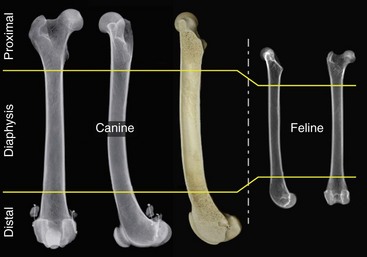
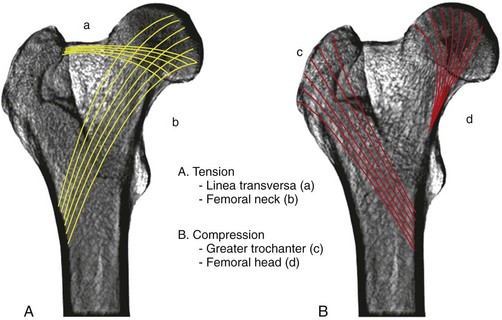
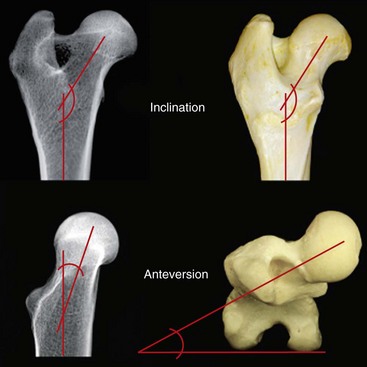
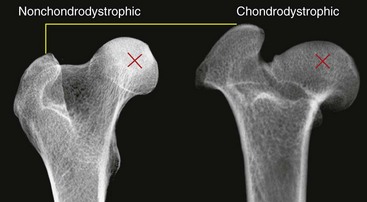
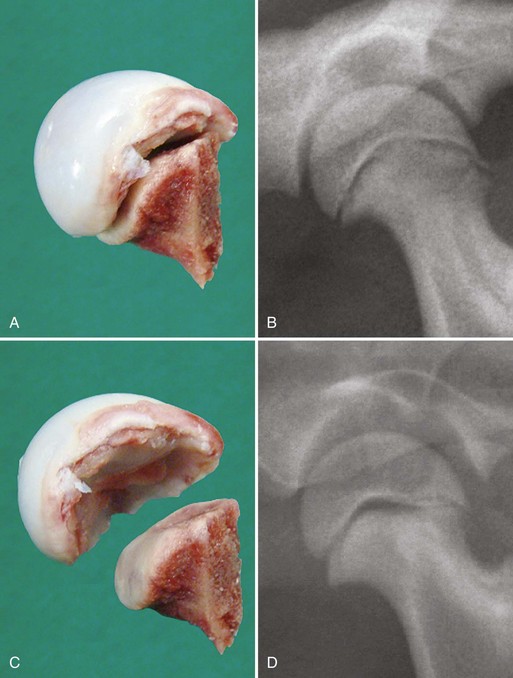
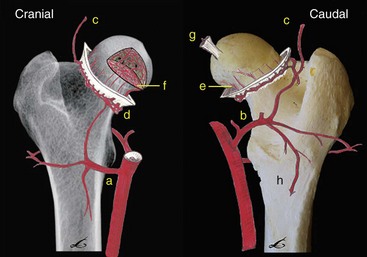
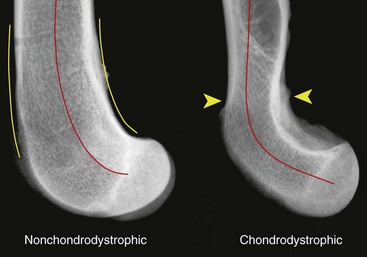
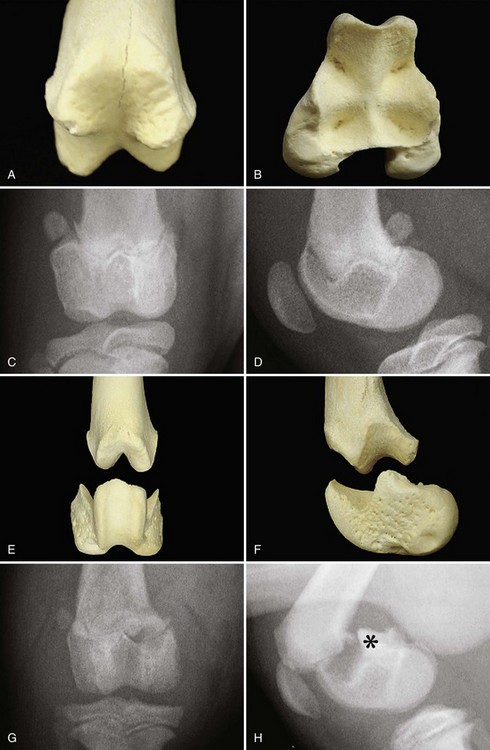
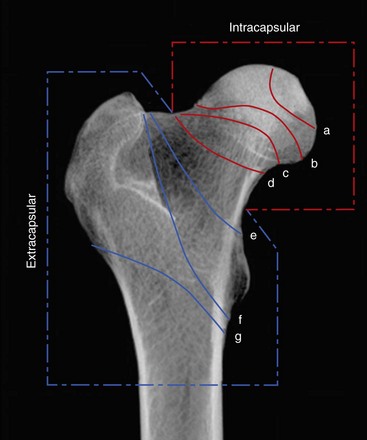
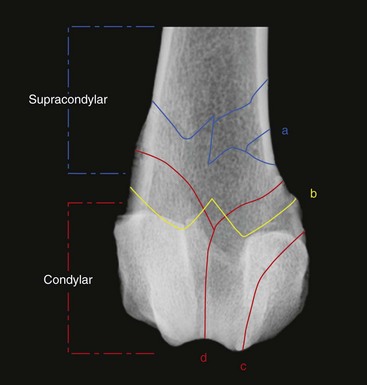
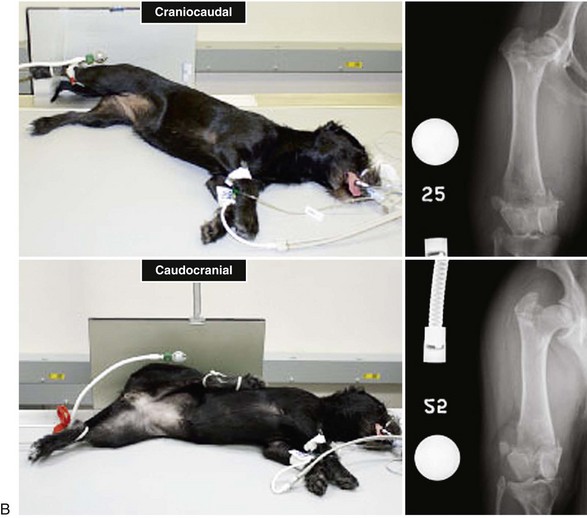
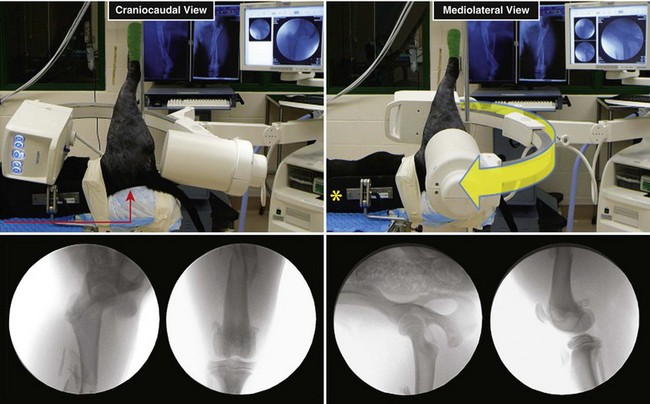
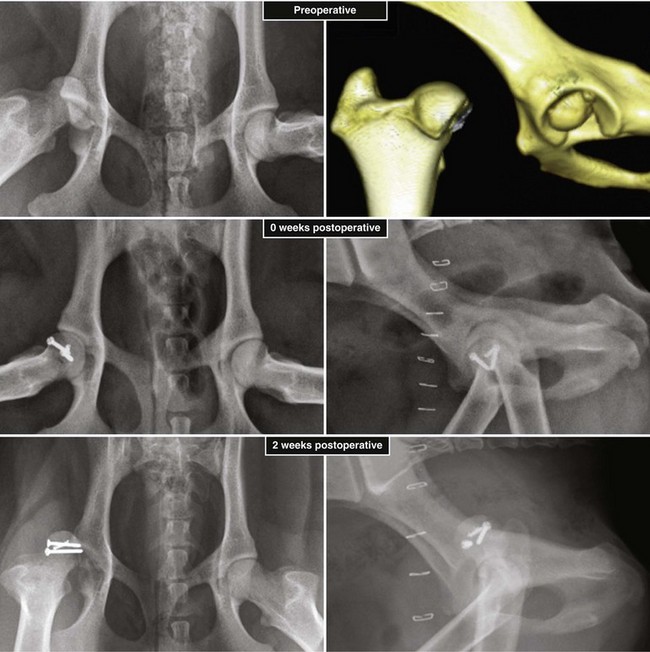
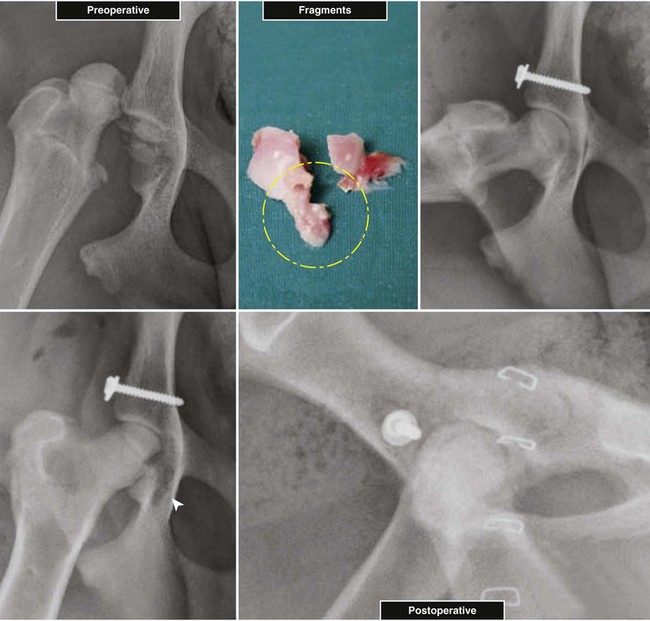
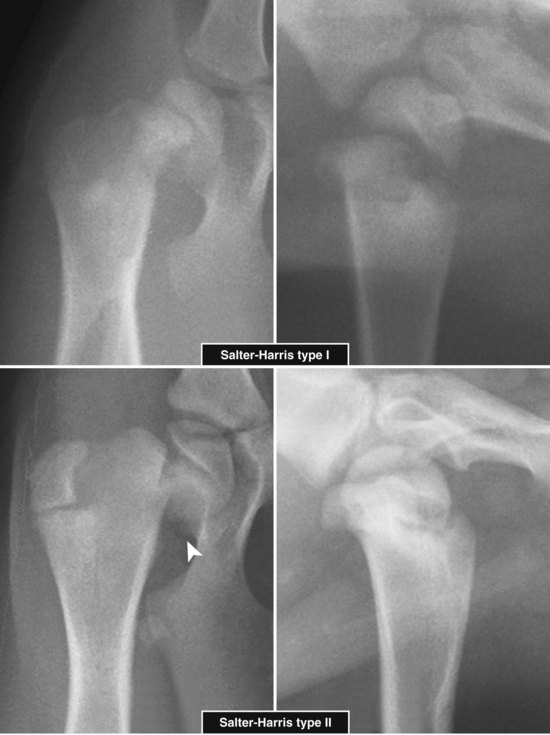
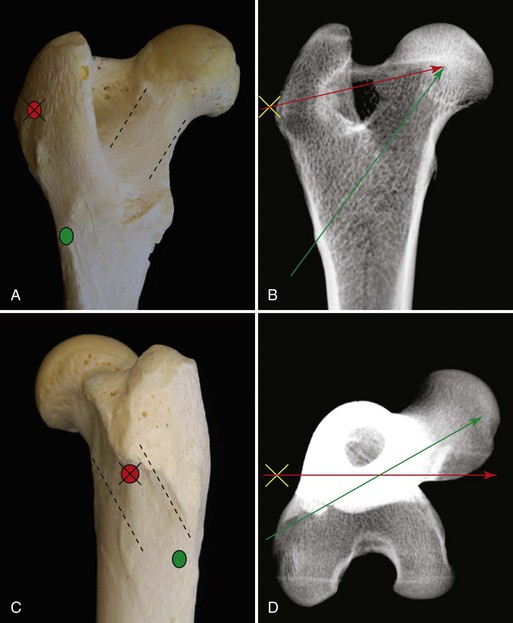
Chapter 61 Femoral fractures constitute approximately 20% to 25% of all fractures encountered in the dog and cat, and represent 45% of all long-bone fractures.178,219 Young animals are significantly overrepresented, with 86% of animals younger than 5 years of age and 48% younger than 1 year.31 Proximal and distal physeal fractures most commonly affect immature animals, whereas diaphyseal and metaphyseal fractures generally involve skeletally mature animals.21,31,219 These fractures are often the result of substantial trauma, most often secondary to vehicular accidents; thus careful evaluation of the animal for concurrent injury is essential. Despite their association with trauma, 83% of femoral fractures are closed,31 likely because of the protective effects of the large thigh musculature. Conservative treatment of femoral fractures is consistently ineffective and should be abolished in favor of internal fixation, regardless of fracture location or pattern (Figure 61-1).33,178,198 As the most commonly fractured long bone, it is not surprising that the femur was the first bone in which internal fixation was attempted.37,71 Although early reports of fixation described the use of a single intramedullary pin, the inability of such implants to effectively counteract all forces at the fracture gap became readily apparent, and additional fixation such as cerclage wires was often advocated. In the then nascent field of veterinary orthopedics, intramedullary pinning was the most frequently taught technique because of the lack of more suitable methods of fixation, including bone plating. The relative simplicity and low cost of intramedullary pinning also contributed to its popularity.36 Unfortunately, this fairly simple method of fixation was associated with an unacceptable incidence of complications, possibly caused by the combined effects of a limited understanding of fracture and implant biomechanics, the use of relatively extensive open approaches, and economic constraints. When the shortcomings of bone pinning were recognized in the early 70s, bone plating of the femur, although it had been available since the early 60s, started to gain acceptance.103 Over time, refinements in bone plating techniques greatly improved the success rate of femoral fracture repair. Since these early reports, and particularly over the past two decades, tremendous advancements in implant application and design have resulted in faster bone healing and a better prognosis. In part thanks to such forward thinking surgeons as Siegfried Weller, Jeffrey Mast, Roland Jakob, Reinhold Ganz, and many others, a paradigm shift has occurred in human and veterinary orthopedics.146,225 Critical evaluation of clinical outcomes and a better understanding of fracture mechanics and biology have incited surgeons to move gradually from a mechanistic approach that underscores absolute rigid fixation, to flexible fixation and less invasive surgical techniques.177 The net result has been the nurturing of a biomechanical environment more conducive to bone healing that has translated to improved surgical outcomes. This concept, which is commonly known as biological osteosynthesis, stresses the importance of reducing iatrogenic trauma to the fracture site through less precise fracture reconstruction (except for articular fractures) and less rigid fixation. Its effect is optimization of biologic potential, which encourages early callus formation with rapid secondary bone healing.91,127 In parallel, implant evolution has included improvements in plate and interlocking nail technology to provide greater strength, as well as better preservation of blood supply. These developments mainly include the use of angle stable mechanisms at the plate-screw or nail-bolt interfaces. Historically, the prognosis for femoral fracture has been reported to be guarded, with variation dependent upon fracture severity, articular involvement, soft tissue trauma, and concurrent injury. In fact, femoral diaphyseal fractures have been reported to be the most common fracture affected by osteomyelitis and nonunion, despite the fact that most fractures are closed.45,46,113,201 It is understood that because the femur is the most commonly fractured long bone, and because internal stabilization is a quasi-absolute necessity, the risk of complications is inherently increased. It is the authors’ belief, however, that underestimation of mechanical challenges, overaggressive approaches, and the utilization of inappropriate fixation methods are more likely to blame for the incidence of complications and the guarded prognosis reported in the literature. The inadequacies of previously used techniques should encourage movement toward biological osteosynthesis and newer implants. It is hoped that these changes, in combination with the advancement of veterinary surgical specialization, will lead to fewer complications and better prognoses. In subsequent sections of this chapter, relevant surgical anatomy, including species- and breed-specific considerations, fracture classification, surgical planning as in selecting an implant and choosing a surgical approach, and treatment options for specific fractures by region will be described. The femur is composed of three separate regions (Figure 61-2)74: (1) the proximal femur includes the