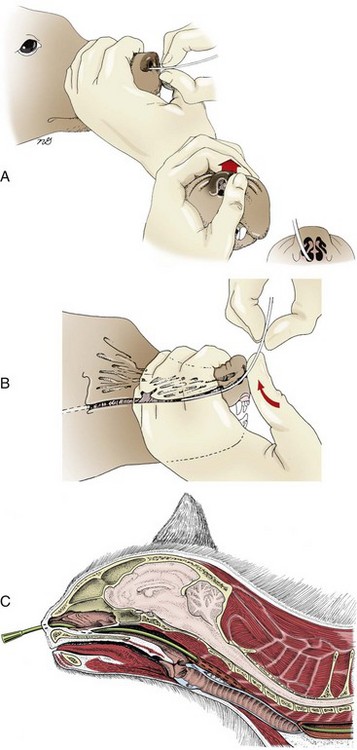
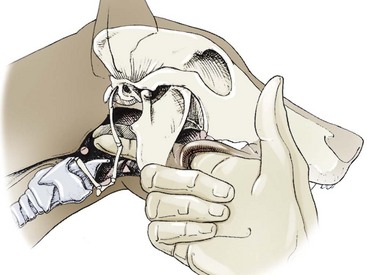
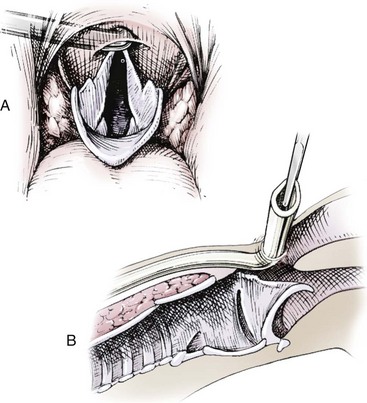
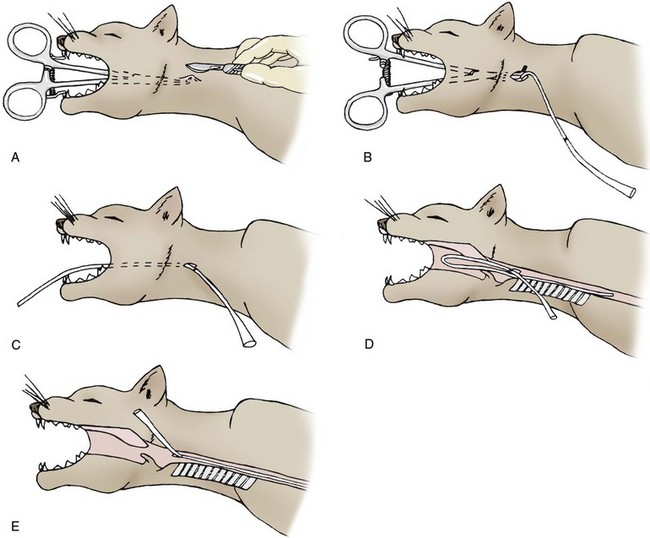
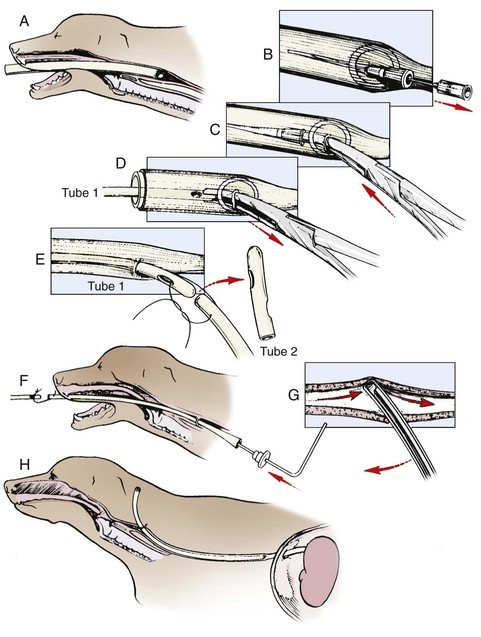
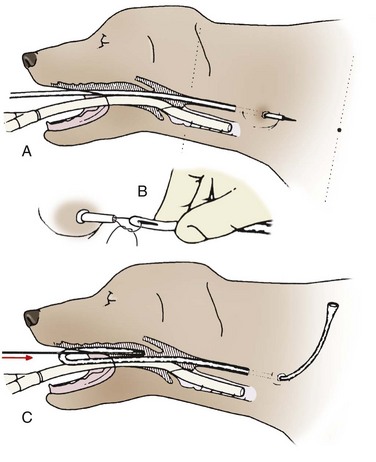
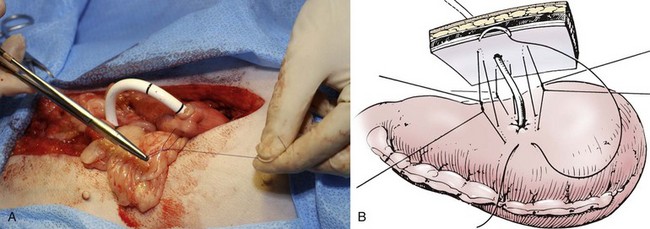
Chapter 98 Enteral nutrition is the preferred method of nutritional management in animals with little or no appetite that have conditions that permit enteral feedings. Early enteral nutrition is associated with more rapid clinical improvement. In animals with gut barrier dysfunction such as enteritis.36 The optimal site of nutrient delivery depends on several factors. In general, it is best to use the simplest method for which there are no contraindications and to allow the food to pass through as much of the gastrointestinal tract as possible. Patient factors to consider include the location of the disease, estimated length of time that nutritional support will be needed, risk of general anesthesia, and anticipated level of patient cooperation for the route selected. If nutritional support is anticipated for more than 1 or 2 days, an indwelling feeding tube will avoid the stress of repeated orogastric intubation. Indwelling tube locations include nasoesophageal, pharyngostomy, esophagostomy, gastrostomy, and enterostomy. Nasoesophageal intubation is the only procedure that does not require general anesthesia. Enteral nutrition is generally considered to be safer, easier, more physiologic, and less expensive than parenteral nutrition. Although some animals may need a sedative or short-acting anesthetic, most nasoesophageal tubes can be placed using only a local anesthetic on the nasal mucosa. Four or five drops (0.5 to 1.0 mL) of 0.5% proparacaine hydrochloride or 2% lidocaine hydrochloride are instilled in the animal’s nostril, and the nose is tilted upward for a few seconds.1,15 Some clinicians will instill anesthetic in both nostrils to improve coverage of the nasopharyngeal region. A small-diameter (5- or 6-Fr) polyurethane or silicone elastomer tube is appropriate for most animals.15,16 Polyvinyl chloride or red rubber tubes may also be used, but polyvinyl chloride tubes may harden and cause irritation. The tube should be long enough to be placed with the tip positioned in the mid to distal esophagus. Tubes passing the lower esophageal sphincter may promote gastroesophageal reflux and esophagitis. The distance to the midthoracic esophagus is determined by measuring from the animal’s nose to the seventh or eighth rib; this distance is marked on the tube. The tube tip is lubricated with water-soluble lubricant or 5% lidocaine gel.15,16 The tube is passed through the ventral meatus. In cats, the tube is simply inserted ventromedially through the nostril.15,16 In dogs, the tube must bypass a ventral protuberance before entering the ventral meatus.15,16 This can be facilitated by inserting the tube several centimeters in a ventromedial direction until it reaches the floor of the nasal cavity. The external nares are then pushed dorsally to provide a straight path for the tube into the ventral meatus (Figure 98-1).1 The animal’s head should be maintained in a neutral position while the tube is gently advanced into the pharyngeal region to decrease the risk of tracheal intubation. The animal will usually swallow repeatedly as the tube enters the esophagus. The tube is advanced to the predetermined distance in the esophagus. Proper tube placement can be verified by injecting 5 to 10 mL of air through the tube and auscultating for borborygmus. Alternatively, 3 to 5 mL of sterile water may be injected through the tube. This will induce a cough if the tube is located in the airway.1,15 If the tube is radiopaque, a survey radiograph may be used to confirm the tube location. The tube is secured to the animal’s head by suturing it to the skin or gluing it to the hair with cyanoacrylate. The tube is most secure if it is first anchored as close as possible to the