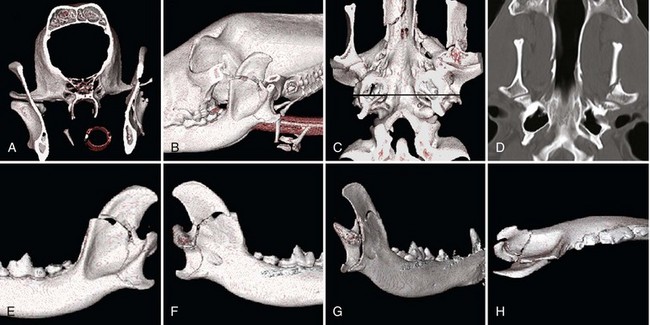
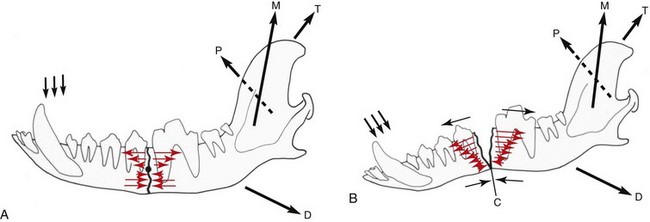
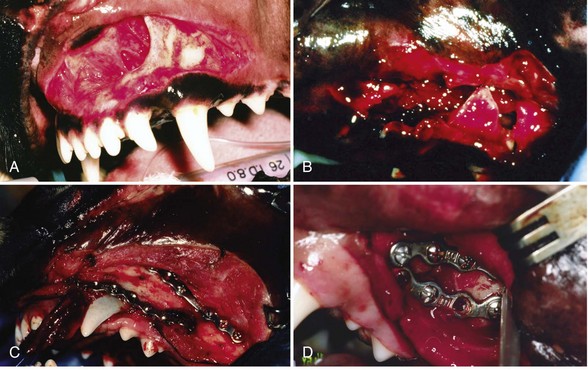
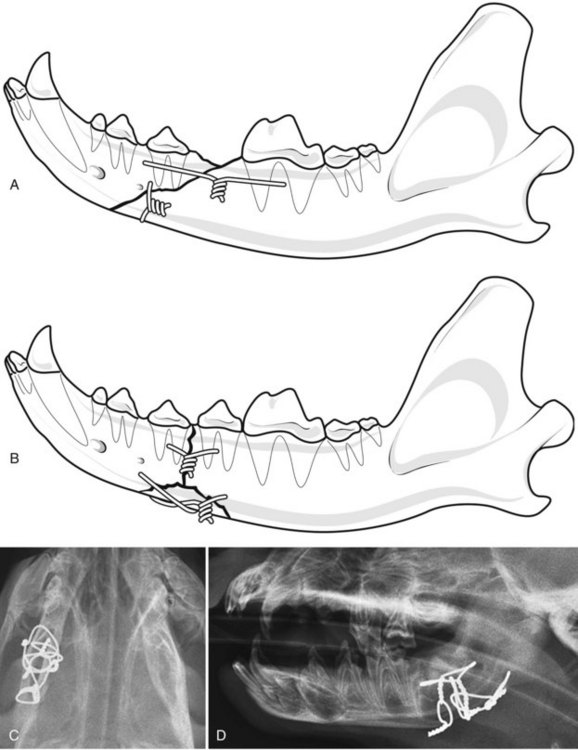
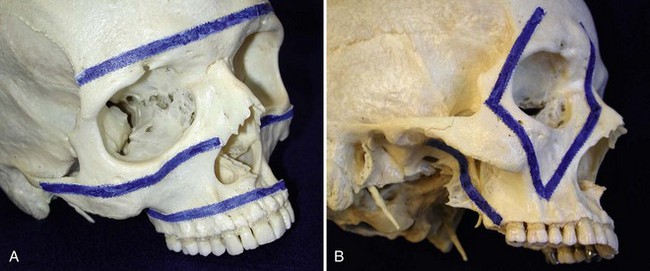
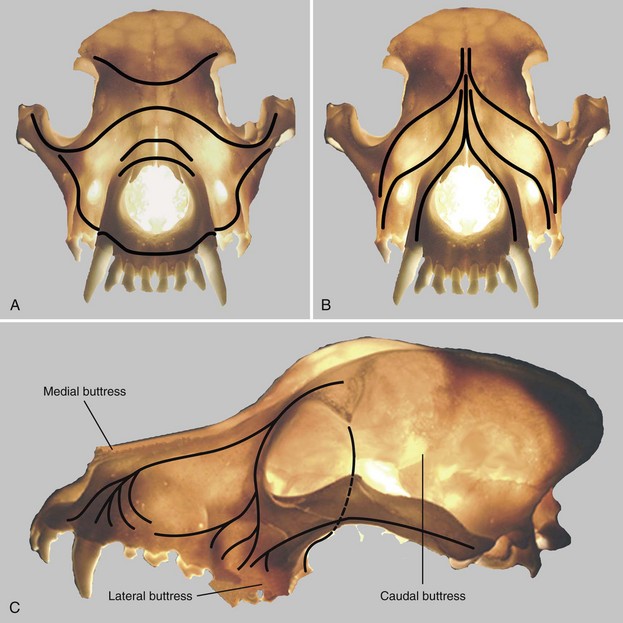
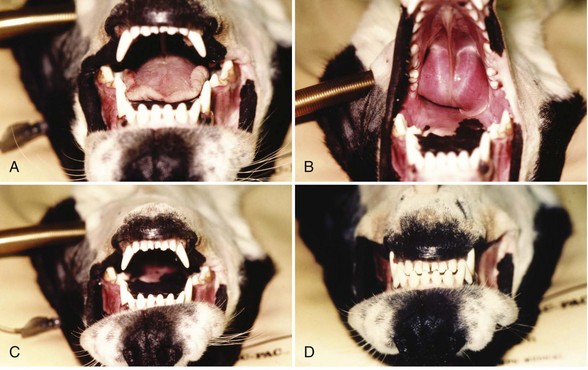
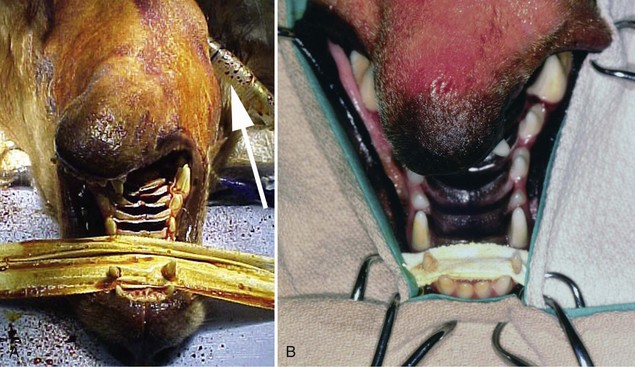
Chapter 67 Radiographic examination is necessary to assess the fracture and to evaluate the teeth (see Chapter 66). Standard radiographic views include ventrodorsal and lateral projections and both right and left lateral oblique views. Oral radiography using dental film or digital imaging is preferred to conventional skull radiography but is limited to areas of the dental arch. Standard radiography is difficult to interpret because of the many overlying structures of the skull and the bilateral nature of the regional anatomy. Fractures involving the ramus or condylar process of the mandible and the midfacial skeleton are best visualized using computed tomography (Figure 67-1). Nasal fractures may be difficult to diagnose, as these bone fragments usually are stable (Figure 67-2).18 Fractures that involve the nasal turbinates may interfere with breathing. Longitudinal fractures along the center of the nose often are stable and seem to be more frequent in cats than in dogs. Swelling, pain on palpation, and nasal bleeding may be clues that nasal and maxillary fractures are present. Maxillary fractures may result in upward or lateral deviation of the nose. Recognition of mild nasal malalignment can be difficult when coexisting fractures of the mandible are present. Similarly, fractures of or near the orbit may involve supporting structures of the eye. Owing to the absence of circumferential bone, these injuries require special attention to reconstruct the supporting soft tissue structures. Canine and feline mandibles differ from the long bones in that they do not have a medullary canal. The mandibular cortex surrounds the cancellous bone and the mandibular canal, which contains the inferior alveolar neurovascular structures, but no hematopoietic cells.92,110 The material properties and structure of the mandible and maxillofacial skeleton are determined by the very different mechanical forces to which they are subjected. The maxillofacial skeleton differs from the mandible in that it consists of a thin lamina of bone, which provides an increased surface area of bone compared with the volume it occupies; consequently, vascularity to these bones is relatively greater. The result is a much faster healing rate in these areas compared with the mandible, which heals similarly to many long bone fractures. As in other areas, fracture healing can occur by indirect or direct bone healing.17,52,95,96 Indirect bone healing results from some mechanical instability of the fracture and leads to callus formation. Direct bone healing occurs under conditions of close apposition of the bone fragments, which also provides improved mechanical stability. Direct bone contact allows healing by cutting cone/Haversian canal remodeling without callus formation; however, interfragmentary compression is not an absolute requirement, as has been demonstrated both experimentally35,38,55 and clinically.25,56 Direct bone healing will occur with reapposition of the fracture ends as contact or gap healing.94,95 Direct bone healing will occur only with anatomic reduction and absolutely rigid fixation, which are the goals of maxillofacial fracture repair. The result is quicker function with no adverse consequences associated with a large callus. Increased frequency of complications with fracture healing has been observed when teeth are removed owing to their involvement with fractures of the dental alveoli.53 Previously, it was recommended to extract the teeth located within a fracture line.67,91 The rationale suggested was that as a consequence of the fracture, tooth blood supply was disrupted and pulpal tissue underwent an inflammatory response that subsequently resulted in a periapical abscess, which in turn delayed or prevented fracture healing. However, despite this possibility, it is not often observed. Furthermore, removal of teeth may increase complications through disruption of the blood supply and iatrogenic trauma to adjacent tissues, including further displacement of the fractured bone fragments, elimination of occlusal landmarks useful in realigning bone segments to allow functional occlusion, elimination of available structures for use in the fixation of bone fragments, and creation of a large bony defect, adding to the difficulty of the reduction and stabilization. These latter factors are much more significant and common issues, resulting in complications of prolonged healing and infection. Several studies in human beings have long established that teeth remaining in a fracture line do not increase the complication rate or morbidity associated with mandibular fracture.57,72 Preservation of teeth involved within a fracture line in mandibular fracture has been reported to be associated with a favorable prognosis if optimal reduction and stabilization of the jaw have been achieved.1,43 Therefore, removal of teeth is not advised unless involved teeth are fractured or loose and cannot be stabilized.1 A general sequence of treatment is recommended, including an “inside-to-outside” approach whereby the bone is treated first, followed by the teeth (as related to the underlying bone), then the soft tissues; treatment for the specific dental injury (i.e., restoration) is the last priority.1 It is preferable to allow long-term observation to assess the final outcome of possible pulp damage in situations in which the vitality if a tooth is in question; compromises in this area often are necessary and appropriate for the overall benefit of the patient.1 Current recommendations by human oral surgeons are to preserve teeth whenever possible in the presence of a fracture.1,41,43 Preservation of teeth in small animals is similarly recommended, especially given the much greater relative area of bone that the teeth occupy in small animals and their greater importance in maintaining bony continuity/stability.86 Fracture of the alveolar bone or fracture of a tooth root results in a loose tooth. If only the alveolar bone is fractured and the tooth structure is intact, the preferred treatment is to leave the tooth in place and stabilize the fracture.34,86 Teeth that are avulsed may be reimplanted provided the alveolus remains intact41,91,104 or can be reestablished with stable fixation (see Chapter 66 for guidelines on reimplantation).34,41,109 Root canal therapy is required in these cases once the tooth is stable but need not be performed at the time of the initial fracture repair, although this is preferred.21,24,41,86,109 If the fracture involves the tooth, treatment approaches vary. Teeth that are not salvageable and are not essential to the stability of the fracture repair should be removed. These extractions most commonly involve the incisors or smaller premolars. Fractured teeth with small mobile coronal fragments are preserved; these fragments are removed and restoration of the defect performed if the pulp cavity is not invaded. In the case of a fractured tooth with exposure of the pulp cavity, an endodontic procedure such as vital pulp therapy or root canal therapy should be performed.86 The indications for these techniques vary with the severity of damage to the pulp.44,109 Vital pulp therapy (partial pulpectomy, direct pulp capping, and restoration of the fracture site) is a procedure designed to treat and preserve vital pulp and should be performed at the time of the initial fracture repair. If the vitality of the tooth in the fracture area is uncertain, the fracture is treated and the tooth is reevaluated both during and after fracture healing. If the tooth loses vitality, root canal therapy is performed. If a periapical abscess develops, extraction should be performed, but this usually is delayed until fracture healing has occurred. Open fractures, which are open to the oral cavity, occur in a majority of mandible/maxillofacial fractures. Inevitably, these fractures are contaminated28,105,106; as such, antibiotic