head, neck, trochanters, and trochanteric fossa; (2) the diaphysis is the elongated, cylindrical region of cortical bone, delineated by the proximal and distal metaphyses; and (3) the distal femur includes the distal metaphysis, or supracondylar region, trochlea, condyles, and intercondylar fossa. Comprehensive knowledge of the anatomy of the femur is a prerequisite for successful fracture repair. Anatomy of the Femoral Head and Neck The femoral head is a nearly hemispherical projection that articulates with the acetabulum to form the hip joint.74 It is covered with hyaline cartilage, except over the fovea capitis, which is the insertion point of the ligament of the femoral head. The femoral neck supports the head and shifts the diaphysis laterally, away from the body wall. Although this provides the hip joint with a greater range of motion, it generates large bending stresses on these structures during daily activity.7,60,161,170 The trabecular network of the proximal femur is naturally oriented to withstand these forces (Figure 61-3) and is reinforced cranially by the linea transversa, an osseous ridge that extends from the base of the femoral head to the greater trochanter.74 These two structures combined help to resist bending moments within the proximal femur, and disruption of their structural integrity creates a challenging mechanical environment for fracture stabilization. The head and the proximal portion of the neck are within the coxofemoral joint capsule, which attaches a few millimeters from the acetabular lip and near the base of the neck.54,74 The anatomic relationship between the femoral head and the diaphysis is characterized by the angles of inclination and anteversion (Figure 61-4).161 Inclination is defined as the angle between the femoral neck and the diaphysis in the frontal plane; several radiographic methods used for its measurement have been described.100,102,154,191,217 In dogs, dependent upon the breed and the method of measurement, the reported angle of inclination ranges from 130 to 145 degrees.100,154,191 Anteversion, which is defined as the angle created by the position of the femoral head with respect to the diaphysis in the transverse plane, may be correlated with the degree of femoral torsion.16,154,161 Reported angles of anteversion range from 27 to 32 degrees in the dog and are also dependent upon the breed and method of measurement.16,154,164 An understanding of these angles is important, as they can influence fracture configuration, the method of stabilization, and prognosis. Their alteration during fracture repair may affect the stability and biomechanics of the hip joint,161 subsequently increasing the postoperative risk for luxation and/or osteoarthritis. The proximal femur embodies three protuberances, which serve as insertion points for the major muscles acting on the hip joint. The greater trochanter is the largest of the three and is located on the lateral surface of the femur. The middle and deep gluteal muscles, as well as the piriformis muscle, attach to this apophysis.74 In dogs, the size and position of the greater trochanter with respect to the femoral head and neck are breed dependent. Typically, the proximal aspect of the greater trochanter lies at the level of the femoral head; however, in chondrodystrophic dogs, it is more prominent and extends farther proximally (Figure 61-5). The lesser trochanter is distal and caudomedial to the femoral neck. It is the insertion site for the iliopsoas muscle and represents the distal limit of the proximal metaphysis.74 The third, and smallest, trochanter is located distal to the greater trochanter on the caudolateral surface of the femur. The third trochanter serves as the insertion site for the superficial gluteal muscle.74 Finally, the trochanteric fossa, which is the large depression caudal to the linea transversa, is the insertion point of the internal and external obturator muscles and the gemelli muscle.74 The floor of the trochanteric fossa is centered over the medullary canal of the femur and is used as the proximal landmark for the insertion of intramedullary implants. Proximal femoral growth initially occurs from a single physis until approximately 2 to 3 months of age, when, as a result of muscular pull, the proximal femur divides into the capital and trochanteric physes.120,187 The capital physis is solely responsible for the formation of the femoral neck and accounts for approximately 25% of the longitudinal growth of the femur.88,112,187,198 The capital physis is described as having an L-shaped profile in the transverse plane, which provides intrinsic resistance to shear and rotational forces during development (Figure 61-6).198 Similarly, in the event of a fracture, this profile helps guide anatomic reduction and provides some intrinsic stability during repair. The physis of the greater trochanter does not significantly contribute to the overall length of the femur. Rather, its importance lies in its shaping of the proximal femur and shifting the attached muscles laterally.100,112,187,198 Although this provides a mechanical advantage to the local musculature by increasing the lever arm of each muscle, it also generates large distraction forces following fracture. Closure of these physes is species and breed dependent. It typically begins at 6 months of age in dogs and is complete by 9 to 12 months.29,47,187,211 In cats, closure occurs between 7 and 10 months.202 The blood supply to the proximal femur is a complex arterial network that has been thoroughly studied.19,54,78,122–125,188 This network is subdivided into (1) extraosseous, (2) intracapsular, and (3) intraosseous vessels.125 Because all arteries of the intracapsular and intraosseous networks propagate from the extraosseous vessels via a single extracapsular vascular ring, the blood supply to the femoral neck and head is highly susceptible to vascular insult. Extraosseous vessels include, from the most to the least