nostril. It can also be anchored on the dorsal nasal midline just rostral to the eyes. Although most animals tolerate nasoesophageal tubes, an Elizabethan collar may be used to prevent premature dislodgement.2 Tube removal is facilitated by clipping the hair where the glue is attached. Complications of nasoesophageal feeding tubes are usually minor and may include epistaxis, dacryocystitis, rhinitis, sneezing, and premature tube removal.1,2,15,16 Vomiting and diarrhea are also reported but are usually related to feeding and can be resolved by adhering to the recommended protocol or changing the diet.2,14 Aspiration pneumonia may occur if the end of the tube is displaced into the pharynx when the animal vomits or regurgitates. Because of this, proper tube placement should be verified before each feeding by instilling a small amount of water through the tube and watching for signs of respiratory irritation. Gastroesophageal reflux and esophagitis may occur if the tip of the feeding tube is placed in the stomach.20,29 Because of their small size, nasoesophageal tubes are prone to obstruction even when commercial liquid diets are used. Soft tubing, such as red rubber or silicone, is recommended for pharyngostomy feeding tubes. The tube size is dependent on the animal’s size; generally, size 8- to 14-Fr tubes are appropriate for cats or small dogs, and size 12- to 28-Fr tubes are appropriate for medium or large dogs.16 Smaller tubes are less rigid and require a stylet for placement. They are also more prone to dislodgement by the animal.16 Tubes smaller than 8-Fr require feeding of liquid foods, 16and tubes larger than 14-Fr permit feeding of blenderized commercial pet foods. Tubes are premeasured and marked so that the tip of the tube rests at the level of the seventh or eighth rib after they are placed. Some surgeons prefer to remove the blind end of tube to avoid a recess for food entrapment. If the tube tip is removed, the tube can be cut to an appropriate length to reduce the amount of dead space. The animal is anesthetized and placed in right or left lateral recumbency. A region of the skin defined by the base of the ear canal, ventral midline, mandibular ramus, and larynx is surgically clipped and aseptically prepared. One hand is placed in the oropharynx to palpate the epihyoid bone on the lateral wall of the pharynx, and a fingertip is positioned caudal to the epihyoid bone at the most dorsal aspect of the pharynx (Figure 98-2).20 The finger may be pressed against the lateral pharyngeal wall to create a bulge that is visible externally. Anesthesia must be deep enough to prevent stimulation of swallowing or chewing during pharyngeal manipulation. A 0.5- to 1.0-cm incision is made in the skin over the fingertip.20 Compression of the external jugular vein will distend the maxillary and linguofacial veins so they may be visualized and avoided. A curved Kelly forceps is used to bluntly dissect the subcutaneous tissues and muscle from the incision to the fingertip.20 Blunt dissection helps avoid injury to the many vessels (carotid artery, jugular vein), nerves (vagosympathetic trunk, hypoglossal, glossopharyngeal), and salivary glands in this region.20 The forceps is pushed through the pharyngeal wall; some force may be needed.16 The premeasured feeding tube is passed from the oral cavity into the distal esophagus. The flared end of the feeding tube is grasped with the Kelly forceps and pulled through the dissected region.20 The tube can then be adjusted so its tip is in the desired location within the esophagus. Oral palpation or laryngoscopic examination is performed to confirm that the tube is dorsal and caudal to the epiglottis and is not kinked (Figure 98-3). The feeding tube is secured to the skin with a fingertrap suture technique.16,45 The stoma around the tube is left open (no purse-string placement). A light bandage may be placed around the neck to cover the pharyngostomy site. A small amount of drainage may occur at the wound site, so