administration is recommended. The initial empirical choice (a broad-spectrum antibiotic, e.g., a first-generation cephalosporin) is followed based on bacterial culture and sensitivity testing. Despite universal agreement regarding perioperative usage, continued postoperative use has been questioned.19,64,89,90 Despite the open nature of these original wounds, infection generally is not a problem owing to the excellent vascular supply of the head. Obtaining rigid stability with the appropriate fixation technique decreases the likelihood of postoperative infection. Conversely, bone fragment motion and subsequent implant loosening interfere with revascularization and healing and predispose the area to infection. Understanding the biomechanics of the mandibular and maxillofacial skeleton is critical to fracture repair, as it dictates optimal implant placement. In the mandible, all muscular insertions are located on the caudal part of the mandible, at the level of the ramus; this eliminates all mechanical support of the mandibular body following fracture. The rostral fragment thus displaces in a caudoventral direction.13 Alternatively, the maxilla is broadly attached to the skull and supports the dental arcade with areas of thickened bone (described as areas of buttress support) that disperse the applied forces over a wide area.14 Bending forces are the primary forces acting on the mandible.30,61,101,102 The mandible acts as a long lever arm and resists bending forces with a strong compact layer of bone that lies parallel to the teeth.32 A continuum of tensile-to-compressive stresses exists from one side of the bone to the other during bending stress.30,73,102 Maximal tensile stresses exist at the oral, or alveolar, surface, and maximal compressive stresses exist at the aboral surface.30,61 At the ramus, shear forces are maximal, whereas rostrally, at the symphysis, rotational forces are maximal.30,101 Distraction of the oral margin occurs after a mandibular fracture and is accentuated upon contraction of the masticatory muscles (Figure 67-3). The anatomic configuration of a long lever arm with absence of any further supplemental support is unique to the mandible and must be considered with any fixation method.32 Application of any implants therefore must consider both the tension and compression surfaces of the bone.32,61 Because all fixation devices are strongest in tension, whereby all stresses act parallel to the longitudinal axis of the implant, they are ideally placed on the tension surface of the bone. In cases of mandibular fracture, this is along the alveolar border of the bone, where the basic biomechanical principle is tension band fixation.26,30,61,76,102 Depending on the implant to be used, this location may or may not be appropriate owing to possible interference with the large tooth roots and adjacent neurovascular structures. The maxillofacial skeleton must support and balance the identical forces applied by the mandible. The distribution of these forces, however, is very different from the mandible, as this area is subject to much less strain. The latter has the construction of an “outer facial frame” in human beings, which acts as a link between the base of the skull and the occlusal surfaces.32 Support of the facial region is provided by a series of anatomic buttresses that distribute the masticatory forces to the head. These buttresses exist in the horizontal, vertical, and coronal planes.20,32,42,85 Three primary buttresses are present: rostral (medial), lateral, and caudal (Figure 67-4). These buttresses can be defined anatomically as rostral (medial) nasomaxillary buttress, lateral zygomaticomaxillary buttress, and caudal pterygomaxillary buttress. The anatomic definitions mirror the bones of the skull that constitute these buttresses. The caudal buttress is composed of the lacrimal, palatine, and pterygoid bones and is not readily accessible. The facial frame can be reconstructed utilizing just two of the three buttresses; thus, all attention is directed toward the medial and lateral buttresses. The caudal buttress is reduced