Ann Rashmir-Raven, Annette Petersen
Hypersensitivity Diseases
Allergic dermatitis is encountered on a regular basis in equine practice. Urticaria and pruritus are the most commonly recognized clinical signs. Severely affected horses may become difficult to ride or manage because of the intensity of their symptoms. The ability to diagnose and treat common causes of allergic dermatitis should prove useful to the practicing veterinarian and improve the overall quality of patients’ lives. Individual horses, like humans and animals of other species, often have a combination of allergies and may be sensitive to multiple allergens, such as insect bites, pollens, food, and other environmental antigens. Addressing multiple factors is usually necessary to obtain adequate long-term control.
Urticaria or Hives
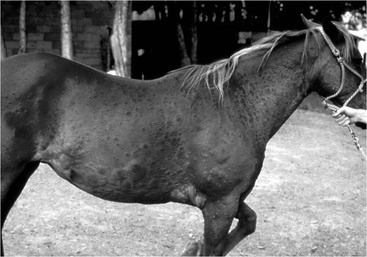
Horses develop urticaria more often than any other species. Urticarial lesions are predominantly caused by degranulation of dermal mast cells that release a variety of biologically active compounds, including histamine, platelet-activating factor, and prostaglandins. These compounds cause relaxation of vascular smooth muscle cells and retraction of endothelial cells, which allows plasma to extravasate and form wheals (localized edema within the dermis). Nonimmunologic (physical) urticaria can be caused by heat, cold, pressure, and exercise. In most urticarial lesions, the skin surface itself appears normal (Figure 132-1); however, if the dermal edema is severe, the serum may ooze to the skin surface and cause focal crusting and matting of the hair coat with subsequent focal hair loss. Urticarial lesions manifest as acute singular eruptions or waxing and waning eruptions, or the animal may experience chronic recurrent urticaria for longer than 6 to 8 weeks. Wheal formations vary in size from 2 to 3 mm to up to 20 to 40 cm in diameter. Papular wheals (3 to 6 mm in diameter) are frequently associated with biting insects—especially mosquitoes—whereas giant wheal formation or polycyclic (irregularly shaped) urticaria may be more frequently associated with adverse reactions to drugs. Annular wheals resemble doughnuts, with a ring of edema surrounding a central depression that is nonedematous. Angioedema is more diffuse edema affecting the dermis and subcutis. Classic urticarial and angioedema lesions resolve within 24 to 48 hours but may recur.
In warm climates, insect bites are arguably the most common cause of urticaria in the horse, but other environmental allergens such as pollen may be the underlying cause in any climate. In rare instances, adverse drug reactions or food allergies can incite the reaction. Insect bite hypersensitivity manifests as mild to intensely pruritic dermatitis and is usually seasonally recurrent, although severely affected horses in southern climates may not enjoy seasonal relief. Pruritus is the result of a local inflammatory response provoked by salivary antigens of biting insects. It is mediated by immunoglobulin E (IgE) and leads to degranulation of mast cells, and basophils, which results in the release of histamines, interleukins, prostaglandins, kinins, and other inflammatory mediators. Insect hypersensitivities tend to increase in severity and in the number of days affected with each subsequent year. Insects most frequently involved in these hypersensitivity reactions are Culicoides spp (midges or “no-see-ums”), Simulium spp (“black fly”), Haematobia irritans (“horn fly”), and Stomoxys calcitrans (“stable fly”). Other parasites that are less commonly implicated include horse flies, mosquitoes, and Onchocerca cervicalis. When Culicoides flies are involved, the disease is sometimes referred to as “sweet itch” or “Queensland itch.” Culicoides hypersensitivity appears to be more common in certain breeds, such as Shire horses, Welsh and Shetland Ponies, and Arabian horses. Icelandic horses imported to the European continent as adults are particularly sensitive, with more than 50% developing insect bite hypersensitivity. Icelandic horses that are born in Europe have a 5% prevalence rate, similar to that of other breeds. Interestingly, weanlings that move to Europe and are exposed to the Culicoides allergen by 7 to 10 months of age are not at higher risk for developing insect bite hypersensitivity than horses of other breeds. Because Culicoides spp are not found within Iceland itself, horses that migrate out of Iceland as adults do not develop immune tolerance and are therefore the most problematic. Clinical signs of Culicoides hypersensitivity are similar to those of other insect bite hypersensitivities, with a higher incidence of lesions along the dorsal and ventral midlines and the mane and the base of the tail.