the bandage should be changed and the peristomal skin cleaned every 2 to 3 days. The tube should be flushed with water and capped when not in use to prevent tube obstruction and influx of air or reflux of food.16 Patients should be in a sternal, head-elevated, or standing position when fed to avoid pooling of fluid and food within the esophagus. Proper tube placement is important to reduce the incidence of complications. Blunt dissection of the tissues avoids nerve damage and hemorrhage. The pharyngostomy tube should pass through the caudodorsal pharynx near the esophageal ostium. A tube that is kinked, placed too cranially, or too large may interfere with the epiglottis, resulting in coughing, dyspnea, or aspiration pneumonia.20 An improperly placed tube may also obstruct the larynx and cause complete or partial airway blockage. Pharyngostomy tubes that enter the stomach have been shown to cause gastroesophageal reflux and esophagitis.20,29 Also, the physical presence of tubes within the esophagus causes esophageal erosion and ulceration in the region of tube contact.29 Termination of the tube within the midthoracic esophagus reduces the likelihood of reflux esophagitis and limits the area of mechanical erosion to a portion of the esophagus that is less likely to have contact with refluxed material.29 Other complications associated with pharyngostomy tubes include regurgitation, vomiting, local infection, and premature tube displacement.20,29 Esophagostomy tubes may be placed in either side of the neck, although some surgeons prefer to place them through the left side. The animal is anesthetized and placed in lateral recumbency, and the midcervical region is clipped and aseptically prepared. The feeding tube is measured, marked, and shortened (if desired) in the same manner as for pharyngostomy tubes. Several techniques have been described for esophagostomy tubes.17,23,40,50 Manual (Unassisted) Transesophageal Advancement: An advantage of this technique is that larger tubes can generally be used, compared with those placed with other techniques.17 A long, curved forceps (e.g., narrow-tipped Carmalt) is passed through the oral cavity into the esophagus (Figure 98-4). The forceps tips are pressed laterally to create a bulge on the neck that can be observed and palpated. A stab incision is made in the skin over the forceps tips, and the forceps are bluntly forced through the incision. Alternatively, the forceps are first forced through the esophageal wall and subcutis and then a skin incision is made over the tips after they are easily palpable. Passage of the forceps tips through the esophageal wall usually requires great force and can be facilitated by placing external pressure on the neck at the expected exit site with one fist while pressing against the rings of the forceps handle with the opposite palm. Needle-Assisted Percutaneous Placement: A long, curved forceps is advanced transorally into the midcervical esophagus, as described above for the surgical technique. The forceps tips are opened slightly, and a 14 gauge needle is inserted through the skin and soft tissues into the esophageal lumen. A small polyvinyl chloride, red rubber, or jugular catheter is inserted through the needle into the esophageal lumen. The premeasured feeding tube is advanced until the tip is in the midthoracic or distal esophagus. The feeding tube length and position are determined in the same manner as for nasoesophageal feeding tubes. With this technique, the needle must either be left in place on the tube, risking tube damage, or the adaptor end of the tube must be excised so the needle can be removed. Tube-Assisted Percutaneous Placement: This esophagostomy technique allows placement of a larger feeding tube than the needle-assisted technique.40 It uses a technique similar to that for a percutaneous endoscopic gastrostomy tube and requires more equipment and attention to detail than manual transesophageal forceps advancement. A rigid polyvinyl chloride