indirectly as a result of primary stabilization of the other fractures of the maxillofacial skeleton and the skull. The incisive bones are not part of the buttresses in the dog and cat and therefore may not need to be stabilized, as this area generally does not provide essential support to the skull; the nasal bones also may be fractured without disturbing the medial buttress. Fixation of the incisive or nasal bones still may be performed to provide support for the incisors or to reestablish the cosmetic appearance of the nasal area.10 Similarly, maxillary fractures may not require stabilization unless the buttresses are compromised.15 If the medial buttresses are compromised, malocclusion is likely, and loss of orbital support may occur. Similarly, if the lateral buttresses are compromised, the orbit is likely to be affected. Because of the anatomic configuration (a thin lamina that is reinforced by thicker areas of support) of the maxillofacial bone, plate fixation is ideally suited to reestablish the three-dimensional integrity; however, very small (mini) implants are necessary owing to the limited available space.10,15 Figure 67-4 Horizontal (A) and vertical (B) buttresses of the maxillofacial region of the human skull. (Reproduced with permission from Moe KS, Byrne P, Kim DW, et al: Facial trauma, maxillary and Le Fort fractures, 2009, http://emedicine.medscape.com/article/283568-overview#a04. Accessed July 18, 2011.) The facial support provided by these buttresses reveals the design of a “truss” or “frame,” which is a triangle; in three dimensions, the basic truss is a tetrahedron, a three-sided pyramid that can resist distortion in any direction three-dimensionally.32 In human beings, the vertical buttresses of the midface are the clinically most important with regard to the management of midface fractures to maintain the vertical dimension, or midface height.32,85 These buttresses are strong in resisting vertically directed stresses; however, they cannot withstand forces of similar magnitudes in the transverse plane. Although no similarly detailed description of maxillary buttresses in the dog or cat has been put forth, a similar anatomic arrangement to the human skull has been suggested (Figure 67-5).14,15 These trusses can be similarly visualized in the skull as pillars of reinforced bone. In the dog, and presumably in the cat, the medial and caudal buttresses provide similar vertical support as in human beings, although because of the configuration of the skull, these buttresses are better designed to withstand transverse forces as compared with those in human beings.14 The lateral buttress appears to function primarily to withstand forces in the vertical plane; however, it also supports the other two buttresses, so as to better withstand increased shearing forces in the premolar/molar region in these species.14 The lateral buttress in the dog and cat thus may be the most clinically important, as it appears to more effectively neutralize forces in the transverse plane, despite lacking secondary lateral support adjacent to the orbit.14,82 The latter is supported by the orbital ligament in the dog and cat,82 whereas this is bony support in human beings and is part of the lateral buttress.32 The attachment of the maxillofacial skeleton to the base of the skull appears to have greater bony support in dogs and cats than in human beings. Figure 67-5 Cranial (A–B) and lateral (C) views of the canine skull, which is transilluminated to reveal the buttressing. The lines drawn indicate the horizontal (A) and vertical (B) buttresses of the maxillofacial region of the canine skull (compare with Figure 67-4). The three maxillofacial buttresses can be described as a combination of these horizontal and vertical buttresses (C). The nasomaxillary (medial) buttress is seen rostrally, the zygomaticomaxillary (lateral) buttress is seen caudally, and the pterygomaxillary (caudal) buttress is shown with the dashed line. (Modified from Boudrieau RJ: Fractures of the maxilla. In Johnson AL, Houlton JEF, Vannini R, editors: AO principles of fracture management in the