In addition to urticaria and pruritus, other classic clinical signs of insect bite hypersensitivity include rubbing of the mane and tail, excoriation, scabs, and hair loss. Depending on which insect is primarily involved and their preferred feeding site, the distribution of the lesions can include the ventrum, face, legs, rump, or a combination.
Atopy
Atopy is an inherited dermatologic condition (atopic dermatitis) and less commonly a respiratory condition (perhaps contributing to recurrent airway obstruction). Horses with atopy form sensitizing antibodies (mostly IgE) against environmental antigens, including grasses, weed and tree-pollens, dust mites, molds, and feathers, and rarely against cotton, wool, and other fibers. Arabians and Thoroughbreds in early adulthood appear to be genetically predisposed to the disease. Similar to the mechanism in insect hypersensitivity, mast cells within the skin or respiratory tract are bound by the sensitizing antibodies. Antigen cross-links the IgE, causing the mast cell to degranulate and release inflammatory mediators. The release of these mediators, and their subsequent effect on other cells, leads to pruritus.
Atopy may be seasonal or nonseasonal, depending on the specific allergens involved. Clinical signs are similar to those of insect hypersensitivities and include alopecia, self-induced excoriations (Figure 132-2), crusts, scales, erythema, urticaria, lichenification, and hyperpigmentation. Areas most commonly affected are the face, ears, ventrum, and limbs. Horses may develop secondary pyoderma, resulting in crusted papules or excessive scaling.
Differential diagnoses include ectoparasite infestation and other types of hypersensitivities (e.g., insect or food allergies). For diagnosis of atopy, the horse’s history and physical examination must be compatible with atopic dermatitis, and other causes of pruritus must first be eliminated. Intradermal testing (IDT) with locally important allergens can be of benefit, but is not required to diagnose atopic dermatitis. Intradermal testing has been validated for these purposes in the horse and assesses tissue-fixed IgE, rather than IgE circulating in the blood.
Even though IDT is currently considered the gold standard, some false-negative or false-positive reactions may still occur. In cases in which skin testing is not available, one of the authors (AP) is of the opinion that serum testing for environmental allergens may be better than no testing (to be able to pursue subsequent immunotherapy). For both intradermal and serum testing, after particular allergens are determined, the best treatment is clearly to avoid exposure. Unfortunately, this is not always possible, and allergen-specific immunotherapy (hyposensitization) can be a useful tool in a successful long-term treatment plan for atopic dermatitis and in some cases of recurrent airway obstruction. Otherwise, glucocorticoids, antihistamines, and omega-3 or omega-6 fatty acids (see Treatment) used in combination are likely to provide the best long-term control.
Food Hypersensitivity
Food hypersensitivity is a cutaneously manifested adverse reaction to food. Although the role of food materials in allergic disease in horses is controversial, it is safe to say that, in addition to ingestion, feedstuffs can cause hypersensitivity by contact (i.e., the horse gets the feedstuffs on its body as it eats or lies in its stall). Food allergies or so-called grain bumps may be more common in young racehorses, although no breed, sex, or age predilections actually have been documented. Depending on the allergen involved, food hypersensitivities may be seasonal or nonseasonal. Generalized or multifocal pruritus and urticaria are the most common clinical signs, and gastrointestinal signs may also occur. Secondary lesions, such as crusting and exudative excoriation, are the result of self-inflicted trauma. Flaking and skin thickening (lichenification) may develop in chronic cases. The face, neck, trunk, and hindquarters are most commonly affected, but the tail and perianal areas may also be involved.
