consideration as a candidate for surgery. Drill bit preference varies with surgeon but 2.5–3.5 mm diameter bits are appropriate. Smaller bits (e.g. 2.0 mm) are more easily broken in the standing patient and larger holes may unnecessarily weaken the bone, as does an excessive number of holes.27 Distance between holes should be kept at approximately 1.0 cm. A large number of holes placed close together can result in sequestrum formation or resorption of a core of bone or significantly weaken MC-III.29 Copious lavage during drilling, and frequent cleaning of the bit, are important to minimize the potential for the bit to break. After final radiographic confirmation of adequate hole placement the incisions are closed routinely and a padded bandage is applied. Horses are confined to a box stall for a total of 4–6 weeks following surgery. Skin sutures are removed 12–14 days postoperatively, at which time daily hand-walking exercise should commence. A bandage is maintained for 2–3 weeks after surgery. After this period of stall confinement and hand-walking, horses are allowed daily turnout exercise in a small paddock for four weeks. If at that point follow-up radiographs reveal good progression of healing, daily light jogging exercise can begin. Harder training should not commence until fractures have sufficiently healed radiographically. Drill holes may persist radiographically for many months (beyond the point of fracture healing), even while horses are training at speed. Based on studies in other species30 and on clinical observation in horses,23 it is assumed that these holes should no longer act as stress risers by that stage. Osteostixis is believed to accelerate or promote healing by facilitating access of mesenchymal cells and other osteogenic medullary elements to the fracture line.7,31 The ‘cores’ of new bone that form across the fracture line may act to stabilize the fracture and further promote healing.32 Osteostixis may also stimulate fracture healing through activation of the ‘regional acceleratory phenomenon’.33 If osteostixis is to be employed along with screw placement, the surgical approach is identical to that described above. If a single screw is being used without osteostixis, a smaller (~1.0 cm) ‘stab’ incision can be used. A 3.5 or 4.5 mm ASIF cortex screw is appropriate. Although screw insertion using the lag technique has been described, the majority of surgeons place these screws in a positional (‘neutral’) fashion. The latter approach is technically easier and the results are comparable. Regardless of the technique, either compression (‘lag screw’) or positional (‘neutral’), screws are placed in a unicortical manner. Transcortical screws that engage the palmar cortex are contraindicated and no longer recommended, as they are associated with a higher incidence of osteolysis around the implant and implant-associated pain,12 as well as fracture and the risk of suspensory ligament damage during placement.34 Standard ASIF techniques are employed for drilling, tapping and countersinking. Screws should be placed as close to perpendicular to the fracture line as possible (Fig. 16.5). Osteostixis, if employed, is then performed as previously described and the incisions are closed routinely. Bandaging and initial aftercare are similar to that described for osteostixis. Screw removal is usually performed between two and three months after surgery. Proponents of the combination of a positional screw and osteostixis feel that two months is generally adequate.22 The decision for screw removal is based on adequate progression of healing on follow-up radiographs. Screws are removed with the horse standing and using sedation and local anesthesia. An additional period of controlled exercise is recommended before resuming training following screw removal. This period varies from 2–8 weeks.22,35 Unicortical screws in the dorsal cortex of MC-III do not cause pain in all horses upon resumption of training and return to racing.34 However, screw removal in the early postoperative phase (i.e. at the 2–3 month point) obviates the need to take the horse out of training if pain develops and it eliminates the screw being implicated as the cause for any number of unrelated problems in the future. The benefits of interfragmentary screw compression (‘lag screw’ technique) in fracture healing are quite clear and well understood. The mechanisms by which a neutral or positional screw acts specifically to promote or accelerate healing of stress fractures of the dorsal cortex of MC-III remain incompletely understood. In one uncontrolled study,22 dorsal cortical stress fractures of MC-III treated surgically by a combination of screw fixation using a positional (non-compression) screw and osteostixis were reported to heal faster (95% of fractures healed in two months) than fractures treated with osteostixis alone (3–4 months for radiographic healing).23,25 Differences in postoperative exercise regimens between studies may have influenced the results, but interfragmentary