The vagina, vestibule, prepuce, and distal urethra have a resident microflora. The oral and anal flora of neonatal puppies correlate with the flora from the milk, vagina, and oral cavity of their dams. The flora of puppies from different dams varies with the dam.273 Bacteria are not normally found in the upper urinary tract, bladder, proximal urethra, or prostate gland.23,170 Bacteria are not normally found in the uterus, except during proestrus and estrus.71,93,93 The clinical importance of the microflora is twofold: first, it must be considered when the results of cultures of urine, semen, and preputial and vulvar discharges are interpreted; second, the normal microflora is thought to be an important factor in host defense against pathogenic organisms. The resident microflora competes with pathogenic bacteria for nutrients and can interfere with adherence of pathogenic bacteria to vaginal epithelial receptors. Lactobacilli isolated from the vagina of dogs showed antimicrobial activity against Proteus mirabilis, Staphylococcus aureus, and Escherichia coli.91 In clinically healthy male dogs, commensal bacteria cultured from the distal urethra and prepuce include gram-positive and gram-negative organisms (Boxes 90-1 and 90-2).22 Mycoplasmas are found in the distal urethra and the prepuce and have also been isolated from the canine prostate. When sampling the prepuce, usually more than one organism is recovered; however, only a single species is obtained in about 20% of preputial and semen samples.48 The prostatic fraction of a cleanly collected ejaculate from healthy, fertile stud dogs is usually sterile (70% of samples).48 The resident microflora of the vagina includes the same types of bacteria (Box 90-3).22,47,47 Aerobic and anaerobic organisms live in the vagina normally.273 Although the same types of organisms are found throughout the vagina, the closer to the cervix, the fewer organisms there are.297 Two or more bacterial species are usually recovered from vaginal cultures; however, 18% of vaginal cultures from healthy bitches contain only one organism, and repeated cultures from most dogs yield a pure culture on at least one occasion.47 Mycoplasmas can also be isolated from the vagina of clinically healthy bitches.47,95,95 Changes in the microflora occur with stages of the estrous cycle, but the change is primarily in the frequency of organism isolation rather than the type of organism found.47 One isolation of Simonsiella was reported from a bitch in estrus.393 Simonsiella is common in the oral cavities of dogs, and its transient presence in the vagina of this dog was attributed to licking. Few changes are associated with neutering.169,240,240 Staphylococcal species have been isolated more frequently from prepubertal and postpartum bitches than from postestrual bitches.47,297 The same organisms are found in the uterus during proestrus and estrus as are found in the vagina, with the exception that mycoplasmas were not found in the uterus.406 Treatment with either ampicillin or trimethoprim-sulfamethoxazole altered the normal microflora of the vagina in clinically healthy bitches.369 The normal microflora was suppressed in 2 of 5 ampicillin-treated dogs. In 3 ampicillin-treated dogs and in all dogs treated with trimethoprim-sulfamethoxazole, bacteria sensitive to the antimicrobial tended to be eradicated, whereas resistant bacteria remained or reappeared. Thus, the use of these antimicrobial agents to “sterilize” the vagina before mating is ineffective. Commensal bacteria are occasionally transferred between dog and bitch during mating.47,48 This transfer does not affect the fertility of either the male or the female. Aerobic bacteria are most commonly isolated from the vagina of healthy intact female cats (Box 90-4). E. coli, staphylococci, and streptococci are most common.172 Anaerobic bacteria are rarely isolated from the vagina.172 Pure growth of a single organism was common in normal cats and should not be considered indicative of disease when cytology is normal.172 Vaginal culture results from clinically healthy cats can be negative.172 The bacterial population of the vaginas of cats was not influenced by mating or administration of progestins.172 Relative numbers of vaginal organisms were greater in young (less than 1 year old) cats and pregnant cats.71 Although one study showed more profuse growth from cats in estrus,23 another study showed no effect of estrus on number of bacteria, but an effect was found on type of bacteria, with estrual cats having more bacteria that belonged to the family Pasteurellaceae.172 Although one study found bacteria in 2 of 29 uterine cultures, both from cats in estrus,71 a later study found no bacteria in the uterus of 66 adult female cats, 9 of which were in estrus.172 Aerobic bacteria are those most frequently found in the prepuce of intact male cats (Box 90-5) with Pasteurellaceae, E. coli, staphylococci, and streptococci being most commonly isolated.172 In contrast to female cats, anaerobic bacteria were isolated from 41% of male cats.172 Anaerobic species were Bacteroides spp., Fusobacterium spp., and anaerobic streptococci. The mean number of bacterial spp. isolated from the prepuce of male cats was 1.8 per cat, compared with 1.1 per cat in vaginal samples.172 Single-organism cultures from the prepuce were uncommon, and negative culture results were not found.172 Urinary tract infection (UTI) refers to microbial colonization of the urine or of any urinary tract organ, except the distal urethra, which has a normal bacterial flora. Infection of the urinary tract may affect more than one organ or may be localized to the upper tract (kidney and adjacent ureter; bacterial pyelonephritis) or to the lower tract (bladder [bacterial cystitis]; adjacent urethra [bacterial urethrocystitis]). Infections of the lower urinary tract in intact male dogs are considered to concomitantly affect the prostate gland (bacterial prostatitis). Infection of one part of the urinary tract increases the likelihood that the rest of the tract will become infected.278,279 Bacterial UTIs are common in dogs, especially in neutered female dogs, followed by castrated male dogs and intact female dogs.72 UTIs are least common in intact males.72 In a large study over a long period, 3.9% of female dogs and 2.9% of male dogs examined in one teaching hospital had positive urine culture results—although some dogs had their urine cultured only if findings of the urinalysis were abnormal, which would lower the infection rate because some dogs with UTIs documented by culture have normal urinalyses.239 Infection rate in 85 asymptomatic, adult, intact male dogs was 9%.49 Half of these dogs had the same organism isolated by direct aspiration of small prostatic cysts.49 UTIs are more common in older dogs than in young dogs, with a median age of 9 years in one study.304 More than 70% of UTIs in dogs are caused by a single bacterial species.239 In two large studies of acute-onset or local-practice UTIs, more than 90% of infections were due to a single bacterial pathogen.17,304 In complicated infections secondary to anatomic or functional abnormalities of the urinary tract, infection with multiple organisms becomes more likely. The most common gram-negative organisms are E. coli, Proteus, Klebsiella, Pseudomonas, and Enterobacter. E. coli is by far the most common urinary tract pathogen, causing 37% to 55% of UTIs.* In fact, most E. coli infections in dogs involve the urinary tract.298 Gram-positive organisms (Staphylococcus, Streptococcus, Enterococcus) account for 23% to 30% of naturally occurring UTIs.† Infection with Staphylococcus or Proteus is often associated with struvite calculi because of alkalinization of the urine by the organisms’ metabolism of urea. The most common eight species just listed account for 93% of all UTIs.239 Although mycoplasmas have been reported as causes of UTIs in dogs, their significance remains obscure because most of the reported cases were complicated by multiple disease processes.181,222 In the largest study of UTIs in dogs, 35 bacterial genera and four species of fungi were identified as causing UTIs.239 Occasionally, cases involving more unusual bacterial organisms are reported, such as Arcanobacterium (Actinomyces) pyogenes,54,239 Corynebacterium urealyticum,16,239,257,370 and Clostridium species.139,239 C. urealyticum infections are associated with preexisting micturition disorders, alkaline urine, struvite calculi or crystalluria, and bladder wall thickening and encrustation.16,257 Bacterial UTIs are less common in cats than in dogs. Numerous studies have shown that young adult cats having signs of lower urinary tract problems (dysuria with hematuria) rarely have bacterial UTIs.27,136,136 However, bacterial UTIs may develop secondary to urinary catheterization or urinary tract surgery, especially perineal urethrostomy.‡ UTIs unassociated with catheterization or perineal urethrostomy are more common in cats older than 10 years, especially female cats.15,31,136,244,245 The vast majority (more than 85%) of UTIs in cats are caused by a single organism.136,243–245 The organisms most frequently involved are the same as those in dogs,14,15,243–245,258 except that Staphylococcus felis was the most common staphylococcal species causing UTIs in cats.244,245 UTI due to Corynebacterium jeikeium has been reported in a cat that had a perineal urethrostomy.315 C. urealyticum UTI has also been reported in cats.16,67 Viruses and mycoplasmas have been considered as potential causes of lower urinary tract signs in cats. Investigators have been unable to find evidence of viral infections in clinical cases, and experimental viral infections have not induced clinical signs in cats.209,211 Mycoplasma felis and Mycoplasma gateae could not survive in osmotic conditions present in normal feline urine, although a Ureaplasma species could.59 However, ureaplasmas were not isolated from any cats with signs of lower urinary tract diseases.212 Yeast and fungi in urine can indicate contamination of the sample. However, the presence of fungi in properly collected (cystocentesis) and promptly examined urine samples is abnormal. In one large study, 0.4% of positive urine cultures from dogs contained fungal species.17 A positive culture result from urine collected by cystocentesis is needed to confirm the diagnosis of a fungal UTI. Fungal UTIs usually have been associated with abnormalities in host defenses, antibacterial use, and urogenital diseases.2,57,137,312,331 Diabetes mellitus, lower urinary tract diseases, neoplasia outside the urinary tract, and renal failure were the most common diseases identified in one study.182 Fungal UTI is commonly seen concurrently with bacterial UTI.182 The most common fungal organism causing UTI is Candida albicans (see Chapter 63).182 Systemic mycotic agents (e.g., Blastomyces [Chapter 57], Cryptococcus [Chapter 59], Aspergillus [Chapter 62]) may be found in urine from animals with systemic infections caused by these organisms and may cause UTIs.281 Urine sediment examination and/or culture were diagnostic of disseminated mycoses in 9 of 13 cases, whereas blood culture results were positive in only 1 of 8 cases.52 Cryptococcal UTI was identified in a cat with chronic renal failure but without any evidence of systemic cryptococcosis.68 Paracoccidioides brasiliensis was found in the urine of a cat with disseminated infection.142 Prototheca wickerhamii and Prototheca zopfii, saprophytic algae, have been found in urine sediment examination and on urine culture in dogs with systemic protothecosis (Chapter 67). In one survey, eight cases had urinalysis, with or without urine culture performed; six had positive findings for the organisms.311 The site of infection in these animals was the kidney. Protothecal infections are associated with immunosuppression of the host. UTIs are usually caused by bacterial organisms from the host’s own fecal or distal urogenital flora. Dogs with a UTI associated with E. coli or P. mirabilis were likely to carry the same organism in their intestinal tracts and prepuce or vagina.133,194,194 E. coli clones that cause UTI can be found frequently as intestinal colonizers in the same host.192 What triggers an organism to shift from asymptomatic colonizer of the intestine to causative agent of UTI is usually unknown. Also, external reservoirs from which the host acquires potential uropathogenic strains of bacteria is poorly understood. It is known that E. coli strains can be shared among humans and pets,195 although sharing of strains carrying urovirulence genes is not common.366 The usual method of infection of the bladder involves organisms ascending the urethra.357 Pyelonephritis is believed to be most commonly caused by ascending infection from bladder urine. Inflammation from cystitis can cause edema and deformation of the ureterovesicular junction, allowing bacteria to reach the ureters and then the kidneys.262 Renal infections also occur in the absence of evidence of cystitis. Uropathogenic E. coli (UPEC) have been shown to ascend from the bladder through the ureters to the kidneys where they can colonize the collecting ducts, distal and proximal tubules, glomeruli, Bowman’s capsule, and the blood vessel walls.223 The renal cortex is much more resistant to infection than the renal medulla, decreasing the likelihood of hematogenous infection.263,336 Pyelonephritis may be associated with renal abscess formation.358,427 Renal abscesses are rare but may result from hematogenous