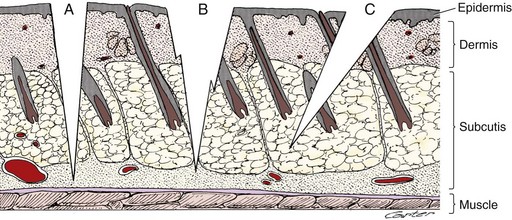
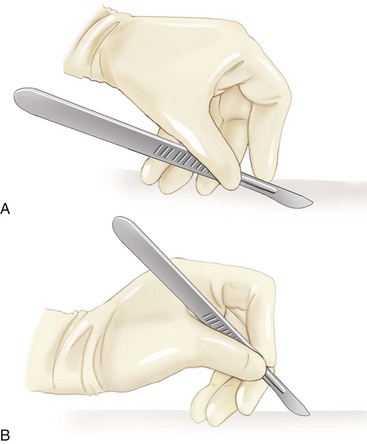
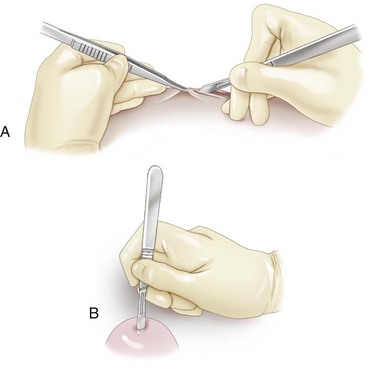
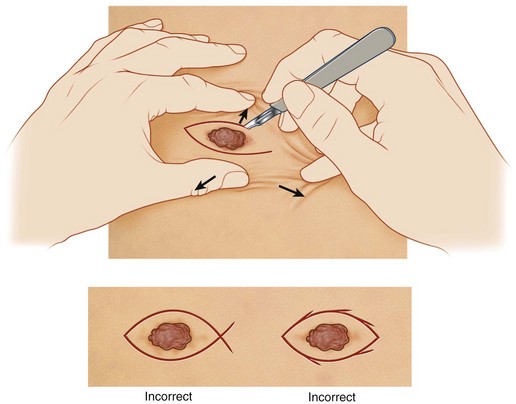
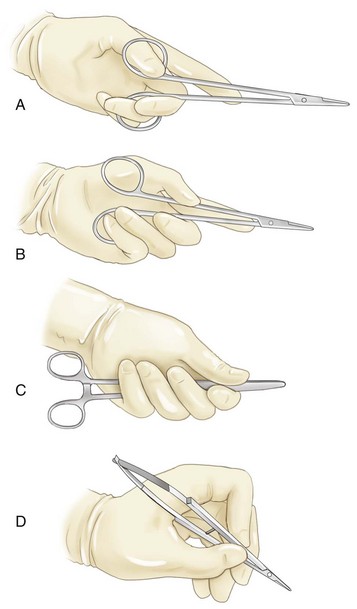
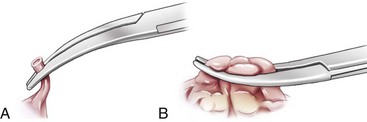
Chapter 18 A very desirable attribute of a good surgeon is a sense of fluency that is achieved by being familiar with the tools of the profession and being able to use them appropriately for the task at hand.26 Good surgery begins before any incision is made, with consideration of the equipment needed and the approach to be used.20 Good surgical technique is important because it affects outcome.12 Many surgeons refine techniques throughout their careers, with necessary emphasis on gentleness.22 The surgeon should strive to discover the simplest and safest way to achieve the operative goal.20 Heuristics are elements of a skill, and they are an essential part of safe and expert performance, including surgery.21 Heuristics apply to the elements of manual or perceptual skills that are used during surgical dissection. Three types of heuristics used in surgery are cognitive (planning movements before performing them), perceptual (recognizing tissues), and motor (handling tissues).21 Perceptual heuristics involve the trained eye that is needed to recognize the presence, site, and extent of structures and their individual properties.21 Haptics, a form of perceptual heuristics, is the study of how perceptions mediated by the hand provide feedback that facilitates performance of a skilled action by the hand.21 An example of a motor heuristic is the way that surgeons cut through tissues at right angles to lines of tension.21 Movements in surgery are nearly all incremental, and there is a trade-off between speed and accuracy. The good surgeon does not necessarily make quicker movements; such movements are performed effectively and with purpose. Hence, the good surgeon performs the task of surgery with less repetition and fewer mistakes than the novice surgeon. The use of heuristics to develop, validate, and train both present-day and future surgeons has been suggested.21 Attainment of safe, efficient, and reproducible surgical technique depends on comprehensive knowledge of the following surgical skills: instrument handling, tissue dissection and manipulation, suturing, knot tying, hemostasis, and wound closure.20 The first four surgical skills (instrument handling, tissue dissection and manipulation, suturing, and knot tying [including ligation techniques]) are discussed in this chapter; the latter two (hemostasis and wound closure) are discussed in chapters 19 and 75, respectively. Instrument handling should be performed safely and in a way that avoids unnecessary maneuvers.20 Surgical instruments, with appropriate use, are designed to help the surgeon follow Halsted’s principles (Box 18-1). The principles most affected by proper instrument use are related to gentle tissue handling and sharp dissection of tissues. Instruments are designed, in terms of both form and size, to be used in specific ways to safely manipulate specific tissues.11 Correct selection and use of instruments helps the surgeon protect tissues from crushing, drying, heat loss, hemorrhage, and loss of vascular supply.11 A defective, nonfunctioning instrument can compromise patient safety and may delay the procedure.8 Recommendations for manipulating articulating and nonarticulating instruments have been put forth.1 Articulating instruments with ring handles (e.g., needle holders) should be manipulated using the fingertips, not the mid-digit. Such a grip improves both efficiency and effectiveness. Nonarticulating instruments (e.g., thumb forceps) are manipulated as extensions of the thumb and forefinger, usually of the nondominant hand, and between uses are