stabilization and the ‘regional acceleratory phenomenon’ have been proposed as mechanisms by which screws facilitate fracture healing over osteostixis alone.22 The prognosis for horses to return to racing following healing of dorsal cortical stress fractures of MC-III is generally very good. Eighty-two to 89% of Thoroughbreds in the US returned to race at least once following osteostixis.23–25 One report on the outcome following screw fixation and osteostixis in Thoroughbreds indicated that 94% raced at least once postoperatively.22 The majority of horses in all studies returned to compete at their prefracture levels. A small percentage of horses experience repeat fracture or new fractures upon resumption of training and racing, regardless of treatment modality.22,23 Recurrent fractures presumably result from inadequate healing (i.e. delayed union) and this may occur up to a year or more following treatment and return to training. New fractures developing at the site of an osteostixis hole have been reported.23 Development of new fractures may also be related to training methodology in these horses (see below). Catastrophic fracture upon resumption of training and racing, although uncommon, has also been reported in Thoroughbreds.24 Dorsal cortical stress fractures of MC-III are a classic example of fatigue fractures that result from failure of bone to adapt to accumulated high-strain cyclic loading.36,37 The reader is referred to the chapter on stress-induced bone disease and maladaptive remodeling syndromes (Chapter 23) for a detailed discussion of this topic. See the previous section on ‘bucked shins’ for additional details of the epidemiology of DMD. Almost all Thoroughbreds with dorsal cortical stress fractures of MC-III experience a previous episode of clinical ‘bucked shins’20 and the same observation has been made in Quarter Horses.1 It has been estimated from older studies that 10–15% of Thoroughbreds which develop ‘bucked shins’ will go on to experience a true stress fracture in 6–12 months.12,20 Therefore, this subgroup of DMD cases in Thoroughbreds is slightly older than the ‘bucked shins’ group, typically 3–5 years of age, but even horses older than five occasionally present with this injury. In contrast, dorsal metacarpal stress fractures in Quarter Horses are seen predominantly in two year olds.1 In Thoroughbreds, these fractures appear to be more common in males than females,21–25 but whether this simply reflects a referral bias or a true physiologic difference between males and females remains incompletely understood.23,38,39 Fractures most commonly involve the left forelimb in Thoroughbreds in the US (72–91%).22–24 This has been attributed to increased strains on this limb as a result of the counterclockwise direction of racing in this country. • Condylar fractures are high-speed injuries affecting racehorses of all breeds. • The lateral condyles in the forelimbs of young Thoroughbreds are most commonly affected. • Condylar fractures are presented as an acute injury during or shortly after a race or workout. • Horses are markedly lame and clinical signs are highly consistent with a fetlock injury. • Surgical treatment involves interfragmentary screw compression. • Some non-displaced fractures can be managed non-surgically with a favorable outcome. • The prognosis for return to racing for most horses with non-displaced lateral condylar fractures is favorable. • The prognosis for most horses with displaced lateral condylar fractures is guarded. • Medial condylar fractures are associated with a significant risk for catastrophic fracture of the affected bone. • Treatment of medial condylar fractures may necessitate supplemental internal fixation to mitigate catastrophic failure. • The prognosis for future athletic soundness for most horses with medial condylar fractures is favorable if catastrophic fracture is avoided. Condylar fractures are common high-speed injuries in racehorses of all breeds.40–45 However, they most commonly affect the lateral condyle of MC-III in Thoroughbreds41,44,45 and are only rarely seen in non-racehorses. Fractures can involve the medial or lateral condyles. Lateral fractures are categorized as incomplete, complete/non-displaced or complete/displaced. Medial condylar fractures fall into three categories: ‘short’ (simple, sagittally oriented fractures involving only the distal metaphysis/diaphysis); ‘spiral’ (fractures that propagate proximally in a spiral configuration and remain a simple fracture); and ‘Y fractures’ (long sagittal fractures that abruptly change configuration or direction in the mid-diaphysis) (Fig. 16.6). The vast majority of horses are not able to continue training. On rare occasions a horse with a chronic fracture (generally short and incomplete) will be presented with a history of recurrent lameness and/or poor performance that is exacerbated with exercise. Some horses have a history of seemingly minor or low-grade ‘soreness’ on the affected limb or other concerns of an ‘ankle problem’, for several days