significant, the lateral and medial circumflex femoral, caudal and cranial gluteal, and iliolumbar arteries (Figure 61-7).124 The lateral and medial circumflex femoral and caudal gluteal arteries coalesce to form an extracapsular vascular ring that lies at the base of the femoral neck.124 The intracapsular arteries develop from this ring, penetrate the joint capsule at its distal attachment, and subsequently ascend toward the epiphysis. These arteries remain subsynovial as they rise and lie along the craniodorsal aspect of the femoral neck.125 Near the capital physis they anastomose to form an intracapsular vascular ring, encircling the neck. Branches of this ring then penetrate the physis and give rise to an intraosseous, arcuate network that supplies the epiphysis and proximal neck (see Figure 61-7).112,125 The artery of the ligament of the femoral head does not contribute to the epiphyseal blood supply in dogs.19,78,125 This is in contrast to cats, which may explain why fewer cases of avascular necrosis of the femoral head and neck are seen in this species.53 Last, branches of the caudal gluteal and medial circumflex femoral arteries penetrate the floor of the trochanteric fossa and create an intraosseous network that supplies the base of the femoral neck and greater trochanter. Disruption of this complex vascular network, particularly in immature animals, by the inciting trauma or by surgical insult may account for complications such as (1) abnormal development of the femoral head and neck, (2) femoral head and neck resorption, and (3) degenerative joint disease.12,54,55,111,112 In addition, it has been suggested that damage to the vessels within the trochanteric fossa during intramedullary pinning may alter the development of the proximal femur in immature animals.28 Anatomy of the Femoral Diaphysis The femoral diaphysis is a cylindrical structure delineated by the cancellous bone of the proximal and distal metaphyses. In dogs, the distal third of the diaphysis curves caudally, whereas in cats, the diaphysis is straight (see Figure 61-2).178 The medullary cavity follows the curvature of the diaphysis, with its narrowest diameter within the proximal third of the femur. The degree of curvature in dogs increases with size and to some extent varies with each animal.178 This curvature may influence the method of stabilization used for diaphyseal fracture and potentially may even affect surgical outcome. Most of the femoral diaphysis lacks muscular attachment, with the exception of its most proximal and caudal surfaces. Proximally, the subtrochanteric region is the origin of the vastus lateralis, intermedius, and medialis muscles, as well as the adductor longus muscle.73,74 The caudal surface of the femur is finely roughened by the insertion of the adductor magnus et brevis muscle along the narrow facies aspera (linea aspera), which spans the entire length of the caudolateral diaphysis.74 The pectineus and semimembranosus muscles insert on the distal third of the caudomedial diaphysis, with their attachments extending distally onto the medial condyle.74 In the event of a fracture, the arrangement of these muscles along the femoral diaphysis commonly results in caudoproximal displacement of the distal fracture segment. Embryogenic development of the femur begins at a primary diaphyseal center of ossification and is followed by growth from secondary centers of ossification at the proximal and distal femoral epiphyses. Approximately 25% of the longitudinal length of the femur originates from the proximal (capital) physis; the remaining 75% occurs from the distal physis (Figure 61-8).47,88,187,210 The afferent blood supply to the femoral diaphysis primarily arises from a branch of the medial circumflex femoral artery, which enters the large, principal nutrient foramen located within the proximal third of the facies aspera.74 Once within the medullary canal, this nutrient artery divides into numerous ascending and descending medullary arteries, which penetrate the endosteal surface and provide the blood supply to the diaphysis.227 Metaphyseal arteries anastomose with terminal branches of the ascending and descending medullary arteries; however, their contribution to the blood supply under normal conditions is minimal.227 In the event of a fracture, substantial hypertrophy of these arteries may occur, resulting in the creation of new vascular channels.227 Although periosteal vessels contribute to the diaphyseal blood supply in immature animals, their importance in adults is minimal. Periosteal arteries enter the diaphysis only along the facies aspera and are the sole blood supply to bone fragments in comminuted or segmental fractures.153,227 This emphasizes the importance of preserving local soft tissue and muscular attachments to limit iatrogenic trauma to the vascular supply.153,178,198 The distal femur is outlined by the trabecular network of the distal femoral metaphysis proximally and the condyles distally. The proximal portion of the distal metaphysis is referred to as the supracondylar region; its distal portion has a tetrahedral appearance and supports two epiphyseal projections known as condyles.74,153,165,198 The supracondylar region, including the supracondylar tuberosities and epicondyles, is the site of origin of numerous tendinous and ligamentous structures. The medial and lateral heads of the gastrocnemius muscle originate from their respective, caudally located, supracondylar tuberosities.74 The superficial digital flexor muscle also arises from the more prominent lateral supracondylar tuberosity. The collateral ligaments originate from each epicondyle, and the tendons of the popliteus and long digital extensor muscles have their respective origins on the lateral condyle and at the junction between the lateral epicondyle and the lateral ridge of the trochlear groove.74 The two condyles form the weight-bearing surface of the distal femur and are covered by articular