positioned in the palm of the nondominant hand.1 Hand tremor and unwanted body movements are minimized by the site and proximity of support provided to the hand or instrument when the work is being performed.10 The unsupported distance between the fulcrum and the tips of the instrument or the fingers should be shortened by supporting the hand or instrument close to the target tissue. Additionally, use of excessive force (e.g., pushing, gripping too hard) increases the amplitude of hand tremor. Controlling the accuracy of hand movement is a particular concern in all areas of surgery, including endosurgery.21 Scalpels are used to make incisions in the skin and other tissues. The cutting edge of the more commonly used scalpel blades (i.e., #10 and #15) is at the center of the blade, and the tip is generally used as the cutting edge with the #11 blade. The scalpel blade and the subsequent incision should be oriented perpendicularly to the skin. Full-thickness skin incisions attained with a single sweep of the scalpel blade are the goal (Figure 18-1).11 When tissues are incised, the scalpel handle is usually held in one of two ways: fingertip grip or pencil grip (Figure 18-2). The fingertip grip places the maximum length of the blade edge in contact with the tissue.1 It offers the greatest accuracy and stability in making long incisions, as movement is performed by the whole arm. The pencil grip, which uses finger motion, is more accurate for short, delicate maneuvers. Four motions of the scalpel’s cutting edge may be used in surgery: sliding, pressing, sawing, and scraping.1 Slide cuts yield precise depth, length, and control of direction and are used most commonly for making skin incisions.1 Press cuts or stab incisions are useful for opening fluid-filled chambers or making initial entry into a body cavity (Figure 18-3). Pressure and motion occur in the same direction with a press cut, but depth is poorly controlled.1 Sawing (e.g., transecting a ligated pedicle) allows continuation of a cut without removal and reinsertion of the blade. The novice surgeon may use a sawing motion when incising the skin. Such poor technique leads to unnecessary tissue trauma and, frequently, to delayed wound healing.11 Scraping is a method of separating tissue layers. The latter two motions are used selectively by experienced veterinary surgeons. Scalpel incisions result in less crushing of tissue compared with scissor incisions. Stabilize tissues when incising with a scalpel by using the tips of the thumb and forefinger of the nondominant hand to tense adjacent tissue (Figure 18-4). Both lateral and longitudinal traction aids in creating accurate full-thickness skin incisions with the scalpel. Curved incisions should be made with no abrupt change in direction (see Figure 18-4).1 Scissors are used to cut or dissect tissue and to cut inanimate objects, including paper drapes and suture material. Cutting of inanimate objects should be limited to specific instruments. To maintain functionality, scissors should be used only for their intended purpose. Three forces are used when cutting with scissors: closing, shearing, and torque.1 Closing force causes the blades to come together; shearing force pushes one blade flat against the other during closing; and torque rolls the leading edges of each blade inward to touch the other.1 When standard surgical scissors are used, creating shearing force is a natural action for the right-handed surgeon, but it requires effort and practice on the part of the left-handed surgeon.16 The gripping motion effectively combines these three forces to create precise cuts. A tripod grip is recommended when using scissors, because it provides maximal control. A tripod grip is achieved by inserting the tips of the thumb and ring finger through the rings and