dog and cat, Stuttgart, 2005, Georg Thieme Verlag.) In the dog and cat, the tooth roots occupy a considerable volume of the mandible and maxilla; the teeth occupy almost one half of the mandibular body volume. Because of the presence of the teeth, it is difficult to provide conditions of rigid bone stabilization along the alveolar margin, which is the biomechanically preferred location for placement of implants (implants under tension) for most effective neutralization of the bending forces. Several fixation methods, therefore, utilize the teeth to secure a variety of intraoral devices (see Chapter 66). In human beings, implants applied to the bone are placed inferior to the tooth roots and inferior to the level of the mandibular canal. This position retains the biomechanical advantage of a tension band because of the overall large dorsoventral mandibular height.20,74 Despite the biomechanical advantage of implant placement on the tension band side of the bone, a second implant is placed parallel and a few millimeters away for added stability; the second implant provides additional shear and rotational stability. Despite the anatomic constraints of a more limited dorsoventral mandibular height and a larger tooth volume in the dog and cat, implants still may be placed along the alveolar bone margin. At this level, however, implant purchase in the bone must occur between the tooth roots using small implants. The latter requirement was the rationale for use of intraosseous wiring fixation techniques; more recently, miniature plating systems have become more popular and offer the additional benefit of providing greater three-dimensional stability. Application of implants along the alveolar bone margin must avoid penetration of the tooth roots, as tooth invasion will lead to tooth death.53 Despite these recommendations, it is likely that both major (>50% of screw diameter penetrating the tooth root) and minor (<50% of screw diameter penetrating the tooth root) contacts with a tooth occur. It is unknown whether significant clinical problems manifest in the dog and cat should this occur; however, studies in human beings have shown minimal morbidity in a large series of clinical patients.8,40 Regardless, care must be undertaken so as to minimize tooth impingement. As previously noted, the teeth play an important role in maintaining fracture stability because of their large size and the bony area that they occupy. Bone healing, especially direct bone healing, relies on absolute stability; therefore, preservation of the teeth is important, as their removal may adversely affect bone healing. Surgical dissection to excise apical fragments may lead to additional disruption of the blood supply and further fragment displacement, may eliminate available structures for possible fracture fixation, may eliminate occlusal landmarks used to realign bone segments, and may create large bony defects that prevent adequate fracture stabilization. To enhance the environment for bone healing (and maximize the stability of the fracture repair), teeth that are present within a fracture line generally are not removed unless they cannot be stabilized or do not contribute to the stability of the fixation.53 Implant placement while avoiding the mandibular alveolar canal is recommended; however, because of the short dorsoventral mandibular height and the large size of the tooth roots, this is not realistically possible. Minimal patient morbidity has been demonstrated despite attempts to investigate this potential problem.59 Despite disruption of the inferior alveolar artery within the mandibular canal, the teeth have been shown to remain unaffected, with no evidence of pulpal necrosis or diseased teeth.59 This is likely due to rapid reconstitution of the vascular supply from the transient extraosseous circulation of surrounding soft tissues that becomes established shortly after fracture.92,110 Perioperative and postoperative antibiotic therapy is recommended in the dog106 and cat,105 much as in human beings,112 because open fractures occur in a majority of these cases.93 Antibiotics