or contiguous spread of bacteria, from penetrating wounds, or from contamination associated with renal surgery or biopsy. Renal abscesses may be parenchymal or perirenal. The major host defense mechanisms against UTI are clearance of bacteria through complete voiding and the intrinsic antibacterial properties of the urinary epithelium.388 Development of UTI indicates an alteration in the host and bacterial flora relationship.301 To accomplish infection, bacteria must attach to and colonize the mucosa of the urethral orifice and transport themselves up the urethra, adhering to the uroepithelium. Both host defense mechanisms and bacterial virulence properties are important in determining whether infection occurs, as well as which part of the urinary tract is affected (Box 90-6). The inflammatory response in a UTI involves three steps: the bacteria stimulate uroepithelial cells to produce inflammatory mediators, these mediators direct inflammatory cells to the site of infection, and the local inflammatory response determines if the infection is eliminated or if tissue damage results. Thus, the host response is important in determining the degree of clinical signs and severity of tissue injury.372 Neutrophils that migrate from blood vessels through tissue and cross the epithelial cell layer to enter the urinary space result in pyuria. The genetic characteristics of a host organism have also been investigated in relation to susceptibility to UTIs and may be important in pathogenesis in some populations.130,336,336 For example, the vaginal epithelial cells of women with recurrent UTIs demonstrate more bacterial adherence in vitro than epithelial cells from women without UTIs.262,336 Important host factors in resistance to infection are normal, frequent emptying of the urinary bladder, presence of the resident urethral microflora, age and sex of the host, characteristics of urine, and normal urinary tract anatomy, including normal urinary tract epithelium with its glycoprotein coat, and immunologic responses.291,336 The importance of host factors is shown by the fact that many E. coli isolated from canine UTI have no detectable urovirulence factors.99 Female dogs and cats are more prone to UTI than their male counterparts, perhaps because of differences in urethral anatomy.15,367,373,385 Structural and functional abnormalities predispose to UTIs (Table 90-1).286,336 Lower urinary tract obstruction with secondary vesicoureteral reflux of infected urine is a contributing factor to the development of pyelonephritis, as are anatomic abnormalities such as ectopic ureters.290,338 Approximately 17% of dogs with ectopic ureters were found to have pyelonephritis.173 Other anatomic abnormalities associated with a chronic UTI include persistent urachus, other bladder diverticuli, perivulvar dermatitis, and a recessed vulva.233,247 Although vestibulovaginal stenosis was associated with UTI in one report,77 another study found no difference in vestibulovaginal ratios between healthy neutered dogs and neutered dogs with lower urinary tract diseases, 10 of 19 of which had UTIs.402 Functional abnormalities include instrumentation or catheterization or abnormal voiding, particularly with neurologic diseases such as spinal cord injury.249,295,295 TABLE 90-1 Terms Used to Categorize Urinary Tract Infections Metabolic diseases can predispose to UTI. Such diseases include diabetes mellitus, hyperadrenocorticism, primary hyperparathyroidism, hyperthyroidism, and renal failure. UTIs have been found in 29% of dogs with primary hyperparathyroidism,108 more than 40% of dogs with hyperadrenocorticism, and 20% to 40% of dogs with diabetes mellitus.117,176 In cats, 17% to 22% with chronic renal failure, 8% to 13% with diabetes mellitus, and 12% to 22% with hyperthyroidism were found to have UTIs.14,15,15 Treatment with certain classes of drugs predispose to UTI. Glucocorticoids are the most commonly used drugs that increase susceptibility to UTI.177 About 20% of dogs treated with glucocorticoids for skin diseases developed UTIs.385 Treatment with dexamethasone in association with surgery for acute thoracolumbar intervertebral disk herniation increased the risk for UTI 11-fold.231 In one experimental study, treatment with hydrocortisone did not result in UTIs in dogs treated for 49 days.116 In humans, antibacterial use up to 4 weeks before onset of UTI increased risk of UTI by three- to sixfold.262 Bacteria adhere poorly to healthy bladder epithelium because of the presence of a