cartilage. They are separated by the intercondylar fossa caudodistally and are continuous with the trochlear groove cranially. Each condyle articulates with the associated meniscus and to a lesser extent with the tibial plateau. The lateral condyle is larger and more convex in all planes when compared with the medial condyle.74 The intercondylar fossa is the femoral attachment site of the cranial and caudal cruciate ligaments on its lateral and medial surfaces, respectively. In addition, the caudolateral aspect of the fossa is the femoral attachment site of the lateral meniscofemoral ligament.74 The trochlear groove, located cranioproximally on the distal femoral epiphysis, is the site of articulation with the patella. The proximal two thirds of the groove is concave and is bound by the trochlear ridges, whereas the distal third of the groove is flat and merges with the condyles.74 The joint capsule of the stifle is the largest in the body, comprising a complex network of interconnecting sacs and subpouches.74 Its attachments surround the patella and extend over the trochlear ridges toward the epicondyles. Proximally, the cranial attachment of the capsule lies deep to the tendon of the quadriceps femoris muscle. The caudal attachment of the capsule lies deep to the heads of the gastrocnemius muscle and is closely associated with each fabella. In most nonchondrodystrophic dogs, the profile of the femoral condyles in the sagittal plane resembles that of a logarithmic spiral opening cranioproximally. This unique shape allows for efficient flexion and extension and moves the patella away from the center of rotation of the stifle joint, thereby providing a mechanical advantage to the quadriceps mechanism. In contrast, the distal epiphysis in chondrodystrophic breeds is relatively elongated and caudally oriented with respect to the diaphysis (Figure 61-9).136 This configuration likely generates greater bending moments at the level of the supracondylar region and in turn may predispose these breeds to supracondylar, as well as condylar, fractures.147 The distal femoral physis is responsible for approximately 75% of the longitudinal growth of the femur.47,88,187,198,210 The distal epiphysis of immature animals features four pyramidal grooves, which interdigitate with four similarly shaped metaphyseal pegs and give the physis its characteristic W shape. This unique geometry, which can be observed on mediolateral and craniocaudal radiographic projections (Figure 61-10), provides intrinsic resistance to rotational and shear forces during growth.21,198 As with the capital physis, the profile of the distal femoral physis is useful in providing stability during repair of fractures involving the physis. In dogs, closure of the distal femoral physis typically begins at 6 months and is complete by 9 to 12 months, with later closure observed in large- and giant-breed dogs.47,50,98,187,198,210 In cats, fusion begins at 4 months and is complete by 7 to 9 months of age.202 Distal metaphyseal vascularization is provided primarily by branches from the saphenous and descending genicular arteries off the femoral artery that enter all sides of the metaphysis.74,227 In addition, caudal genicular arteries from the popliteal artery arborize to supply the caudal part of the joint capsule, but also reinforce vascularization of the distal femur.74 Finally, terminal medullary branches from the principal nutrient artery anastomose with the metaphyseal arteries to complete this network of vessels.227 Presumably because of this robust blood supply, complications secondary to vascular compromise are uncommon with fracture of the distal femur. Nevertheless, minimizing iatrogenic trauma to the local vascular supply should always be considered during surgery to preserve optimal tissue healing. An adaptation of the AO (Arbeitsgemeinschaft für Osteosynthesefragen) system established for the classification of fractures in people can be applied to all long bones, including the femur, in dogs and cats.158,219 When this method is used, fractures are classified according to an alphanumeric system, based on the location, degree of comminution, and severity and prognosis of the fracture. Each long bone has been assigned a number (3 = femur), which is followed by a second number that denotes the relative position of the fracture within the bone (1 = proximal; 2 = shaft; 3 = distal). Additionally, each fracture is described with respect to its morphology (A = single fracture, B = wedge or butterfly fragment, C = complex or more than one fragment) and is assigned a final number corresponding to severity and prognosis (1 = least severe, good to excellent, 2 = moderate severity, guarded to good prognosis, 3 = severe, poor to guarded prognosis).116,178,219 Although this system is effective for sorting and retrieving data,116,219 fracture classifications based on anatomic and morphologic descriptions are often preferred because of their clinical relevance. The fracture is described with respect to its location within the proximal, diaphyseal, or distal region. Fractures of the proximal femur are commonly described as intracapsular or extracapsular, according to the location of the fracture with respect to the joint capsule (Figure 61-11).54 From proximal to distal, intracapsular fractures include epiphyseal, physeal, subcapital, and transcervical fractures (Figure 61-12). Similarly, from proximal to distal, extracapsular fractures include basilar neck, intertrochanteric, and subtrochanteric fractures. This classification system was proposed because of the capsule’s intricate association with the vascular supply to the femoral head and neck.54 Accordingly, it was speculated that intracapsular fractures would be more likely to result in avascular necrosis, and that the classification system could potentially be used as a prognostic indicator.54 Fractures of the distal femur are classified according to their anatomic location within the