placing the index fingertip near the fulcrum (Figure 18-5).1 Curved scissors offer greater maneuverability and visibility, whereas straight scissors provide greater mechanical advantage for cutting dense tissue.1 Metzenbaum and Mayo scissors are used to cut and dissect tissues; utility or operating scissors are usually used to cut inanimate objects. Metzenbaum scissors are reserved for more delicate tissues. Mayo scissors are sturdier and are used on heavier connective tissue.19 Scissors are excellent dissection instruments, in part because of their excellent direction control and accuracy, particularly in flaccid tissues; however, their efficient use requires practice. Scissors are used for dissection of two types: sharp or blunt. Sharp dissection may be accomplished by a conventional double-blade cutting action or by forcing the semi-opened tips through the tissue carefully and steadily in one continuous motion (push-cutting).11,16 When cutting with double-blade cutting action, take care to create a straight incision, regardless of the shape of the scissor tips. Cutting nearer the scissor tips provides less closing force but more secure stability of the tissue.1 When scissors are opened too widely and tissues engage the blades closer to the fulcrum, cutting forces are greatly attenuated.29 Cutting tissues with the portion of the blade near the fulcrum (i.e., deep within the jaws) results in greater crushing injury to the tissue, jagged incisions, and potential inadvertent trauma to adjacent tissues.1 When continuing an incision with scissors, one should not completely close the blades. Instead, the scissor blades should be nearly closed, advanced, and closed again. Scissors with appropriate tips (e.g., sharp-sharp) are ideal for blunt dissection.1 Blunt dissection is accomplished by inserting the closed tips of scissors into lax tissues and then opening and withdrawing the points to break down connections and define important structures.11,14 Scissors have an advantage over forceps for blunt dissection, as alternating blunt and sharp dissection can be performed without changing instruments.1 Blunt dissection, in general, should be minimized, as excessive dead space and tissue trauma may result. The most controlled cut with bone-cutting chisels and osteotomes is induced by a mallet.1 Holding the cutting instrument by using a palmed grip in the nondominant hand helps guide the direction of the cut. Curettes are held in a pencil grip and are manipulated by using back-and-forth rotating motions or pulling strokes.1 Periosteal elevators are usually manipulated by using a controlled pushing stroke.13 Bone-cutting forceps are manipulated by using a palmed grip with the dominant hand. The configuration of grasping instruments, a stable yet mobile union of two pieces of metal via a pivot, transfers manual power efficiently to the jaws.15 The final power developed depends on four factors: leverage at the pivot, the shape and area of jaw contact, the elasticity of the handles and jaws, and the effect of ratchets.15 Although needle holders are used only on inanimate objects, they indirectly affect the degree of tissue trauma produced by having an impact on both the surgical needle and surgical efficiency. Inefficient use of the needle holder accounts for more wasted time than poor technique with any other surgical instrument.1 Self-discipline in mastering the 10 steps associated with suturing, to a greater extent than skill, is required to use a needle holder efficiently.1 Combination needle holder and scissors (e.g., Olsen-Hegar) may be preferred by solo surgeons because of the potential for enhanced efficiency. Additionally, needle holders should grasp only that portion of the suture stand that is distal to the impending knot. Grasping other portions of the suture stand