Amber L. Labelle
Glaucoma
Glaucoma, one of the most challenging ocular diseases for the equine practitioner to diagnose and treat, almost inevitably results in vision loss despite provision of aggressive and appropriate treatment. For this reason, referral to a veterinary ophthalmologist is indicated for most cases of glaucoma in horses. If referral is not an option, consultation with a veterinary ophthalmologist is strongly recommended. Research into the pathogenesis of this serious condition is vital for the continued development of novel and efficacious therapies. This chapter discusses the etiopathogenesis, clinical signs, diagnosis, and treatment of glaucoma in horses.
Glaucoma Pathophysiology
Intraocular pressure (IOP) results from the balance of aqueous humor production by the ciliary body epithelium and drainage from the eye through the two major routes of aqueous humor outflow: the iridocorneal angle (conventional pathway) and the uveoscleral outflow pathway. Unique to the horse is the importance of the uveoscleral outflow pathway; approximately 50% of aqueous humor leaves the eye by this route. Glaucoma consists of a series of pathologic events in the eye that culminates in IOP increase, optic nerve damage, and vision loss. In humans, forms of glaucoma are recognized that result in optic nerve degeneration with vision loss in the absence of IOP elevation; such forms of glaucoma have not been documented in the horse, and elevation in IOP is thought to be the major risk factor for glaucomatous optic nerve damage in equine patients.
Glaucoma in veterinary patients is classified as congenital, primary, or secondary. Congenital glaucoma has been reported but is exceedingly rare in horses. Primary glaucoma has not been described in the horse, and experienced veterinary ophthalmologists doubt its existence. In humans, primary glaucoma is thought to be genetic in origin and results from resistance to aqueous humor outflow at the level of the iridocorneal angle with subsequent IOP elevation. Secondary glaucoma is likely the most common form in the horse. It is caused by concurrent intraocular diseases such as chronic uveitis, intraocular neoplasia, or retinal detachment. Although equine recurrent uveitis (ERU) is the most common intraocular disease associated with secondary glaucoma, the precise mechanisms associated with etiopathogenesis are poorly understood.
Clinical Signs of Glaucoma
The clinical signs of glaucoma can be variable, and acute signs differ from signs seen with chronic glaucoma. Unlike other domestic species, horses can maintain vision despite having a high IOP for a comparatively long period of time; thus, the degree of visual deficit may be variable at the time a horse is evaluated. Assessing vision in horses is challenging. The menace response is the most basic test for assessment of vision, but it has the potential for both false-positive and false-negative results. Careful assessment of the menace response from all visual fields should be made. A dazzle reflex, assessed by shining a very bright, focused light into the eye and observing an avoidance response, which may include closing the eyelids, retracting the globe, or moving the head, gives the practitioner useful information about retinal function. Although a positive dazzle reflex is not synonymous with vision, it does indicate that some retinal function is present. A negative dazzle reflex is a poor visual prognostic indicator. Observing the horse navigating an unfamiliar environment under bright and dim lighting conditions is helpful for detecting visual deficits but is difficult to perform in the farm environment to which the horse has already become accustomed. Setting up a simple obstacle course, including large objects that require avoidance (trash cans) or objects that require stepping over (poles on the ground), may provide useful information about visual performance.
The degree of pupillary light reflex deficit varies in horses with glaucoma. Horses with concurrent intraocular inflammation may have miotic pupils, whereas those with end-stage retinal or optic nerve damage will have mydriatic pupils. Posterior synechiae may create dyscoria (abnormally shaped pupil) or make pupil size discordant with the concurrent ocular disease (i.e., a miotic pupil in an end-stage glaucoma eye).
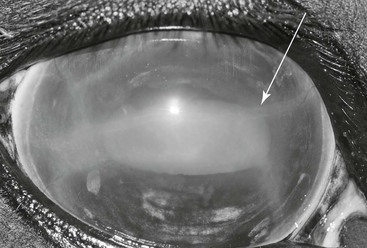
Many horses with glaucoma do not have classic signs of ocular pain, including blepharospasm and epiphora. Mild to moderate conjunctival hyperemia and episcleral injection are common. Mild to severe diffuse corneal edema is frequently observed. Corneal edema may be segmental, starting in vertical stripes in the central cornea and then progressing to diffuse edema. Edema likely results from physical distortion of corneal stromal fibers and dysfunction of the endothelium. Edema may also be linear and traverse the cornea. Descemet’s striae (also called corneal striae or Haab’s striae), areas of discontinuity in Descemet’s membrane, may later appear at these sites of linear edema (Figure 144-1). Severe edema may be associated with bullae, or fluid-filled subepithelial blisters. These bullae may rupture and lead to corneal ulceration. Superficial perilimbal corneal vascularization may be observed, with vessels extending several millimeters from the limbus toward the axial cornea. Keratic precipitates, pinpoint conglomerates of fibrin and inflammatory cells, may or may not be present on the corneal endothelial surface.
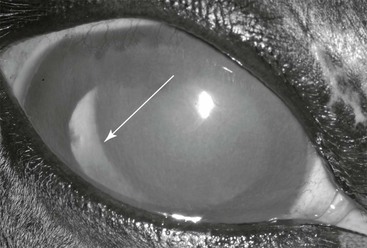
Intraocular examination of horses with diffuse edema is often challenging. Lowering the ambient lighting to as dim a level as possible and aiming the light source across the anterior chamber from limbus to limbus (using indirect vs. direct illumination) is helpful for visualizing intraocular structures. Intraocular examination findings may be consistent with ERU, including hyperpigmentation of the iris, blunting or atrophy of the corpora nigra, dyscoria, posterior synechiae, aqueous flare, and cataract. The iridocorneal angle is most easily examined at the lateral limbus, where the opening of the trabecular meshwork is visible just axial to the limbus. A normal iridocorneal angle has the appearance of a kitchen sponge, with strandlike pectinate ligaments visible as a meshwork traversing the opening of the angle. An abnormal angle may appear recessed beneath the scleral shelf or sclerotic, with a band of white fibrous tissue replacing the normal pectinate ligaments. No information correlating the appearance of the iridocorneal angle with the onset of glaucoma or prognosis is available in horses. Lens subluxation or luxation may result from chronic stretching of the glaucomatous globe and subsequent zonular degeneration (Figure 144-2).
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree