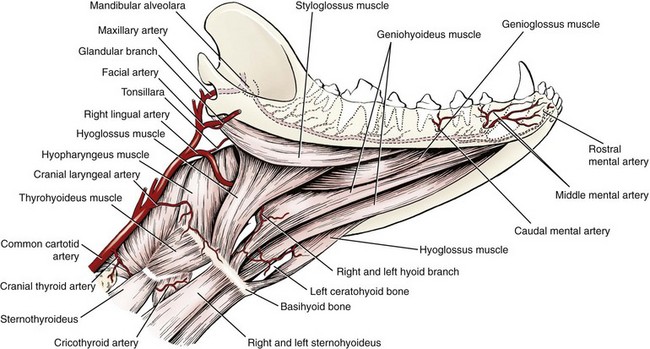
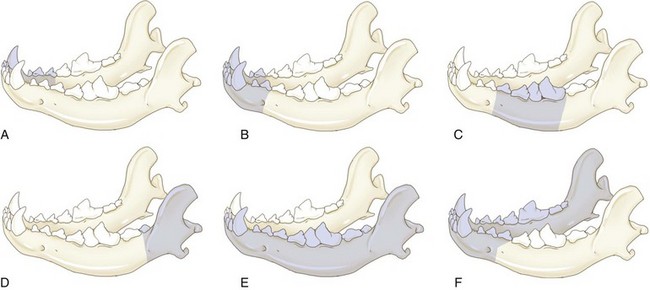
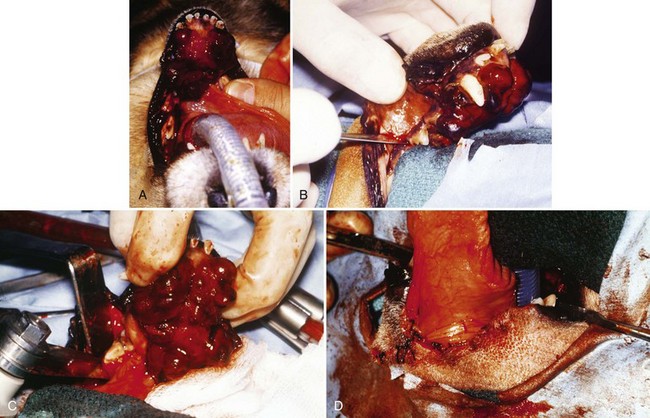
Chapter 89 In both dogs and cats, the mandible consists of right and left halves, each of which are divided into the body, which is the horizontal component containing the teeth, and the ramus, which is the vertical component that articulates with the skull at the temporomandibular joint and does not contain teeth. The body and ramus converge at the angle of the mandible.10 The two bodies are joined rostrally at the symphysis, which is a strong, fibrous joint. The major muscles of mastication are the masseter, which extends from the zygomatic arch to the lateral surfaces of the caudal body and ventral ramus; the temporalis, which extends from the temporal region of the skull to the dorsal portion of the ramus; the pterygoideus, which extends from the pterygoid, palatine, and sphenoid bones to the angular process of the ramus; and the digastricus, which extends from the occipital region of the skull to the ventral border of the body of the mandible. The majority of blood supply to the mandible is provided by the mandibular alveolar artery, a branch of the maxillary artery (Figure 89-1). The mandibular alveolar artery enters the mandible through the mandibular foramen, which is located on the medial surface of the bone near the angle of the mandible. The artery courses rostrally within the marrow cavity of the mandible, eventually exiting laterally through the mental foramen immediately caudal to the canine tooth. The mandibular alveolar artery almost invariably must be ligated or cauterized and transected during mandibulectomy. The mandibular nerve provides sensory innervation to the mandible and lower teeth. A branch of the trigeminal nerve, it enters the mandibular canal via the mandibular foramen; courses through the canal as the mandibular alveolar nerve; and exits laterally through the mental foramina as the mental nerves, which innervate the lower incisors and surrounding tissues. The mandibular and sublingual salivary ducts course medial to the body of the mandible beneath the gingiva and open at the sublingual papilla just caudal to the symphysis. These ducts are occasionally identified during mandibulectomy and may be ligated if they are visualized; however, transection of the ducts without ligation does not lead to complications.10 Each side of the muzzle of dogs and cats is composed of three bones: the maxilla, the largest bone of the face, which contains the canine, premolar, and molar teeth; the incisive bone or premaxilla, which contains the incisor teeth; and the nasal bone, a long, slender bone on the dorsal midline of the muzzle. The nasal cavity contains the highly vascular nasal turbinates and is usually entered during maxillectomy. Blood supply to the maxillary region is provided by two major arteries, both branches of the maxillary artery (see Figure 99-6). The major palatine artery courses through the caudal nasal cavity, passes through the caudal portion of the hard palate via the caudal palatine foramen, and then courses rostrally ventral to the hard palate midway between the midline and the maxillary teeth. Ligation or cauterization of the artery during maxillectomy does not have adverse effects. The infraorbital artery courses through the caudal nasal cavity dorsal to the major palatine artery and passes through the maxillary foramen and infraorbital canal of the maxilla, exiting laterally through the infraorbital foramen at the level of the rostral margin of the carnassial tooth. The infraorbital nerve, a branch of the maxillary nerve supplying the teeth, also courses through the infraorbital canal. Resection of tumors that approach or involve the infraorbital canal requires ligation or cauterization of the infraorbital artery and transection of the infraorbital nerve. Both structures can be transected without adverse