is likely to weaken it. Four grips may be used in manipulating the needle holder: thumb–ring finger (tripod), thenar, palmed, and pencil grip.1 The thumb–ring finger (tripod) grip (Figure 18-6, A) provides for precise needle grasping and release and is well suited for delicate work. When the thenar grip is used, the needle holder is grasped between the ball of the thumb (thenar eminence) and the ring finger (Figure 18-6, B). The metacarpophalangeal joint of the thumb helps control one ring, while the tip of the ring finger controls the other ring of the needle holder. This grip tends to save time during placement of continuous patterns, but needle release is often less precise than with the thumb–ring finger (tripod) grip. The palmed grip (Figure 18-6, C) is the strongest grip, provides the greatest needle pressure and control in dense tissue, and provides for maximal wrist rotation; however, needle release and grasping often require adjusting to another grip, as neither ring is immediately accessible to fingertips.1 The pencil grip (Figure 18-6, D) is best suited for needle holders with spring handles (e.g., ophthalmic needle holders). It allows needle control with fine digital movement. Both Allis and Babcock tissue forceps have a plane of grip that is perpendicular to the direction of pull. They each have a crushing effect on tissue and should not be used on tissue slated to remain with the patient. Kocher forceps may be used on more dense tissue that is to be excised. Crushing-type tissue forceps are most suitable for static tissue holding during dissection around the secured tissue.26 Although considered to be a noncrushing tissue forceps, Doyen intestinal forceps, particularly as duration of application increases, induce tissue trauma. Doyen intestinal forceps are most frequently used by the solo surgeon to occlude the intestinal lumen and prevent intraoperative contamination during enteric procedures. Digital intestinal occlusion by an assistant provides an alternative, seemingly less traumatic, method.25 In part because of their small size and atraumatic nature, various peripheral vascular forceps (e.g., patent ductus arteriosus clamp) may be used to achieve temporary intestinal occlusion in selected instances (e.g., feline subtotal colectomy). Cardiovascular forceps provide tissue occlusion without cutting or crushing the blood vessel wall.11 When they are used on larger blood vessels (e.g., vena cava), only a selected portion of the vessel is occluded. The portion of the vessel not enclosed in the clamp maintains blood flow. Hemostatic forceps are used frequently during surgical procedures, either to isolate bleeding points or to bluntly dissect tissue.26 Hemostats may be used in either of two clamping techniques: tip clamping or jaw clamping (Figure 18-7). In general, hemostats with transversely oriented serrations (e.g., Halsted mosquito, Crile, Kelly forceps) are designed to grasp small amounts of tissue with the tip of the forceps directed toward the open vessel. Forceps with longitudinally oriented serrations (e.g., Rochester-Carmalt forceps) are designed to grasp larger amounts of tissue (e.g., ovarian pedicle) with the jaw, such that the tip of the forceps is pointing away from the vessel.1 Although jaw clamping facilitates placement of ligatures during tying, it also results in increased tissue trauma.1
Instrument and Tissue Handling Techniques
Instrument Handling
Use of Cutting Instruments
Scissors
Other Cutting Instruments
Use of Grasping Instruments
Needle Holders
Crushing-Type Tissue Forceps
Noncrushing-Type Tissue Forceps
Hemostatic Forceps
< div class='tao-gold-member'>
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Instrument and Tissue Handling Techniques
Only gold members can continue reading. Log In or Register to continue