metaphysis or epiphysis (Figure 61-13).198 The term supracondylar is reserved for metaphyseal fractures, whereas the terms condylar and intercondylar are used to describe epiphyseal fractures.21,136,150,178,198 Although rare, bicondylar fractures occur, typically with simultaneous supracondylar fractures, and are commonly called T or Y fractures (Figure 61-14).178 In immature animals, proximal and distal physeal fractures are routinely described according to the Salter-Harris classification system.193,198 Femoral fractures are frequently associated with severe trauma; therefore, thorough evaluation and appropriate treatment of the animal for shock and for injuries involving the thoracic or abdominal cavity should be performed. Similarly, neurologic deficits and other orthopedic conditions should be addressed following stabilization of the animal. Preoperative splinting and/or bandaging of the femur is ineffective in providing adequate immobilization of the limb and instead creates a fulcrum at the fracture site, resulting in greater fracture displacement, increased soft tissue trauma, and intensified pain.178 For these reasons, it is commonly accepted that attempts at immobilization are ill advised and should be abandoned in favor of cage confinement, appropriate analgesia, and prompt surgical fixation. Most authors consider that, regardless of fracture location or pattern, internal fixation of femoral fractures is essential for a successful outcome.33,178,198 Radiographic Assessment of the Femur Following physical examination, fracture assessment and classification begins with radiographs of the fractured femur. Orthogonal radiographs of the affected limb are essential for accurate fracture evaluation. A magnification marker is required for templating, particularly with digital radiographs, and should be placed alongside the femur to decrease measurement errors (Figure 61-15, A–B). Special views taken to highlight a region of interest and radiographs of the contralateral, normal femur may be beneficial for thorough surgical planning. Radiographic assessment starts with a mediolateral radiograph of the affected limb. The patient is positioned in lateral recumbency with the sternum slightly elevated. With the affected limb resting on the table in a semi-flexed position, the contralateral limb is abducted and held in extension to effectively isolate the entire femur with minimal distortion and superimposition (see Figure 61-15, A). Next, a craniocaudal radiograph is obtained. This can be achieved via an extended ventrodorsal or horizontal beam projection. Although the ventrodorsal view is easily obtained with the patient in dorsal recumbency, because the femur cannot be positioned parallel to the cassette, distortion of the entire femur will occur (see Figure 61-15, A). This alters the perception of fracture lines and is particularly detrimental to the assessment of diaphyseal and distal fractures. The horizontal beam projection can be used to enhance visualization and reduce distortion. A caudocranial horizontal beam projection was initially proposed and was reported to produce a more accurate craniocaudal representation of the femur (see Figure 61-15, B).22 Instead, a craniocaudal horizontal beam projection is preferred by the authors to further reduce the amount of soft tissue superimposition over the hip joint (see Figure 61-15, B). In either case, horizontal beam projections require the use of a maneuverable radiographic tube. If further depiction of the fracture is required, a flexed ventrodorsal view (frog-leg) may prove beneficial for fracture(s) of the proximal femur.185 Oblique projections of the proximal femur are of little diagnostic value; however, their use for the distal femur, in combination with a tangential view of the trochlea, may be helpful. To further reduce fragment distortion, radiographs centered over the stifle joint can be added to the standard projections of distal femoral fractures. Given the limitations of standard, two-dimensional images, more detailed imaging via computed tomography (CT) should be considered, especially for the proximal and distal femur. All surgical approaches to the femur have been previously described in An Atlas of Surgical Approaches to the Bones and Joints of the Dog and Cat.179 This textbook is an integral component of any orthopedic procedure and should be referenced for complete, step-by-step descriptions of each approach. Numerous approaches to the proximal femur and hip joint have been described.* The most common techniques are performed with the patient in lateral recumbency and with the affected femur facing up. These include (1) the craniolateral approach, (2) the dorsal approach via osteotomy of the greater trochanter (Gorman approach), and (3) the dorsal approach via tenotomy of the gluteal muscles.* The craniolateral approach provides adequate exposure of the proximal epiphysis, physis, and neck. This approach is suitable for open reduction of nearly all epiphyseal, physeal, and cervical fractures and is the approach used most commonly for femoral head ostectomy. Additional exposure may be provided by a greater trochanteric osteotomy or, in very young animals, by a tenotomy of the superficial and deep gluteal muscles.179 Gentle tissue-handling skills and preservation of the vasculature must be applied with each approach to limit postoperative complications, especially in immature animals. Controversy continues as to which of these approaches is least detrimental to the epiphyseal blood supply. It has been suggested that the craniolateral approach potentially results in significant trauma to vessels supplying the extracapsular vascular ring, particularly the caudal gluteal and lateral circumflex femoral arteries.125 Similarly, however, some authors believe that a trochanteric osteotomy, as used in Gorman’s approach, invariably destroys the same vessels.19,54 As an alternative, to completely avoid interfering with