consequences. The parotid salivary gland overlies the ventral portion of the vertical ear canal, and its duct terminates at a small papilla just lateral to the fourth upper premolar tooth. The zygomatic salivary gland lies medial to the rostral portion of the zygomatic arch and is drained by several ducts that terminate just caudal to the papilla of the parotid duct. Whether visualized or not, the ducts can be transected during maxillectomy without adverse consequences. Tumor Types and Biologic Behavior The most common oral tumors of dogs, in descending order of frequency, are malignant melanoma, squamous cell carcinoma, fibrosarcoma, osteosarcoma, and acanthomatous ameloblastoma. (In this chapter, the term squamous cell carcinoma refers to nontonsillar squamous cell carcinoma; squamous cell carcinoma of the tonsils has a significantly higher metastatic rate than the nontonsillar form and cannot be managed effectively with surgery alone.) Each of these tumors has significant potential to invade surrounding tissues, including bone; however, they vary significantly in their metastatic potential. In a large necropsy study reported in 1979, 81% of malignant melanomas, 82% of squamous cell carcinomas, and 35% of fibrosarcomas had metastasized to or beyond regional lymph nodes.39 The sample of squamous cell carcinomas in this study was small, and subsequent studies have indicated that this tumor has a metastatic rate of approximately 20%.38 Similar to appendicular osteosarcoma, oral osteosarcoma frequently metastasizes to the lungs, although survival times after surgical excision appear to be superior to survival times observed after amputation for appendicular osteosarcoma.17,36 Fibromatous epulides of the periodontal ligament and ossifying epulides are slow-growing, firm lesions that may be pedunculated or broad based and that often occur in the premaxillary region (Figure 89-2). Local excision without bone removal usually provides excellent long-term control. The likelihood of cure can be increased by extracting the involved tooth and removing a small margin of surrounding alveolar bone with an air drill. Acanthomatous ameloblastoma is a nonmetastatic but locally invasive tumor that frequently invades the underlying bone and should be treated by mandibulectomy or maxillectomy.3,42 This tumor typically occurs in the rostral portion of the mouth. Other, infrequently observed malignant tumors that may occur in or near the oral cavity include peripheral nerve sheath tumors arising from the infraorbital nerve; multilobular osteochondrosarcoma;35 and histologically low-grade, biologically high-grade fibrosarcoma.7 The latter tumor is a variant of fibrosarcoma that appears histologically benign but that aggressively invades bone and requires wide excision.7 Although a definitive diagnosis of oral tumors requires histopathology, a reasonably accurate guess regarding tumor type often can be based on signalment of the patient and location and gross appearance of the lesion. Malignant melanoma, squamous cell carcinoma, and fibrosarcoma usually arise from the gingiva. Malignant melanoma tends to affect older small-breed dogs, including Cocker spaniels and miniature poodles, but may occasionally affect larger-breed dogs such as Chow Chows and golden retrievers.39 The tumor is often darkly pigmented but may be amelanotic (Figure 89-3). Squamous cell carcinoma tends to affect older large-breed dogs39 and often has a flat, ulcerative appearance with minimal production of an external mass (Figure 89-4). Fibrosarcoma, including the histologically low-grade, biologically high-grade variant, usually affects middle-aged and older large-breed dogs, particularly golden and Labrador retrievers.39 The tumor usually is proliferative, often arises in the gingiva near the maxillary carnassial tooth, and may extensively involve the hard palate (Figure 89-5). Osteosarcoma usually affects medium- and