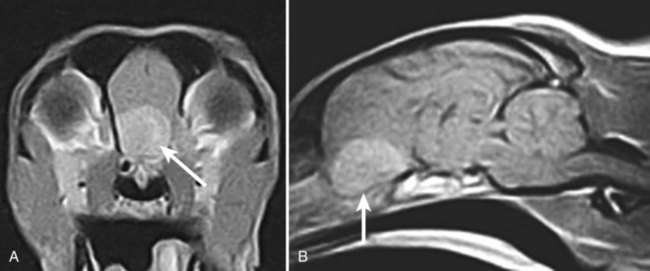
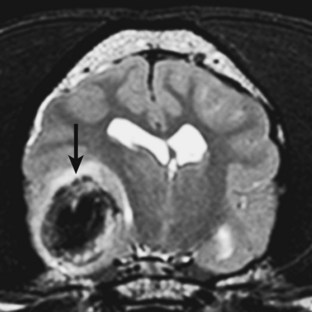
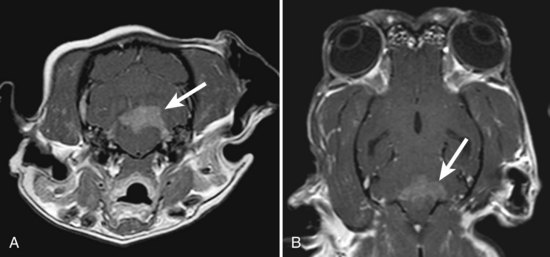
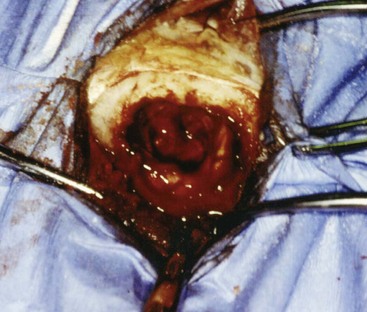
Chapter 36 Primary neoplasia of the central and peripheral nervous systems and secondary or metastatic neoplasms are commonly encountered in dogs and cats. Primary and secondary brain tumors will be considered in this chapter. Primary brain tumors can originate from brain parenchyma, the meninges, or the ependyma, as well as from vascular elements, including the choroid plexus.5,14 Secondary neoplasms involve the brain through metastasis or by direct extension from extraneural sites.5,14 Benign and malignant tumor types exist, and the definitive cause of primary and secondary brain tumors is uncertain. Meningiomas are the most commonly reported primary brain tumors in dogs and cats and are often histopathologically benign.5,14,29,32,57 Meningiomas are typically discrete tumors that are mesenchymal in origin.29,50 They most commonly arise from the arachnoid layer and expand inward; however, they can originate from the dura and pia mater.14,29,32,50 Extraneural metastasis is very rare, but metastasis to the lungs has been reported.48 In contrast to the well-encapsulated feline meningiomas, canine meningiomas tend to infiltrate the brain parenchyma, making them more difficult to remove surgically.* Multiple histologic subtypes of meningiomas are possible in dogs, including meningothelial, fibroblastic, transitional, psammomatous, angiomatous, papillary, granular cell, myxoid, and anaplastic (malignant) meningiomas.29,50 Fewer histologic subtypes exist for feline meningiomas.29 All subtypes, except anaplastic (malignant) meningiomas, tend to be slow growing.29,50 Gliomas are primary brain tumors that are reported frequently in dogs and less frequently in cats.5,14,57 Gliomas originate from the supporting cells (astrocytes and oligodendrocytes) of the brain parenchyma. 29,50 Variants of glioma include astrocytoma, oligodendroglioma, and the extremely malignant glioblastoma multiforme.14,32,45,50 In addition, choroid plexus tumors, primary central nervous system lymphomas, primitive neuroectodermal tumors (e.g., neuroblastoma), primary central nervous system histiocytic sarcomas, ependymomas, cerebellar medulloblastomas, vascular hamartomas, and, rarely, microglial tumors have been reported in the dog.5,14,29,32 In addition to gliomas, other less commonly reported primary tumors in the cat include ependymomas, olfactory neuroblastomas, cerebellar medulloblastomas, choroid plexus tumors, and, rarely, microglial tumors.29,50,57 On rare occasions, young dogs can develop a proliferative disorder of the leptomeninges referred to as meningioangiomatosis.8 This nonneoplastic disorder invades the brainstem and/or cervical spinal cord parenchyma by way of the perivascular spaces, ultimately mimicking a neoplastic process.8 Affected animals are typically middle aged or older (>5 years), with a median age of 9 years for dogs and >10 years for cats.2,5,14,32,57 Canine and feline patients with meningiomas tend to be older at diagnosis as compared with other primary brain tumor types.2,5,14,57 No apparent sex predilection exists for dogs; however, male cats are more likely than females to develop meningiomas.5,14,32,57 Golden Retrievers and Boxers are prone to developing primary brain tumors; however, any breed can be affected.2,5,14,32 Dolichocephalic dog breeds (e.g., Collies) are predisposed to meningiomas, whereas brachycephalic breeds (e.g., Boxers, Boston Terriers) seem more likely to develop gliomas.2,5,14,32 No obvious breed predilection exists for cats.57 Primary brain tumors are more commonly found in the cerebrum than in the brainstem or cerebellum.2,5,14,32 Approximately half of canine primary brain tumors occupy more than one anatomic region of the brain, often leading to the misconception of multifocal disease.2,49 Canine astrocytomas have a predilection for the diencephalon and cerebellum.5,14,32 Two subtypes of choroid plexus tumors exist: papilloma and carcinoma.29,50,52,58 They are differentiated on the basis of histopathology and the presence of metastases. Choroid plexus tumors of either subtype can develop in the lateral, third, or fourth ventricles. 