the epiphyseal blood supply, a ventral approach can be used.94,104,131,199 This approach is suitable for fractures of the proximal epiphysis and capital physis, but it can also be used for femoral head ostectomy. However, it provides only limited exposure of the femoral head and requires that all implants be placed from the articular surface. Closed reduction with internal fixation using minimally invasive techniques is likely the most effective alternative for reducing iatrogenic injury to both the articular surface and the vascular network of the proximal femur. Although this technique is used most frequently by the authors for treatment of acute fractures, it requires the use of intraoperative fluoroscopy and training. Because of the bulkiness of the image amplifier, the patient’s pelvis must be elevated from the table to allow proper visualization of the hip joint in the craniocaudal and lateral planes (Figure 61-16). This in turn may complicate anesthetic procedures through thoracic compression by abdominal organs. The approach to the femoral diaphysis is almost exclusively through a lateral incision with the patient in lateral recumbency and the affected limb facing up.35,179 This approach provides exposure of the entire femoral diaphysis distal to the greater trochanter and proximal to the supracondylar region.179 The skin incision should be made along the craniolateral border of the diaphysis; this is followed by an incision in the superficial leaf of the fascia lata, just cranial to the biceps femoris muscle. Retraction of the biceps femoris muscle caudally and the vastus lateralis muscle cranially provides exposure of the entire femoral cortex.35,179 Proximally, the origin of the vastus lateralis muscle may be elevated off the craniolateral surface of the diaphysis for greater exposure of the subtrochanteric region.73,74,179 This approach can be combined with a craniolateral approach to the hip joint and a lateral parapatellar approach to the stifle for exposure of the entire femur.179 Multiple approaches have been described for exposure of the distal femur; they can be used individually or in combination.162,169,179 The patient should be positioned in dorsal recumbency so conversion to another approach can be made if necessary. Depending on the fracture location and complexity, as well as surgeon preference, a lateral, medial, or combined approach through the same skin incision can be made, all of which require stifle arthrotomy.178,179 A lateral approach is often preferred, as it can be extended proximally for exposure of the diaphysis if required.179 It provides adequate exposure of most supracondylar, lateral condylar, intercondylar, and distal physeal fractures.179 If greater access to the medial aspect of the distal femur is necessary, a medial approach should be used. It is not uncommon for articular, intercondylar, or comminuted fractures of the distal femur to require combined exposure. Osteotomy of the tibial tuberosity has been suggested for additional exposure in cases of articular fracture; however, the morbidity associated with this procedure typically negates any benefit derived from gained exposure.162,179 Its indication should be limited to severely comminuted articular fractures.17,179 Fractures of the proximal femur account for approximately 25% of all femoral fractures and are typically the result of severe trauma.31,178 In dogs, 91% of proximal femoral fractures occur in animals younger than 12 months of age (skeletally immature); nearly 70% of these fractures involve the capital physis (see Figure 61-6).54 Conservative treatment of these fractures consistently results in a poor functional outcome, characterized by chronic discomfort, persistent lameness, disuse muscle atrophy, secondary osteoarthritis, and the potential development of a hypertrophic pseudoarthrosis (Figure 61-17).176,198 Thus, conservative management is not considered a suitable option, and early surgical intervention is recommended. The repair of proximal femoral fractures, however, can be challenging because of several unique biologic and mechanical features, including (1) concurrent trauma to the fragile vascular network, (2) residual growth potential of the capital physis, (3) eccentric loading of the femoral head, (4) limited bone stock for stabilization, and (5) potential articular involvement. Surgical options for the treatment of proximal femoral fractures are broadly categorized as primary repair or salvage procedures. In the majority of cases, most authors recommend primary repair, as it is associated with a good functional outcome. Conversely, salvage procedures, such as total hip replacement or femoral head ostectomy, may be indicated for nonrepairable fractures or revision surgeries when necessary.53,115 The reduction technique and the method of stabilization should be selected in consideration of the animal’s age, duration between the inciting trauma and treatment, and fracture location with respect to the vascular anatomy. Prognosis is influenced by all of the aforementioned factors and varies from guarded to excellent.