generally are continued in the postoperative period; the choice of subsequent antibiotic therapy is determined by the results of bacterial cultures obtained intraoperatively and subsequent susceptibility testing.93 Patient positioning for unimpeded surgical access is performed such that the head is situated at the end of the surgical table, thus allowing easy access rostrally and laterally (the latter bilaterally) (Figure 67-6). This requires that all anesthetic equipment to be positioned away from the head, usually at the tail end of the patient. Therefore, anesthetic monitoring cannot utilize eye position and reflexes or jaw tone and must be performed by assessing other parameters such as heart rate and rhythm, respiratory rate and depth, pulse character, and blood pressure. Figure 67-6 For mandibular fracture repair, the dog is positioned in dorsal recumbency with both forelegs pulled caudally (the forelimbs also are crossed, which helps to stabilize the positioning). A wire-reinforced tracheal tube has been placed through a pharyngotomy incision on the left side of the neck. A, Rostral view of the occlusion. B, The tip of the tongue has been reflected caudally into the pharynx. C–D, Repositioning the tongue in this manner allows the tongue to be reflected out of the way so it does not interfere with assessment of occlusion intraoperatively. The maxilla also must be secured to the table to provide a stable base for any assessment/manipulation (see Figure 67-7). The head must be securely fastened to the surgical table to provide the requisite surgical stability during surgical manipulation. The maxilla (dorsal recumbency) or mandible (ventral recumbency) is taped to the table with waterproof tape that traverses across the upper or lower canine teeth, respectively (Figure 67-7). The tongue must be reflected caudally into the pharynx to allow complete closing of the mouth and to permit unobstructed intraoperative assessment of occlusion (see Figures 67-6 and 67-7). Figure 67-7 The dog is positioned in dorsal recumbency for mandibular repair (the head and neck are slightly elevated with a positioning device, and the head is pulled rostrally); the upper jaw is secured near the end of the table with waterproof tape placed over the maxillary canine teeth (A); the tape and oral cavity are aseptically prepped in standard fashion, along with the skin of the ventral mandible. The wire reinforced endotracheal tube has bypassed the oral cavity by being placed through a right pharyngotomy (arrow); all anesthetic monitoring is performed at the tail end of the dog. The surgical field includes access to the mouth (to assess occlusion); surgical access is attained rostrally (B). Compare with Figure 67-6. Aseptic preparation of the surgical field, including the mouth, is accomplished by routine methods. Preparation of the oral cavity itself is accomplished by wiping the area, then rinsing; obviously, complete asepsis is not present in the mouth, thus the oral cavity is avoided whenever possible despite its inclusion within the surgical field. The eyes must be protected with an ophthalmic ointment. In simple fractures, in which endotracheal intubation per os is performed, the oral cavity is not included in the draping. In those cases in which occlusion is to be used to assess the reduction and the endotracheal tube bypasses the mouth, draping is performed to obtain full access to the oral cavity. Any tape within the oral cavity, used to secure the patient, is included in the preparation (see Figure 67-7). Although the fractured bone fragments often may be directly viewed within the mouth, because of the extensive lacerations of the gingiva that usually accompany these fractures, separate ventral approaches are the preferred surgical access.13,77–79,93 The ventral approach to each mandible facilitates exposure and bone fragment manipulation, including the ability to perform accurate reduction and stabilization.13,93 A separate lateral approach is required to expose the temporomandibular joint.13,80,93 The mandibular ramus dorsal to this joint need not be repaired. Skin