Skin biopsy specimens usually reveal nonspecific perivascular dermatitis with eosinophilia. These lesions are identical to those seen in specimens from horses with any other allergic skin disease and therefore do not help distinguish between the different types of allergies (e.g., insect, environmental, or food allergens). Instead, the diagnosis of food allergy is made by removing the feed material suspected of causing the problem from the horse’s diet, stall, and neighboring environment. Horses should undergo a 4- to 6-week dietary trial in which the horse’s diet is gradually altered to remove the offending agents without risking an episode of colic. All grains and supplements should be removed. The hay should be changed from grass hay to alfalfa, or vice versa, depending on what the horse was consuming previously. After the horse’s clinical signs are under control, reintroduction of feedstuffs may be attempted. Exacerbation of clinical signs usually occurs within 24 to 72 hours but may take much longer. Intradermal testing and allergen-specific serologic allergy tests (radioallergosorbent test, enzyme-linked immunosorbent assay) are not useful in the diagnosis of food hypersensitivity in the horse and cannot be recommended. Attempts at hyposensitization for equine food allergy are similarly not recommended. Dietary and environmental restrictions (e.g., access to pasture), along with administration of glucocorticoids, antihistamines, and omega fatty acids, may be beneficial. In cases in which direct skin contact with the food allergen is believed to contribute to the problem, bathing the horse in cool water with colloidal oatmeal shampoos is recommended. If oats are a suspected antigen, the oatmeal shampoo is omitted and replaced with pramoxine shampoo.
Contact Hypersensitivity
Contact allergies are rare in horses but may develop as the result of exposure to plants, bedding, topically administered agents (e.g., shampoos, insecticides, hoof paints, medications), and tack. When a contact hypersensitivity has developed, it generally persists indefinitely, and any future contact with the allergen will result in a dermatologic reaction within 1 to 3 days. In rare instances, the horse was exposed to the offending substance more recently. In most cases, the horse suddenly develops a hypersensitivity to a substance to which it has been exposed for years without any previous problem. Contact hypersensitivity clinically manifests as vesicles and papules that rupture, leaving an erythematous oozing and crusting on the skin surface with associated alopecia and subsequent lichenification of the skin in chronic cases. Urticaria can also develop. The distribution of the lesions depends on the causative allergen and is the most important clue for suspicion of a contact allergy. If a plant is the offending allergen, lesions will be found on areas such as the muzzle, pasterns, and fetlocks, areas that are in contact with grazing materials. Contact allergy to the saddle or the girth causes lesions where the tack contacts the skin. If the signs are generalized, a shampoo or insecticide should be suspected. Ectoparasites and the previously mentioned hypersensitivities should be considered in the differential diagnosis. The suspected material should be removed for 7 to 10 days. For example, in horses in which an allergic response to bedding is suspected, a trial of paper bedding is usually recommended. If signs regress, direct contact with the substance can then be allowed to observe for signs of recurrence, which provides a definitive diagnosis. When contact hypersensitivity is suspected, the affected area should be washed and the allergen should be avoided. If the causative agent cannot be identified, oral or topical glucocorticoids can be used to reduce inflammation.
Drug Eruption
Drug eruption describes a cutaneous adverse reaction of the skin to any chemical compound that gains access to the skin by ingestion, injection, inhalation, or topical absorption. These reactions may occasionally occur on first exposure to the drug, but the reaction itself may be delayed for weeks or months. Most commonly, however, the onset of the reaction occurs within 24 to 48 hours of drug administration. Drugs most likely to be involved in these eruptions are those most commonly used in equine practice and include nonsteroidal antiinflammatory agents, antibacterial agents (especially penicillin and sulfonamides), phenothiazine-based tranquilizers, diuretics, and local anesthetic agents. Features commonly associated with drug eruptions are urticaria and angioedema, diffuse erythema, bilaterally symmetrical lesions, papular eruptions, intense pruritus, sharply demarcated erosions and ulcerations, vesicular and bullous eruptions, photosensitization, and noninflammatory acquired alopecia. After the drug is discontinued, signs may persist for varying amounts of time, ranging from several hours to more than 6 months. Differential diagnoses to consider include other types of the previously mentioned hypersensitivities, systemic lupus erythematosus, and pemphigus foliaceus. Exposure to the causative drug and drugs from the same family should be carefully avoided in the future.