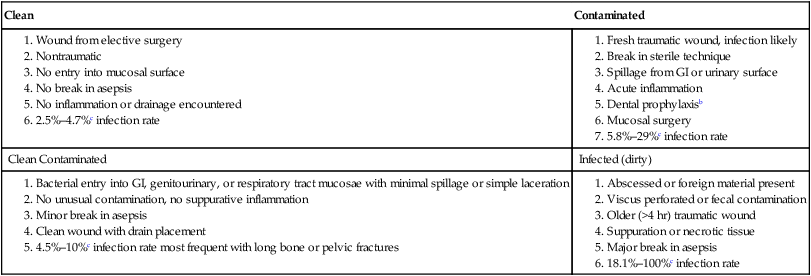
Surgical site infections (SSIs), which hinder successful healing of operative wounds, are recognized as a relatively uncommon but inherent risk of every surgical procedure.51 Although every surgical wound becomes contaminated with bacteria, only a few become infected. The use of aseptic methods and minimization of tissue trauma were major breakthroughs in reducing postoperative infections. Subsequent development and use of antibacterials in association with surgery further reduced numbers of SSIs. However, SSIs will continue to be an inherent risk, and the risks will likely increase over time as a result of more invasive and prolonged surgical procedures, wider use of synthetic implants, and continued emergence of and dissemination of multidrug-resistant bacteria. When the physical barrier of the skin is compromised, as from surgical incisions, the resulting wound must progress through the predictable stages of wound healing. As mentioned, bacterial contamination of the wound bed occurs with every surgical procedure, but most surgical wounds do not develop an infection. The success of wound healing is influenced by the overall health of the patient, the surgical procedure and type of wound created, and the type and number of contaminating organisms introduced into the wound. In a prospective study of postoperative surgical site infections in dogs and cats, the risk of infection was statistically associated with greater duration of surgery, increasing number of operating room participants, and decreased cleanliness of the surgical site.19 These and other factors regarding postoperative surgical site infections are reviewed next. The major source of bacteria that contaminate surgical wounds is the patient’s endogenous microflora. Surgical incisions can also be infected from the hands of veterinary personnel or owners and the environment, but these are typically of lesser concern. Infections with methicillin-resistant staphylococcal organisms have been of some concern because of their zoonotic implications (see Chapters 34 and 99).61a Skin-associated bacteria can be reduced but not eliminated by antisepsis. Bacteria residing in the deeper parts of the skin such as the hair follicles and sebaceous glands are not removed or killed by preparative scrubbing, and they may enter deeper tissues during the initial incision. Development of SSIs, however, is not a simple matter of bacterial contamination. Whether or not an infection develops involves the interaction of bacterial (organism, virulence, dose, antimicrobial resistance), patient (immune status, comorbidities), and procedure (tissue injury, foreign materials) factors. In humans, the National Research Council (NRC) has established a surgical wound classification system that is summarized in Web Table 53-1 and in Web Box 53-1. This system has been used in veterinary medicine, although it usefulness in veterinary patients has been questioned.10 In a study of 1574 dogs and cats with clean, clean contaminated, contaminated, or dirty surgical wounds, infection rates were 4.7%, 5%, 12%, and 10%, respectively.10 Anaerobic bacteria should always be assumed to be a component of mixed surgical infections,17 or numerous therapeutic failures could result. WEB TABLE 53-1 Classification of Surgical Wounds and Indications for Prophylaxisa 1. Bacterial entry into GI, genitourinary, or respiratory tract mucosae with minimal spillage or simple laceration 2. No unusual contamination, no suppurative inflammation 4. Clean wound with drain placement 5. 4.5%–10%c infection rate most frequent with long bone or pelvic fractures GI, Gastrointestinal. aModified from National Academy of Sciences/National Research Council. 