glycosaminoglycan coating. This coating, which can be replaced within 24 hours if injured, is extremely hydrophilic, so a layer of water forms at the surface. This aqueous layer provides a barrier between the transitional epithelium and the urine, explaining in part why bladder epithelium can tolerate constant exposure to a substance as irritating as urine. Infection is more likely to occur if this surface coating is damaged as by uroliths, neoplastic transformation, or exposure to chemical irritants such as cyclophosphamide. The kidney has no natural barrier against bacterial adherence.336 Bladder epithelial cells exfoliate in response to infection and are cleared with the flow of urine, an important defense mechanism. The bladder epithelium normally has a slow turnover rate of approximately 40 weeks in humans and mice.271 In humans with a UTI, large numbers of bladder epithelial cells exfoliate.271 Although this exfoliation is considered a host defense mechanism, it is also a way for bacteria to be spread into the environment and may also expose the underlying epithelial cells to infection. The antibacterial effects of urine include osmolality, urea concentration, and organic acid concentration.336 Markedly acidic (pH 5) or highly concentrated urine has an inhibitory effect on bacterial growth. The ability of cats to highly concentrate their urine may be one explanation for the low incidence of bacterial UTIs in young cats. However, results of one large study indicated that decreasing urine specific gravity was not correlated with UTI in cats, although increasing age, chronic renal failure, diabetes mellitus, and uncontrolled hyperthyroidism were associated.15 Urine that is less acidic and not well concentrated supports multiplication of urinary tract pathogens almost as well as nutrient broth.201 Specific serum and urine antibody responses accompany acute pyelonephritis in experimental models. These antibodies can be synthesized locally within the kidney and may enhance bacterial opsonization and ingestion by phagocytic cells; however, their importance is debated.336 The role of urinary immunoglobulins in preventing infection of the bladder is even more unclear.336 The urinary tract mucosa produces secretory IgA, which is thought to have a role against the entry of pathogens—probably by interfering with bacterial adherence, although absence of its production does not lead to increased UTI susceptibility.391 Evidence is lacking for a protective role for cell-mediated immunity in UTIs.336 It is clear from UTI research that minor weaknesses in host defenses necessitate more virulent organisms to induce disease. Normal host defenses clear some infections spontaneously, and some require minimal antimicrobial therapy. The more severe the host defense abnormality, the more prone the host is to infection, even with less virulent organisms, and the more prone to severe infections that require precise and extensive therapy.336 UPEC are a genetically heterogeneous group of E. coli that differ from nonpathogenic E. coli by the presence of virulence factor genes (see Chapter 35).271 UPEC typically carry large blocks of genes called pathogenicity-associated islands (PAIs), which are not found in fecal isolates.151 PAIs code for virulence factors such as hemolysins, adhesins, iron acquisition systems, fimbriae, and toxins.151 The presence of PAIs allows virulence genes to be easily spread among bacterial populations by horizontal gene transfer.291 Virulence factor genotypes of feline UPEC varied considerably with geographic location, for example, New Zealand versus Great Britain.128 Similar virulence factors were found in E. coli associated with canine UTI and pyometra.352 The virulence factors that were significantly more likely to be found in E. coli causing UTI or pyometra, compared with E. coli in feces from healthy animals, were the factors involved with hemolysin (hlyA), which lyses not only erythrocytes but also leukocytes, endothelial cells, and renal epithelial cells; iron acquisition (lucD); and a new protein, uropathogenic specific protein (usp).352 The type of virulence genes present in a certain strain appears to determine the site of infection (lower versus upper tract) and the severity of the infection.291 One genetic type of UPEC was found to change virulence properties depending on host response during infection.271 Results of genetic studies continue to determine whether E. coli isolates that cause cystitis are distinct from those that cause