tube is placed transorally and into the esophagus to serve as a guide (Figure 98-5). The end of the guide tube is cut at an oblique angle and pressed laterally against the esophageal wall. A small (2 to 3 mm) skin incision can be made at the proposed esophagostomy tube site, if desired. A rigid, 18-gauge, over-the-needle catheter is inserted through the incision, subcutaneous tissues, and esophageal wall and into the guide tube lumen. The needle is removed from the catheter. The tips of a Carmalt forceps are placed in the hub of the catheter, and the catheter and forceps are forced through the subcutis and esophageal wall and into the lumen of the guide tube. The catheter facilitates blunt tissue separation to allow forceps advancement. The external end of the guide tube is lowered, allowing the catheter to fall out. Eld Percutaneous Feeding Tube Applicator: Devitt and Seim23 described the use of a trocar-tipped applicator for percutaneous esophagostomy tube placement. The end of the applicator, containing a sheathed trocar, is inserted through the oral cavity into the midcervical esophagus (Figure 98-6). A small incision is made through the skin and subcutaneous tissue over the tip of the applicator. The trocar is advanced through the esophageal wall and incision, and the tip of the feeding tube is sutured to the eyelet of the trocar. The trocar is retracted, and the Eld applicator is removed from the mouth, pulling the feeding tube with it through the esophagus and oral cavity. The suture between the applicator trocar and the feeding tube is cut. A stylet is inserted into a side hole of the feeding tube to facilitate redirection of the tube into the distal esophagus. Esophageal Feeding Tube Applicator: Esophagostomy tubes can be placed percutaneously with a special esophageal applicator (Esophageal Feeding Tube Applicator, Firma Fixomed, Munich, Germany) that permits immediate normograde placement, thus avoiding the need for tube repositioning.50 The applicator is bowed, has a length of 25 cm, and is structured with a 1.6-cm “bulb” near its distal end. Through and beyond the bulb is an 8-mm-wide groove that runs to the tip of the applicator. The applicator is passed through the mouth until its bulb can be palpated in the midcervical region. A 1- to 2-cm incision is made through the skin over the bulb, and a forceps is used to bluntly dissect down to the esophageal wall. A stab incision is made through the esophageal wall, and the esophageal tube is passed into the groove of the bulb and directed normograde along the remainder of the trough until it reaches the midthoracic esophagus. After an esophagostomy tube is in place, the catheter is secured to the skin with a finger-trap suture46 or tape butterfly. The stoma around the tube is left open (no purse-string placement), and the neck is wrapped with a light bandage. The esophagostomy site should be cleaned and rebandaged daily to reduce the likelihood of local infection. The tube should be flushed with water and capped when not in use. Feeding may be initiated within hours after tube placement. Patients should be in a sternal, head-elevated, or standing position when fed to avoid pooling of fluid and food within the esophagus. When the esophagostomy tube is no longer needed, it is removed, and the wound is allowed to heal by second intention.17,23 Esophagostomy tubes may be removed the same day they are placed without concern for leakage.17 Animals may eat immediately after tube removal.30 Reported complications of esophagostomy are usually minor and may include stomal infection or abscessation, tube kinking, tube obstruction, and tube displacement caused by vomiting.17,19,23,30 Vomiting may occur if the tube is passed through the distal esophageal sphincter or may be related to underlying disease. Midesophageal placement of the tube reduces the incidence of esophageal injury and reflux esophagitis.29 Rarely, esophageal leakage through tears or perforation may occur in animals with