or weeks prior to overt acute fracture (see discussion of pathophysiology below). Diagnostic analgesia is rarely needed to localize the site of pain in horses with condylar fractures and is contraindicated in all horses with clinical signs typical of acute fracture given the risks for exacerbation of the injury (i.e. development of a complete or even catastrophic fracture). In the exceptional case of a horse with a chronic, incomplete or unicortical lateral condylar fracture46 (a horse that has been able to continue some level of exercise or does not have a history of acute onset of marked lameness and joint effusion), a full lameness examination with diagnostic analgesia would be acceptable. In these horses a low palmar/plantar nerve block or intra-articular local anesthetic block of the fetlock joint will result in improvement of the lameness. Four standard radiographic projections (lateral, dorsopalmar/plantar, DLPMO, DMPLO) of the involved fetlock are indicated for all cases of lateral condylar fracture. Ideally, these should include the full length of the metacarpus/metatarsus because on rare occasions fracture lines will extend proximally into the diaphysis. Radiographs of the full metacarpus/metatarsus are mandatory for all cases of medial condylar fracture given the propensity for these fractures to extend into the proximal diaphysis, and the concerns of mid-diaphyseal comminution and the associated potential for catastrophic fracture.47 A flexed dorsopalmar/plantar projection48,49 is also recommended to evaluate the palmar/plantar aspect of the condyles for the presence of a comminuted fragment at the articular surface (Fig. 16.7). Similarly, the proximal sesamoid bones should be scrutinized for the presence of any associated fractures – in particular, axial fractures of the lateral proximal sesamoid, which are most commonly associated with displaced lateral condylar fractures44,50 (Fig. 16.8). It is important to note the presence of any additional pathology such as dorsal Pl chip fractures (flexed lateral radiographs are beneficial here), so that these can be addressed at the time of surgery, or signs of degenerative joint disease so that their potential impact on the horse’s prognosis can be appropriately considered. The advantages of CT and MRI over conventional radiography for diagnosis of musculoskeletal injuries have been clearly demonstrated in people and horses. Nonetheless, advanced imaging techniques are rarely necessary to make an initial diagnosis in the vast majority of condylar fractures. However, in the specific case of condylar fracture, the superiority of CT over radiography for identifying proximal fissures, articular comminution, proximal sesamoid fractures and other subtle pathology have been documented.51 As such, these modalities, in clinics where available, are sometimes used to assess fracture configuration in the more complex cases – in particular medial condylar fractures – prior to surgical repair. Horses with short medial condylar fractures should at least be managed with a rigid heavily padded bandage (such as a Robert-Jones bandage), with the addition of splints a prudent option. In horses with radiographically identifiable fracture lines in the mid-diaphysis, dorsally and laterally applied splints in the forelimb (extending to the elbow) or plantar and lateral splints in the hind limb extending to the point of the hock are recommended. Rigid coaptation with a bandage and splints or application of a well-constructed full-limb cast should also be considered prior to transportation given the propensity for catastrophic failure.44,47 In certain cases of short, incomplete condylar fractures, particularly those in which economic considerations preclude surgery, non-surgical treatment can result in a good outcome.41,44,52 The distal limb is kept in a bandage for 2–3 weeks to help minimize any soft tissue swelling and to provide some support. NSAIDs are administered only as needed to provide analgesia. Generally, the majority of horses in this category are quite comfortable within a few days to a week or so following the injury. Horses initially should have 1–2 months of strict stall rest, followed by another 1–2 months of stall confinement with daily hand-walking exercise. Follow-up radiographs are repeated three months from the time of fracture and if healing is progressing well, exercise in the form of small paddock turnout can begin. Under ideal circumstances, fractures heal in approximately four months. The major disadvantage of non-surgical treatment is the tendency for fractures to exhibit delayed healing at the articular surface.41,52,53 Resumption of training should not commence until fractures have completely healed and this may take up to six months or longer in some horses treated non-surgically. However, in a small percentage of horses a gap or defect in the subchondral bone may persist indefinitely well beyond the point at which the fracture has healed, which can complicate the decision on when to resume training.