incisions generally are made directly over the fracture in nasal, maxillary, or frontal areas (Figure 67-8). Dorsal midline incisions may be best for avoiding neurovascular structures along the nose and most easily exposing the maxillary buttresses.10,15 Fractures along the alveolar border may be approached directly by incising the gingiva a few millimeters away and parallel to the dental arcade. Usually one side of the head/face is more severely injured; therefore, a commonsense approach is to first repair the side with the simplest fractures. In most instances, the mandible is repaired first, and this serves as the “base” for subsequent facial repairs. The mandible should be repaired from caudal to rostral, with symphyseal separations secured as the last step. After mandibular reconstruction has been completed, the midfacial skeleton is subsequently addressed, with attention first on the lateral, and then on the medial, maxillary buttresses (in human beings, the medial buttress is addressed first to preserve midface height). Temporary maxillomandibular fixation will achieve occlusal realignment; this procedure thus will maintain appropriate orientation of the bone fragments and will function to provide a template for reconstruction and application of the definitive fixation. Securing the lateral and medial buttresses in this manner permits exact rostrocaudal positioning of the maxilla, along with correct height and projection. Caudal buttress reconstruction is unnecessary. All fractures must be fully visible by a direct surgical exposure to ensure accurate anatomic realignment of all bone fragments, thus enabling appropriate implant application for successful reconstruction of the entire face. This point cannot be overemphasized. The zygomatic arch can be approached directly.13,80 The lateral buttresses can be accessed from the dorsal midline. The lateral aspect of the frontal bone and the adjacent orbit can be approached by combining an approach to the zygomatic arch and reflecting the lateral soft tissue support to the eye and orbital ligament, which is attached to the zygomatic process of the frontal bone. In the presence of both maxillofacial and mandibular fractures, repair must begin in the area of the least severe fractures; most often, this is the mandible. The midface often is difficult to assess because the bone is thin and fractures frequently are essentially hidden, as the affected area is stable owing to fracture impaction and is difficult to manipulate. Because occlusion is the ultimate goal, a decision must be made to address the area that has better ability to be anatomically reconstructed, and then to use it as the base for subsequent repairs. The rationale for most often addressing the mandible first is that in most instances, these fractures are better defined owing to the structure of the bone and the greater ease of exposure, and thus of reconstruction. In some cases of stable (impacted) maxillofacial fracture in which the maxilla is slightly laterally displaced and stable (common in cats), the mandible can be realigned to match the maxillary dental arcade and to restore occlusion.1 Mandibular symphyseal repair (often a concomitant injury in the cat) may necessitate an intentional symphyseal shift; if the symphysis remains intact, it can be split to allow this shift to be performed.18 Maxillofacial repair, undertaken to restore the original anatomic configuration, can be accomplished with many techniques, including oral splints, interfragmentary wiring, standard plates, and miniplates. Two general methods are commonly used to obtain fracture fixation and restoration of function: (1) oral methods that utilize the teeth for the application of fixation devices, and (2) use of the bony skeleton itself. The former is addressed in Chapter 66; the latter is discussed here. This discussion is limited primarily to intraosseous wiring and plating techniques; the role of external skeletal fixation also is addressed. Miniplate fixation may provide the optimum environment for direct bone healing because of its ability to provide three-dimensional