large-breed dogs and may arise in the maxilla or mandible. Acanthomatous ameloblastoma usually affects medium- and large-breed dogs and often occurs in the rostral mandible or maxilla. The tumor has a similar gross appearance to squamous cell carcinoma and often causes spreading of adjacent teeth (Figure 89-6). Figure 89-5 Fibrosarcoma. The tumor often arises near the carnassial tooth and is typically proliferative in appearance. Oral radiographs obtained during general anesthesia may be useful as an aid in determining the extent of the tumor. Between 60% and 80% of tumors arising in or near the gingiva cause radiographically apparent bone lysis.17,39 However, because bone must lose a significant proportion of its mineral before it acquires a lytic radiographic appearance, plain radiographs tend to underestimate the extent of bone destruction and are an unreliable tool for surgical planning. In addition, plain radiography gives a poor representation of the degree of involvement of normal soft tissues. Computed tomography (CT) and magnetic resonance imaging (MRI) are superior modalities for assessing bony and soft tissue margins but are not yet widely available to veterinarians. These modalities are particularly valuable for evaluating lesions whose size or location may make complete resection difficult. These include caudal maxillary or mandibular lesions; lesions that approach or extend beyond the midline; and lesions that may encroach upon the nasal cavity, pharynx, or orbit. Small tumors located in the rostral oral cavity often can be assessed adequately through a combination of physical and radiographic examination. Thorough preoperative staging of oral malignancies should include an assessment of regional lymph nodes for metastases. The canine oral cavity drains to the mandibular, parotid, and medial retropharyngeal lymph nodes; however, of these, only the mandibular node is normally palpable. Lymph node size as determined by palpation is an unreliable indicator of metastases: in a series of 100 dogs with oral malignant melanoma, the sensitivity and specificity of lymph node size for predicting cytologic or histologic presence of metastases were only 70% and 51%, respectively.44 Cytologic examination of material obtained by fine needle aspiration of the mandibular lymph node is likely to provide an accurate assessment of that node;14,18 however, the parotid and medial retropharyngeal nodes are not readily accessible to aspiration. A simple surgical approach that allows excision of all three nodes through a single incision has been described34 and is the optimal strategy for lymph node staging for dogs with suspected oral malignancies. In a series of 28 dogs and three cats undergoing this procedure, 35.5% had histologic evidence of metastases to one or more of the three lymph nodes; however, of these, only 54.5% had metastases to the mandibular node, demonstrating the inadequacy of staging protocols that assess the mandibular node alone.34 This staging procedure can be performed during the anesthetic episode used for biopsy and imaging of the primary tumor. Complete resection of most oral tumors, with the exception of those confined to the lip margins or tongue, requires partial mandibulectomy or partial maxillectomy. Many clients have a natural aversion to considering these procedures and require a thorough description of the cosmetic and functional results of surgery before making a decision. Owners may benefit from viewing images of dogs or cats that have undergone the procedures and from conversations with other owners whose animals have been treated for oral cancer. In a retrospective survey of 27 owners of dogs that had undergone mandibulectomy or maxillectomy at a mean of 44 months previously, 85% of owners of owners stated that they were satisfied with their decision to have surgery performed.11 A brief discussion of cosmetic and functional considerations