Metacarpus/metatarsus
Dorsal metacarpal disease (the ‘bucked shins’ complex)
Recognition
Physical examination
Lameness examination
Diagnostic confirmation
Radiography
Therapy
Anti-inflammatory therapy
Modified training protocol
Prognosis
Epidemiology
Prevention
Dorsal cortical stress fractures of MC-III (‘saucer fractures’, metacarpal fatigue fractures)
Recognition
History and presenting complaint
Physical examination
Lameness examination
Diagnostic confirmation
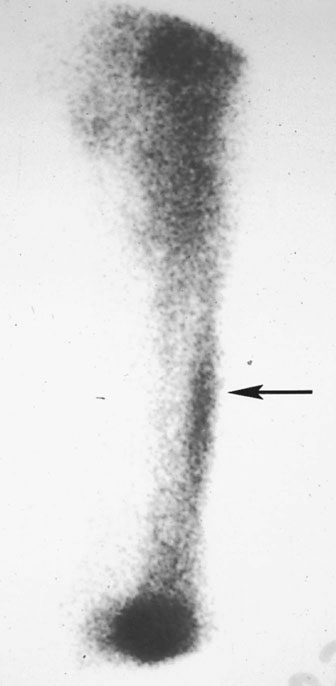
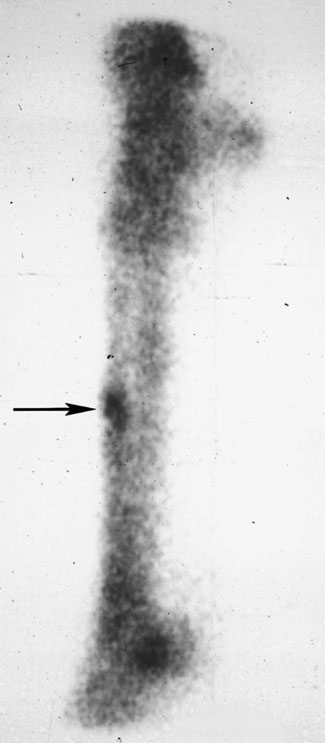
Scintigraphy
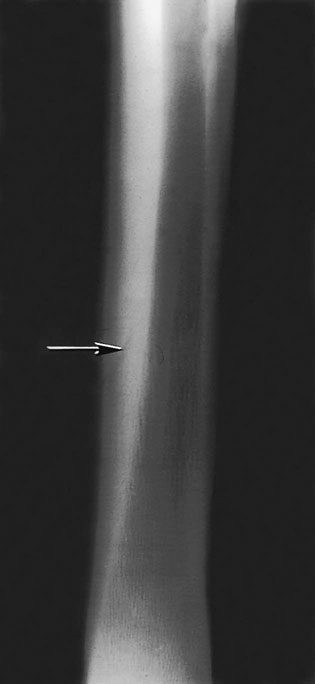
Radiography
Treatment and prognosis
Non-surgical management
Osteostixis
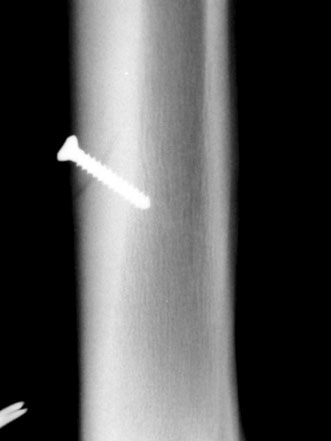
Screw fixation
Prognosis
Etiology and pathophysiology
Epidemiology
Condylar fractures (parasagittal or longitudinal fractures of the distal third metacarpus and metatarsus)
Recognition
History and presenting complaint
Diagnostic confirmation
Diagnostic analgesia
Radiography

Computed Tomography and Magnetic Resonance Imaging
Therapy
Emergency treatment
Non-surgical management
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Metacarpus/metatarsus