stability. In the mandibular and maxillofacial skeleton, implants must be placed at the most biomechanically favorable sites, so as to appropriately neutralize the tension forces and torsional moments that cause fracture distraction. The basic premise of wire fixation is to use intraosseous wire as a rigid suture to reappose and compress fractured bone fragments together. Intraosseous wiring techniques thus rely on the static forces generated by the tension of the wire and by the frictional forces between corresponding bone fragments.3,36,48 No stability is imparted in rotation or bending. Adequate stability for healing can be attained only with accurate anatomic reduction and sufficient neutralization of two broad, opposing bone fragments.3,48 Consequently, intraosseous wiring techniques are most successful if all bone fragments can be anatomically repositioned, thereby enabling the bone and implants to share any applied loads.3,36,48Significant comminution or bone loss precludes the ability to obtain such precise anatomic reapposition of all bone fragments, as it is not possible to achieve continuous interfragmentary compression across each/all bone fragments.3,36,48 Intraosseous wires provide only two-dimensional stability because rotation continues to occur around the wires as they are passed through holes of slightly greater diameter than the wire.3,36,48 Comminuted fracture reconstruction often fails owing to the difficulty encountered in anatomically reconstructing and appropriately securing all bone fragments. Wiring of multiple small bone fragments, although technically feasible, often is not attainable. With many small bone fragments, it is unlikely that anatomic reduction of each and every fragment will be attained. Similarly, any gaps in reduction preclude this method of fixation; attempting to bridge small gaps by spanning wires across a gap to adjacent bone fragments will not be successful, as this form of fixation cannot function as a buttress device. Failure to anatomically reduce the fracture fragments exactly will result in an unstable fixation. In this situation, the bone fragments are not brought into apposition resulting in insufficient contact between the two opposing bone surfaces. Consequently, the wires are ineffective in compressing these fragments together, and stability is not obtained. The end result is that the fixation becomes loose, with further loss of the marginal reduction obtained. Moreover, failure to anatomically reduce the bone fragments results in malocclusion. The biomechanical limitations of this fixation method must be fully appreciated. Implants are small and require application in tension, so as to compress two opposing fragments together. For effective fixation, intraosseous wires must be placed along the lines of tension stress, so that any distractive forces do not overwhelm the implants.25 Application of the tension band principle takes advantage of the fact that these fixation devices are strongest in tension.7 In mandibular fracture, the lines of tensile stress are along the alveolar margin; therefore, it is along this surface that wire fixation is most effective.25,63 Torsional and shear forces also exist, each most prominent rostrally and at the ramus, respectively. Therefore, in addition to the tension band wire along the alveolar bone margin, a second area of fixation must be considered along the ventral bone margin to effectively neutralize shear and rotation.25,61,63 The second wire often is referred to as a stabilization wire (Figure 67-9).13,93
Mandibular and Maxillofacial Fractures
Anatomic and Biologic Considerations
Teeth in the Fracture Line
Soft Tissue Considerations
Biomechanics
Mandible
Maxillofacial Skeleton
Teeth
Occlusion
General Anesthesia
Surgical Positioning
Surgical Approach
Maxillofacial Skeleton
Zygomatic Arch/Orbit
Sequence of Repair
Fixation Techniques
Intraosseous Wire
Mandible
< div class='tao-gold-member'>
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Mandibular and Maxillofacial Fractures
Only gold members can continue reading. Log In or Register to continue