29,50,52,58 According to one report, choroid plexus tumors tend to occur in the fourth ventricle, and only choroid plexus carcinomas occur in the lateral ventricles.52 It has also been reported that 23% of dogs with primary brain tumors have concurrent, unrelated neoplasia affecting the thoracic and abdominal cavities.49 On the basis of this finding, thorough screening for concurrent, unrelated neoplasia via three-view thoracic radiographs and abdominal ultrasound is recommended before advanced imaging and definitive brain tumor therapy are provided. Typically, the neurologic signs associated with primary brain tumors progress slowly over time; however, subacute to acute development is possible.5,32,49 Subacute to acute development of neurologic dysfunction is possible with sudden loss of the brain compensatory mechanisms, a subacute to acute hemorrhagic event, or acute obstructive hydrocephalus secondary to the tumor.14 Clinical signs vary and are governed by tumor location, in addition to various secondary effects such as hemorrhage and/or edema.5,14,32,49,57 Tumors involving the forebrain (cerebrum and diencephalon) are typically associated with seizure activity, behavioral changes, circling, head pressing, visual deficits, hemi-neglect (hemi-inattention) syndrome, proprioceptive placing deficits, and neck pain.14 Tumors affecting the brainstem (midbrain through medulla oblongata) can manifest as altered consciousness, dysfunction in cranial nerves III through XII, and obvious gait and/or proprioceptive deficits. 14 Cerebellar tumors are often associated with cerebellar ataxia, intention tremors of the head and/or neck, vestibular dysfunction, and menace deficits despite normal vision.14 In approximately one half of canine primary brain tumor cases, the primary complaint is seizures.5,14,32,49 The overall incidence of seizure activity in feline brain tumor cases was 23%, occurring more commonly with glioma (26.7%) and lymphoma (26.3%), in comparison with meningioma (15%).55 In one report, 20% of cats with primary brain tumors had nonspecific signs, including lethargy and anorexia, and 19% of primary feline brain tumors were incidental findings.55 The most common presenting complaint in cats is behavior change.5,14,55,57 Multiple meningiomas are possible in cats; therefore clinical signs may reflect multifocal neurologic dysfunction.19,55,57 As with any form of neoplasia, a definitive diagnosis of brain tumor cannot be made without histopathology. Several veterinary referral centers now have stereotactic computed tomography (CT)-guided biopsy available in an effort to obtain a definitive diagnosis at the time of imaging without the need for major intracranial surgery.28 A tentative diagnosis can be made with advanced imaging modalities, including magnetic resonance imaging (MRI) and CT. MRI is currently the preferred imaging modality for primary brain tumors. Blood work (complete blood count and chemistry panel), in addition to a urinalysis, three-view thoracic radiographs, and an abdominal ultrasound, should be performed before advanced imaging, in an effort to rule out metastatic disease and/or concurrent unrelated neoplasia. Certain characteristic features appreciated on MRI and CT can help to distinguish tumor types.30,31,39 Since meningioma arises from the dura and results in extra-axial compression, they are typically characterized by a broad-based, extra-axial mass effect. Additionally, meningioma typically demonstrates distinct tumor margins and uniform contrast enhancement (Figure 36-1).12,30,31,39 The normal brain parenchyma is usually displaced by the tumor. Certain meningioma subtypes calcify and thus can be detected on noncontrast CT images.30 Another characteristic feature of meningiomas appreciated on MRI is the “dural tail” sign.25 This contrast-enhancing meningeal “tail” extends from the primary tumor.25 Occasionally, meningiomas may have a cystic component extending from or contained within the primary tumor mass.4 In contrast to meningiomas, gliomas tend to arise from within the brain parenchyma (intra-axial) and grow toward the periphery of the brain. They often are highly infiltrative and invade the normal brain parenchyma, leading to a lack of distinct tumor margins and poor, nonuniform contrast enhancement (Figure 36-2).* Choroid plexus tumors and ependymomas tend to be intraventricular in location and often uniformly demonstrate contrast enhancement (Figure 36-3).12,30,31,39 “Ring enhancement” is characterized by peripheral contrast enhancement of a lesion which surrounds a nonenhancing central area of the lesion.59 This nonspecific imaging finding is associated with both neoplastic (gliomas) and nonneoplastic brain diseases.59 It is essential to recognize that imaging features are not pathognomonic for specific tumor types. For example, falcine meningiomas (originating from the falx cerebri) and those arising from the choroid plexus can appear to be intra-axial on MRI. Similarly, peripherally located gliomas can be mistaken for meningiomas. In a recent study, the accuracy of predicting primary tumor type in 20 dogs on the basis of MRI was 65%.47 Cerebrospinal fluid is often abnormal in patients with