pyelonephritis or whether the host response determines the way the genes operate.151,223 E. coli from UTIs in dogs has been found to have varying propensities to cause pyelonephritis and renal damage in mice based on urovirulence factors.423 Even though bacterial virulence factors are important, the severity of the tissue injury also depends on the inflammatory reaction of the host. The most studied adhesin and the first virulence factor identified for UPEC was P fimbria.223 P fimbriae are encoded by the pap (pyelonephritis-associated pili) gene cluster and are more prevalent among strains of UPEC associated with pyelonephritis, although they do not appear to be essential for UPEC to cause pyelonephritis.223 The pap gene cluster consists of 11 genes, one of which, papG, encodes the P-fimbrial adhesion.223 The class III papG allele is associated with UPEC causing genitourinary tract infections in dogs and cats.223 Although P fimbriae are important, UPEC have other types of fimbriae, providing the organism with multiple alternatives for adherence during UTI.223 The bacterial mechanisms for adherence and infection are complex and not that well studied in dogs and cats. UPEC are usually thought of as extracellular pathogens because they are cultured from the urine. Observations have found that these organisms are not always extracellular.340 Piliated type 1 E. coli are able to enter bladder epithelial cells. Usually, this triggers the epithelial cell to undergo apoptosis and exfoliate. However, some E. coli seem to be able to persist intracellularly in some hosts by moving to other superficial cells or to deeper epithelial cells.271,340 Thus, infection can persist even though bladder urine is sterilized by antimicrobial therapy. FimH, the adhesin for type 1 fimbriae that can trigger the uptake of E. coli into murine bladder cells, has been found in UPEC from cats.128 Many recurrent infections are relapses with the same bacterial strains. The ability of E. coli to persist intracellularly is a possible explanation for some cases of relapsing UTIs.340 Some E. coli are antimicrobial resistant. Interestingly, quinolone-resistant E. coli from canine UTI were found to have fewer virulence genes and to be less likely to be in phylogenetic group B2, normally associated with urogenital pathogenicity.193 Most of these quinolone-resistant E. coli were fecal E. coli, not typical of UPEC. They also carried non-canine-associated virulence factors. Several possible explanations were given. One is that dogs with resistant E. coli UTI were immune compromised so that fewer pathogenic organisms could cause infection, thereby making exposure to quinolones more likely. Such a situation has been described in humans. Another explanation is that the organisms originated from a noncanine source. A chicken-source quinolone-resistant E. coli has a phylogenetic group distribution and virulence gene profile similar to those of quinolone-resistant E. coli from humans.193 UTIs in dogs and cats are often clinically silent (the owners report no signs of illness in their pets).235 In one survey of asymptomatic cats, 29% had UTIs.245 Most of these cats were older (median age 14 years) females (92%) and were examined for a variety of medical problems or for routine geriatric or preanesthetic screening.245 None showed signs of lower urinary tract disease or had a history of UTI.245 Two organisms were responsible for 95% of these infections, Enterococcus faecalis (50%) and E. coli (45%).245 These UTIs were associated with higher erythrocyte counts and leukocyte counts than urine specimens from noninfected cats, indicating inflammation in response to infection.245 The E. coli most commonly involved (82%) was of phylogenetic group B2, which is a virulent extraintestinal pathogenic E. coli, suggesting that these asymptomatic UTIs are not benign colonization by commensal organisms.245 Of dogs with diabetes mellitus or hyperadrenocorticism and a UTI, 95% had no UTI symptoms as described by their owners117; similarly, no dogs being treated with glucocorticoids for pruritis that developed UTIs had symptoms.385 Asymptomatic UTIs are also common in dogs with spinal cord injury.249 UTIs in cats with diabetes mellitus, hyperthyroidism, and chronic renal failure are also often asymptomatic.14,258 Many UTIs arising as a result of urinary tract manipulation are asymptomatic. Asymptomatic infections also occur in dogs and cats without such predisposing conditions. It is unknown whether this is due to the infecting