* Severe preexisting coxofemoral osteoarthritis is a contraindication for primary repair; a salvage procedure may be recommended instead. Epiphyseal fractures are rare in both skeletally immature and mature animals.54,168 Although an association with coxa plana has been suggested,168 most authors agree that these fractures occur in combination with coxofemoral luxation secondary to the inciting trauma. In these cases, the avulsed epiphyseal fragment commonly remains attached to the ligament of the femoral head (Figure 61-18).131,198,221 Appropriate treatment of these fractures is dependent on the number of epiphyseal fragments and on their size. Typically, the greater the number of fragments, the less likely articular reconstruction is to be achieved. Smaller fragments not amenable to fixation are excised to prevent injury to the articular cartilage (Figure 61-19). In contrast, when the fragment(s) is large enough, anatomic reduction and rigid fixation is performed to restore congruity of the articular surface. In these cases, because of the necessity for anatomic reduction and stable fixation, open reduction and stabilization through a craniolateral, dorsal, or ventral approach to the hip joint is recommended.94,130,131,152,213,214 However, when craniolateral or dorsal approaches are used, transection of the ligament of the femoral head is often required for adequate observation of the articular surface. Because this is believed to contribute to joint instability and subsequent osteoarthritis, a ventral approach to the hip has been devised.94,131,152,213,214 Following anatomic reduction, stabilization can be performed with Kirschner wires, small-diameter lag screws, or the combination of a Kirschner wire and a lag screw (see Figure 61-18). Regardless, a minimum of two implants should be used to resist rotational forces, and all implants must be countersunk below the level of the articular surface to prevent trauma to the cartilage of the acetabulum.94,130,213,214 The use of lag screw(s), however, has been associated with premature physeal closure in immature animals, resorption of the femoral neck, and greater degenerative changes over the acetabular surface.94,130,152,213,214 Finally, during closure, capsulorrhaphy is important in providing joint stability and aiding in the prevention of postoperative coxofemoral reluxation (see Figure 61-18).54 Augmentation techniques, such as a prosthetic joint capsule or an iliotrochanteric band, should be considered in cases where capsulorrhaphy is not feasible, or if coxofemoral instability remains following its application.4,32 Capital physeal fractures occur in skeletally immature animals secondary to trauma.198 A rare subset of these fractures, known as capital physeal dysplasia, is seen in young, mature animals and is discussed in the following section. Salter-Harris type I fractures of the capital physis, commonly referred to as slipped caps, are by far the most frequent physeal injury of the proximal femur (Figure 61-20).55,145 Concurrent separation of the trochanteric physis is seen in approximately 11% to 15% of cases.36,59,88 Surgical treatment is recommended as soon as the animal’s condition permits general anesthesia, as delay in reduction and stabilization allows for ongoing trauma to the local vasculature and physeal surfaces. Reduction and internal fixation of physeal fractures can be achieved using an open or closed approach. If an open approach is chosen, a craniolateral, dorsal, or ventral approach to the hip joint can be performed. For the dorsal approach, gluteal tenotomy should be reserved for animals younger than 3 to 5 months of age; otherwise osteotomy of the greater trochanter is recommended. With open approaches, the joint capsule is incised along preexisting tears to minimize additional trauma to the vascular network. Closed reduction, with the assistance of intraoperative fluoroscopy, is preferred by the authors because of its potential to limit iatrogenic trauma to the blood supply of the proximal femur. Regardless of the approach, anatomic reduction is required for an optimal outcome. The L-shaped profile of the capital physis helps guide reduction by providing landmarks for the restoration of normal anatomy; it also offers some intrinsic stability that counteracts shear forces once reduction is achieved.198 Multiple implants, including Kirschner wires, Steinmann pins, and bone screws, have been proposed for the stabilization of capital physeal fractures.* To prevent compression and iatrogenic closure of the physis, most authors recommend the use of multiple Kirschner wires or small-diameter Steinmann pins, as opposed to bone screws.116 It is often presumed, however, that regardless of the implant, the physis may close as a result of the inciting or surgical trauma. Pins can be placed in a normograde or retrograde fashion. Normograde insertion, in a distal-to-proximal direction, is the least invasive; however, accurate pin placement is technically challenging. Pin insertion should begin on the lateral aspect of the femur, caudodistal to the greater trochanter at the level of the third trochanter (Figure 61-21). For optimal anchorage, the pin is angled so its exit point is near the center of the capital physis, which can be facilitated by the use of a C-shaped drill guide. The first pin is inserted until its trocar tip appears at the fracture end, with all subsequent pins positioned in a similar fashion prior to reduction. Only after anatomic reduction is achieved are the pins advanced and secured within the proximal segment. Retrograde pinning has been described to provide more accurate pin placement and better spacing of pins within the capital physis.198 However, these benefits are offset by the extensive dissection of the fracture site required for placement. In addition, subsequent iatrogenic injury to the blood supply and physis presumably increases the risk of complications. Normograde pin placement from the articular surface has been described.* However, this technique is not recommended because it requires transection of the ligament of the head of the femur, which, in turn, results in coxofemoral instability and potentiates the early development of osteoarthritis. Although the ventral approach eliminates the need for transection of the ligament of the femoral head, it remains associated with the development of osteoarthritis because of the intra-articular placement of implants.94,152,213,214 Several studies have evaluated optimal pin diameter, number, and distribution within the femoral head and neck for effective stabilization of capital physeal fractures.