brain tumors; however, white blood cell counts and protein levels are variable and nonspecific for neoplasia.6 Because of this fact, the authors often do not pursue cerebrospinal fluid analysis if CT or MRI strongly suggests a brain neoplasm. Despite the fact that the risk of obtaining a cerebrospinal fluid sample under elevated intracranial pressure in a patient with a brain tumor is not high, the nonspecific result often does not alter the therapeutic plan or prognosis and is not worth the small risk to the patient. It is essential that imaging be performed to rule out concurrent cerebellar herniation before a cerebrospinal fluid tap is performed. Two main treatment categories exist for the management of primary brain tumors: palliative and definitive. The goals of palliative therapy are to reduce the secondary effects of the tumor, such as decreased peritumoral edema, and to treat seizures if present.6,14,40 Most palliative therapy consists of an antiinflammatory dose of oral prednisone (0.25 to 0.5 mg/kg q12h) that can be adjusted according to patient response. Prednisone therapy decreases intracranial pressure by relieving tumor-associated brain edema and by decreasing cerebrospinal fluid production.14 If the tumor results in seizure activity, anticonvulsant drugs are also recommended. Administration of standard phenobarbital doses in dogs with rostral forebrain tumors can lead to profound sedation.14 As an alternative, drugs without appreciable side effects, such as zonisamide (5 mg/kg PO q12h if patient is not concurrently on phenobarbital, or 10 mg/kg PO q12h if patient is on phenobarbital) and/or levetiracetam (20 mg/kg PO, IV q8h), are used for dogs with brain tumors, unless cost prohibits usage.14 Definitive therapy consisting of surgical removal/debulking, chemotherapy, and megavoltage radiation therapy is aimed at diminishing tumor volume or eliminating the tumor.40 Several features such as tumor size, degree of invasiveness, and tumor location can help the clinician determine whether surgical resection is an option.5,14,15,20,42 As expected, intra-axial tumors are significantly more difficult to remove than extra-axial tumors. Benefits of surgery include removal of cancerous tissue, an immediate decompressive effect, and a definitive diagnosis via histopathology.5,14,15,20,42 A definitive diagnosis provides prognostic information and, in the case of subtotal resection, allows further treatment planning.20 Various surgical approaches have been described, including rostrotentorial, caudotentorial, transfrontal, and suboccipital craniectomy.5,15,20,24,42 The surgical approach can consist of one of the aforementioned techniques, or it can combine several different approaches with the goal of removing the entire mass. The approach is governed by tumor size, location, and degree of invasiveness. Most brain tumors in dogs and cats are removed via standard rostrotentorial craniectomy (Figure 36-4). Suboccipital craniectomy is discussed in Chapter 37. For a rostrotentorial craniectomy, the authors prefer a midline incision on the head from approximately the level of the lateral canthi to several centimeters caudal to the external occipital protuberance. The cutaneous colli muscles are sharply incised and the cervicoscutilaris muscle is transected near midline, leaving about a centimeter for reattachment during closing. The temporalis fascia is sharply incised with a #11 blade, leaving at least several millimeters attached to the external sagittal crest for reattachment purposes. The temporalis musculature is reflected ventrally by elevation off the side of the skull with a Freer elevator (cats and small dogs) or a more sturdy instrument such as a Sayre, AO style, or Langenbeck periosteal elevator (large dogs). An oval outline of the intended defect in the calvaria is created with a high-speed air drill. The edges of this outline are deepened until a thin layer of periosteum is left. The ventral aspect of the defect does not have to be drilled full thickness. Once the bone along the dorsal, rostral, and caudal aspects of the craniectomy defect has been completely drilled to the inner periosteum, a periosteal elevator, positioned in the dorsal margin of the defect, is used to lever off the bone flap. The craniectomy defect can be further enlarged with the use of rongeurs once the bone flap has been removed. After removal of the bone flap, any bleeding meningeal vessels are cauterized using bipolar cautery.
Intracranial Neoplasia
Primary Brain Tumors
Diagnosis
Treatment of Primary Brain Tumors
< div class='tao-gold-member'>
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Intracranial Neoplasia
Only gold members can continue reading. Log In or Register to continue