bacterium, the host response, or a combination of the two. One idea in humans is that affected individuals are genetically different from those who develop symptomatic infections in regard to their host response.372 In one study in children, E. coli caused the majority of symptomatic, catheter-related infections, but the same E. coli clones were associated with both symptomatic and asymptomatic infections, suggesting that host response to the infection was more important.341 In a woman whose voided urine samples were cultured biweekly for 16 weeks with a single sample 1 year later, the same E. coli with a high virulence factor score was isolated on 8 occasions, but she had symptoms of acute cystitis only once and responded to a 3-day course of antimicrobial therapy.274 The use of self-collected voided samples makes it impossible to know if these E. coli were in the bladder only once when the clinical signs were present. The use of voided samples for bacterial culture in human medicine makes it difficult to compare results of studies of asymptomatic bacteriuria in humans with the situation in dogs and cats where cystocentesis samples are most common. Also, dogs and cats cannot report symptoms. Because of the lack of historical and physical signs, asymptomatic infections are difficult to localize to the upper or lower urinary tract. In one study, 6 of 12 clinically asymptomatic female dogs with UTIs had infection localized to one or both kidneys, whereas 6 had bladder infections.238 Despite the absence of clinical signs, 3 of the dogs with renal infection and 3 of the dogs with bladder infection had mild to moderate inflammation in the infected organ. Animals with few historical signs have had severe tissue injury, such as renal or prostatic abscess formation. Unfortunately, there is no way to differentiate asymptomatic bacteriuria that is benign from that which may lead to urinary tissue injury. It is hoped that the application of polymerase chain reaction–based tests to detect E. coli with known virulence factors, the ability to quantify the host response by measurement of urine chemokines, and the detection of genetic defects in immunity may help determine which cases of asymptomatic bacteriuria require therapy.141 A relapse is a UTI due to the same organism that recurs after therapy is discontinued (see Table 90-1). A reinfection is defined as a UTI caused by a different organism each time it recurs, at variable intervals after therapy is discontinued. Although most relapsing UTIs recur quickly, some do not relapse for months.129 When recurrence of UTI with the same organism does not occur for months, it is difficult to distinguish a relapsing infection from a reinfection due to the same species of organism. E. coli is the most common organism to cause recurrent UTI in dogs.17 Clinicians have relied on the antimicrobial susceptibility pattern of the organism to help determine whether the current infection is due to a new or the same E. coli. However, the same E. coli can shift in regard to antibacterial susceptibility, so this method is not very accurate.99,126,129,150 Unfortunately, more accurate methods, such as pulsed-field gel electrophoresis and virulence factor genotyping, are not readily available.
Genitourinary Infections
Resident Microflora
Dogs
Cats
Urinary Tract Infections
Etiology
Bacterial Infections
Dogs
Cats
Fungal Infections
Algal Infections
Pathogenesis
Host Factors
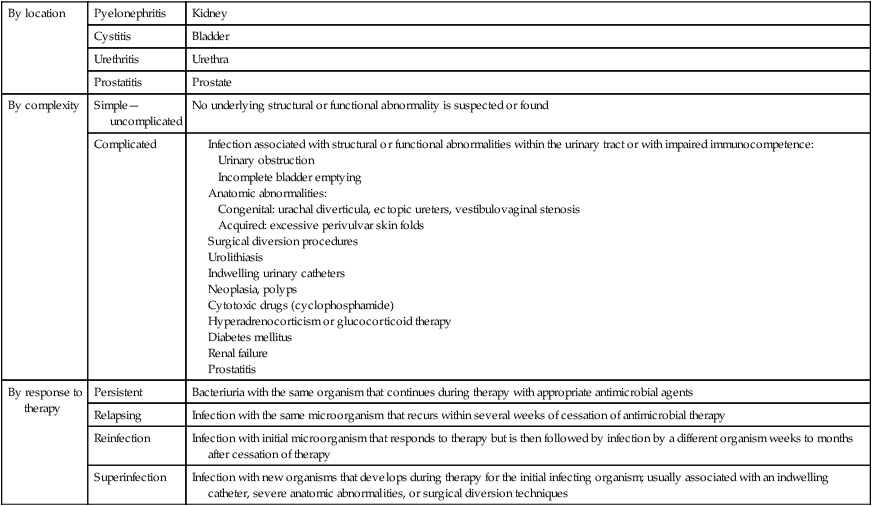
By location
Pyelonephritis
Kidney
Cystitis
Bladder
Urethritis
Urethra
Prostatitis
Prostate
By complexity
Simple—uncomplicated
No underlying structural or functional abnormality is suspected or found
Complicated
By response to therapy
Persistent
Bacteriuria with the same organism that continues during therapy with appropriate antimicrobial agents
Relapsing
Infection with the same microorganism that recurs within several weeks of cessation of antimicrobial therapy
Reinfection
Infection with initial microorganism that responds to therapy but is then followed by infection by a different organism weeks to months after cessation of therapy
Superinfection
Infection with new organisms that develops during therapy for the initial infecting organism; usually associated with an indwelling catheter, severe anatomic abnormalities, or surgical diversion techniques
Bacterial Virulence Factors
Asymptomatic Bacteriuria
Recurrent Infections: Relapse Versus Reinfection
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Genitourinary Infections