1964. Postoperative wound infections: the influence of ultraviolet irradiation of the operating room and of various other factors. Ann Surg 160(Suppl):1-132. bFor dental prophylaxis information, see Gingivitis and Periodontitis, Chapter 88. cPrevalence of wound infections in dogs and cats from veterinary teaching hospitals.10,30,30 The process of wound healing should be viewed as a complex interaction involving the patient, the local wound environment, and the contaminating pathogen. Each facet of this interaction has many associated factors, the combinations of which are unique to each situation. A thorough assessment of these factors and the common sources of perioperative contamination (Box 53-1) should be considered when preparing for each surgical procedure so that the most appropriate steps can be taken to minimize the risk for the development of postoperative infection (Box 53-2). However, there have been few proper risk factor investigations regarding SSIs in small animals, and most current practices are based on extrapolation from human medicine along with subjective determination of “best practices.” Preoperative preparation of the surgical site is a critical factor in preventing wound infection (see Chapter 93). Skin trauma produced during surgical preparation greatly increases the local bacterial population. Preoperative clipping time is an important factor in the development of postoperative wound infections.10 Animals with surgical sites that were clipped before anesthesia induction rather than immediately before surgery were three times more likely to develop surgical wound infections. Animals clipped hours or days before the surgery because ultrasonographic studies were performed had a postoperative infection rate three times greater.10 This presumably relates to mild skin trauma or abrasion that predisposes to proliferation of bacteria and inhibition of the efficacy of surgical skin preparation. Animals with endocrinopathies such as hypothyroidism or hyperadrenocorticism are much more likely to develop postoperative wound infections.46 Intact males were also found to have a higher risk of wound infection, which parallels findings in people and rodents and is presumably a result of the inhibitory effect of testosterone on some inflammatory cytokines.59 Many additional risk factors have been identified in humans, and some could also apply to veterinary patients, such as diabetes mellitus, obesity, malnutrition, immunosuppressive therapy, and colonization with specific pathogens such as methicillin-resistant Staphylococcus aureus.4,38 Use of proper surgical technique is perhaps the single most important factor in preventing postoperative infections. The risk of tissue infection is directly proportional to the increased amount of tissue handling and trauma. Vascular compromise to tissue, excessive electrocautery, and bleeding into tissue spaces are the major contributory factors. Foreign material and blood clots allow for adherence and replication of microorganisms and facilitate formation of biofilms. Experimentally, use of fibrinolytic agents prevents infections, abscesses, and adhesions after surgery. Bacteria that invade surgical sites or implants can remain dormant for months to years, and although less common, the sites can be entered during the healing and recovery phases. In some animals, occult orthopedic infections develop. The bacteria remain at the site of the healed fracture but do not cause clinical or radiographic evidence of osteomyelitis.16 The infection may persist locally and be refractory to treatment until the orthopedic implants are removed. Surgical wounds of pets may be contaminated with the human commensal S. aureus, from contact with veterinary personnel or owners, which may lead to infections that are resistant to treatment if methicillin-resistant strains are involved (see Chapter 34).42,49,49 Orthopedic implants have greatly improved treatment of bone fractures and noninfectious arthritis, but they are associated with an increased risk for orthopedic device–related infection.20b,75 Similar risks have been found for cardiovascular implants in dogs, where Pseudomonas aeruginosa and Staphylococcus spp. were most commonly isolated.20 Vascular implants have a high risk of infection in dogs, which can be partially controlled by the use of antimicrobial-impregnated materials.58 Immediately after implantation, all synthetic materials undergo a race in colonization of their surface by tissue and bacterial cells in the local area. In addition to body fluids containing serum proteins (albumin) and platelets, bacteria such as staphylococci