* Although optimal pin diameter is dependent upon patient size, Kirschner wires (0.7 to 1.6 mm diameter) are typically sufficient in cats and in most small- and medium-breed dogs.53,115,198 Small-diameter Steinmann pins may be indicated for large- or giant-breed dogs.26,198 Clinical retrospective and in vitro studies have evaluated the number of pins required to resist physiologic forces within the proximal femur to limit the development of complications.25,26,55 A retrospective study evaluating clinical repair of capital physeal fractures, using one or two pins, or using three or four pins, did not find a significant association between pin number and the development of femoral neck resorption or osteoarthritis.55 The biomechanical strength and stiffness of capital physeal repairs with the use of one, two, or three 1.6-mm pins were compared in an in vitro study in small-breed dogs. Failure strengths using one or two pins were not significantly different from failure strengths of intact physes. The addition of a third pin, however, made the repair 29% stronger than an intact physis.26 This finding was challenged in a follow-up study, which showed that the mechanical strength of two-pin fixation was significantly weaker than that of intact controls.25 Inconsistency of results was attributed to slight variations in the age, weight, and general health of the patient.25 Based on these studies, and regardless of the patient’s size, a minimum of two pins is recommended to resist rotational and shear forces, but no more than three pins is considered necessary.25,26,55,198 Because implant failure is not a common complication following repair of these fractures, the use of additional pins is ill advised and only increases the likelihood of articular penetration, vascular compromise, and iatrogenic fracture. Pins placed in a parallel fashion offer biological and mechanical advantages when compared with divergent pins.132,198 Biologically, parallel pins allow for continued physeal growth, while divergent pins may create a locking effect on the physis, ensuring premature closure. Mechanically, forces applied to pins inserted in a parallel fashion are distributed equally between the pins. In contrast, with divergent pins, uneven distribution of loads between the implants renders the technique significantly weaker and thus predisposes the repair to failure.132 Because of the limited bone stock available proximal to the physis, the pins should be advanced as deeply as possible within the capital epiphysis to optimize implant anchorage. However, if the pins extend through the articular cartilage and into the hip joint, severe chondrolysis and degenerative joint disease will develop.52,141,142,186 The hemispheric contour of the epiphysis creates a challenging environment for accurate advancement in that the depth of penetration varies with the location of the implant.178 Fluoroscopically guided placement is ideal because the pins can be embedded within the subchondral bone at various locations, while ensuring that the articular cartilage has not been penetrated.141 In the absence of fluoroscopy, epiphyseal thickness can be estimated with the use of standard radiographs.141 In a cadaveric study using immature, small-breed dogs, it was determined that the contralateral epiphyseal depth and the pubic bone width, calculated from a ventrodorsal radiograph, have strong correlations with the actual epiphyseal depth.141 It was recommended that pins located within the center of the epiphysis can be advanced safely a distance equal to 75% to 80% of the contralateral epiphysis or width of the pubic bone, but eccentrically placed pins can be advanced only to a depth equal to 65% of these measurements.141 As a final option, one may purposely advance the pins until they can be seen or palpated while the articular cartilage is lifted.53,198 If the trocar point is not visible and the pin is believed to have passed into the articular cartilage, a blunt instrument may be used to sweep the surface of the femoral head for subtle irregularities. After the articular cartilage is penetrated, the pins are withdrawn slightly until the trocar is no longer within the joint. Although this technique causes minor damage to the articular surface, it guarantees maximal purchase of the epiphyseal bone and ensures that implants are not penetrating the joint. Although primary repair of capital physeal fractures is ideal, chronic fractures with subsequent remodeling may impede reduction and repair. In such cases, femoral head ostectomy should be recommended and is currently the preferred salvage procedure for immature animals. Despite its general acceptance, it remains a salvage procedure and is commonly associated with altered weight bearing, disuse muscle atrophy, lameness after exercise, and ankylosis.64,65,85,144,184,198 Early and aggressive postoperative rehabilitation is required following femoral head ostectomy to limit the development of complications and optimize an animal’s functional outcome. Recently, total hip replacement was reported in animals younger than 5 months of age.222 Despite this report, concerns regarding the size of the implant used, with respect to the animal’s size at skeletal maturity, have arisen. Therefore, total hip replacement as a salvage procedure for capital physeal fracture in immature animals, using current techniques and implants, should be considered at this time only with great caution.
Fractures of the Femur
Introduction
Surgical Anatomy
Proximal Femur
Anatomy of the Trochanters and Trochanteric Fossa
Growth of the Proximal Femur
Vascular Supply of the Proximal Femur
Femoral Diaphysis
Growth of the Femoral Diaphysis
Vascular Supply of the Femoral Diaphysis
Distal Femur
Growth of the Distal Femur
Vascular Supply of the Distal Femur
Fracture Classification
Surgical Planning
Imaging of the Femur
Surgical Approaches to the Femur
Proximal Femur
Femoral Diaphysis
Distal Femur
Specific Treatment
Epiphyseal Fractures
Capital Physeal Fractures
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Fractures of the Femur
Only gold members can continue reading. Log In or Register to continue