follows descriptions of surgical procedures below. Local nerve blocks using 0.5 to 1.0 mL of 0.5% bupivacaine can be very useful for preventing pain in patients undergoing mandibulectomy or maxillectomy. Techniques for local blocks have been well described.21,33 For rostral mandibulectomy, the incisor region can be blocked by injecting just rostral to the mental foramen at the level of the second premolar tooth. For more extensive mandibulectomies, the entire body and surrounding tissues can be blocked by injecting the mandibular nerve near the mandibular foramen, which is often palpable on the medial side of the bone near the angle of the mandible. The rostral maxillary area can be blocked by injecting the infraorbital nerve as it exits the infraorbital foramen dorsal to the rostral aspect of the fourth upper premolar tooth. The entire maxillary region can be blocked by injecting the maxillary nerve; the needle is introduced rostral to the ramus and below the ventral border of the zygomatic arch just caudal to the lateral canthus of the eye. Because of the extensive vascular supply of the oral and nasal cavities, control of intraoperative hemorrhage is an important technical aspect of mandibulectomy and maxillectomy. The mandibular alveolar artery must be identified and ligated or cauterized during mandibulectomy. The major palatine artery or infraorbital artery may need to be transected during partial maxillectomy and must be ligated. The nasal cavity is usually entered during maxillectomy, and control of diffuse hemorrhage from transected nasal turbinates can be challenging. Temporary13 or permanent occlusion of the carotid arteries before tumor removal may be used to reduce intranasal hemorrhage and is most useful during caudal maxillectomy. In most other cases, hemorrhage within the nasal cavity can be controlled with a combination of electrocautery, absorbable gelatin sponges, and topical administration of epinephrine, as described below. For purposes of the descriptions below, rostral mandibulectomy refers to excision of bone surrounding some or all of the lower incisors and, if necessary, one or more canine teeth; central mandibulectomy refers to removal of a segment of one mandibular body; caudal mandibulectomy refers to removal of all or a portion of one ramus; and hemimandibulectomy refers to removal of the entirety of one half of the mandible (Figure 89-7). These are overlapping designations with no strict definitions, and the procedures are commonly combined as necessary. The majority of mandibular tumors are confined to a body of the mandible and do not require transection or removal of the ramus. Rostral and Central Mandibulectomy (Figure 89-8).: After the sites for transection of bone have been selected, the gingiva is sharply transected to the level of the bone. The gingival margins should be located approximately 0.5 cm beyond the level of the planned bone transection. The gingiva is undermined with a periosteal elevator, preserving a cuff of gingiva to be used in closure. After gingival transection, the oral mucosa, labial mucosa, muscular attachments, and skin are transected and dissected away from the mandibular body and tumor as necessary to achieve adequate resection margins. In most dogs, there is redundant skin and mucosa adjacent to the mandible, and wide soft tissue margins can be taken without compromising prospects for wound closure. Some diffuse hemorrhage should be expected during dissection of the soft tissues, and use of electrocautery in cutting mode can dramatically limit this bleeding.
Mandibulectomy and Maxillectomy
Anatomy
Maxilla
Canine Oral Tumors

Preoperative Staging
Surgery
Preoperative Patient Preparation
Technique for Mandibulectomy
< div class='tao-gold-member'>
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Mandibulectomy and Maxillectomy
Only gold members can continue reading. Log In or Register to continue