have adhesins that attach bacteria to the biomaterial. Adherence leads to colonization of the foreign body surface, which can result in overt infection or bacteremia. Under these conditions, bacteria become sessile and develop antimicrobial resistance in this quiescent phase. Standard antimicrobial therapy at this time may eliminate the clinical illness, but the bacteria may persist in the biofilm. Various organisms such as coagulase-negative staphylococci and P. aeruginosa are able to produce a pathogenic biofilm composed of polysaccharide glycocalyx (slime). With strict anaerobic conditions or with molecular identification techniques, anaerobes such as Propionibacterium species are often recognized.65 They form an additional layer on the surface of prosthetic implants that can originate during the surgical procedure.3 The glycocalyx slime promotes intercellular adhesion, captures nutrients, and protects microorganisms from antibacterial therapy. The use and timing of prophylactic antimicrobial therapy affects infection rates in animals with clean surgical wounds. Guidelines in human surgery have been established to justify their use and ensure maximal effects with minimal consequences; however, implementation of standardized protocols has been inconsistent in veterinary practice.71 In a study at a teaching hospital, 72.5% of 1100 animals with clean surgical wounds received perioperative antibacterials, which were associated with a lower infection rate.68 However, in another comparable study in which 41% of 1146 animals with clean surgical wounds received antibacterials at varying times, the infection rate varied according to the timing of the antibacterial administration.10 Animals with clean wounds receiving perioperative antibacterials, no antibacterials, or postoperative antibacterials had infection rates of 2.2%, 4.4%, and 8.2%, respectively. In another study at a teaching hospital, dogs undergoing elective orthopedic surgery were divided into three groups and given either no antimicrobials, penicillin G, or cefazolin 30 minutes before surgery, and again if the surgery lasted longer than 90 minutes.74 Dogs in both antibacterial treatment groups had lower infection rates; therefore the control group was abandoned. Results of these studies emphasize the importance of having maximal antibacterial activity at the time of the surgical procedure. (See Tables 53-1 and 53-2 and the Drug Formulary in the Appendix for a list of dosages.) TABLE 53-1 Indications and Drugs for Antimicrobial Prophylaxis or Treatment in Surgery
Surgical and Traumatic Wound Infections
Etiology
Clean
Contaminated
Clean Contaminated
Infected (dirty)
Surgical Class
Examples
Associated Bacteria
Recommended Therapy
First Choice
Alternatives
PROPHYLAXIS
Cleana
Routine surgery
None
None
None
Clean contaminated
Genital surgery
Aerobes: gram-negative
Anaerobes
Cefazolinb
Fluoroquinolone
Prolonged (>3 hr) surgery, orthopedic prosthesis, amputation, open fracture reduction
Escherichia coli, staphylococci, streptococci
Cefazolinb
β-Lactamase-resistant penicillin
Intra-abdominal
Aerobes: gram-negative
Anaerobes
Cefoxitinc
Gentamicin, metronidazole
Dentistry
Aerobes: gram-positives and anaerobes
Cefazolinb
Ampicillin, amoxicillin, chloramphenicol
Contaminated
Bite wounds
Aerobes and anaerobes
Ampicillin or amoxicillin-clavulanate
Clindamycin
Enterotomy with leakage, abdominal trauma
Aerobes: streptococci, enterococci
Anaerobes: bifidobacteria, clostridia, fusobacteria, Bacteroides
Cefoxitinc or, for enterococci, use ampicillin or amoxicillin
Aminoglycoside, metronidazole
Biliary infection cholecystectomy
Enterobacteriaceae (E. coli, Klebsiella, Proteus), Bacteroides, Clostridium
Cefoxitinc, cefotaximed
Gentamicin
Colonic resectione
E. coli, Bacteroides
Neomycin and metronidazole preanesthesia, and enemas
Cefoxitin, gentamicin, clindamycin
TREATMENT
Infected
Abscesses
Aerobes
Ampicillin or amoxicillin-clavulanate
Aminoglycoside, clindamycin
Ruptured bowel, colonic leakage
Anaerobes
Cefotaximed
Metronidazole
Pyometra
Aerobic and anaerobes
Cefazolinb
Fluoroquinolone ![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Surgical and Traumatic Wound Infections