friable tissues (e.g., very young patients), when overly large instruments are used to penetrate the esophageal wall, or when multiple attempts are necessary for tube placement (Figure 98-7). Sharp dissection of subcutaneous tissues may result in severe hemorrhage if major vessels are lacerated. Indications and Contraindications Gastrostomy tubes may be placed in anticipation of anorexia or inability to eat. They are also indicated for animals in which the oral cavity, pharynx, and esophagus must be bypassed because of injury, disease, or obstruction or after pharyngeal or esophageal surgery when the presence of a feeding tube could interfere with healing. Because they are safe, relatively easy to place, and permit administration of blenderized foods, many clinicians prefer gastrostomy tubes over pharyngostomy or esophagostomy tubes even when the esophagus is normal. Gastrostomy tubes may be left in place for months and are well tolerated by most animals. They do not interfere with prehension, deglutition, or digestion of food; therefore, the animal can begin eating voluntarily while being supplemented with tube feeding. Most owners become comfortable feeding their pets through a gastrostomy tube provided they are given clear instructions and remain in communication with the veterinarian while the tube is in place.43 Gastrostomy tube placement is not recommended in animals with primary gastric disease or persistent vomiting. Gastrostomy tube feeding should be used with caution in animals with a dysfunctional esophagus or abnormal mentation because these animals have a higher risk of aspiration pneumonia.4 Surgical Placement: An advantage of the surgical method is that the stomach can be secured to the abdominal wall with sutures rather than relying on later adhesion formation. Surgical placement of gastrostomy tubes may be performed during routine ventral midline celiotomy or through a limited left paracostal approach. The animal is anesthetized and intubated with a cuffed endotracheal tube to prevent aspiration in the event of regurgitation or reflux. For a paracostal approach, the animal is placed in right lateral recumbency, and the left paracostal region is clipped and aseptically prepared for surgery. A 2- to 5-cm incision is made parallel and several centimeters caudal to the last rib and ventral to the paravertebral epaxial musculature.13,16 The external abdominal oblique, internal abdominal oblique, and transverses abdominus muscles are separated between their fibers.13 The internal abdominal fascia is incised. The body of the stomach is identified and brought to the incision using a Babcock forceps or by means of a large, stiff orogastric tube.13,16,44 With a midline abdominal approach, the stomach, pylorus, and intestines are examined for abnormalities before tube placement. With either approach, temporary stay sutures or a Babcock forceps may be used to maintain retraction of the stomach.13 A full-thickness purse-string suture of 2-0 or 0 absorbable monofilament is placed in the wall of the proximal half of the left gastric body, and a full-thickness stab incision is made in the center of the purse string. The tip of a mushroom-tipped catheter is placed through the stab incision into the stomach lumen. The mushroom-tipped catheter may exit through the limited abdominal wall incision when a paracostal approach is used or through a separate stab incision when a midline approach is used. Some clinicians pass the catheter through a layer of omentum before advancing it into the stomach to help contain potential leakage as the site heals; the effects of this technique on adhesion formation along the gastropexy site are not known. The stomach is sutured to the internal abdominal wall with 2-0 polydioxanone, polyglyconate, or polypropylene in a simple continuous or simple interrupted pattern (Figure 98-8).16 If desired, the gastropexy site can be encircled with omentum, which is tacked in place. The abdominal wall is closed routinely, and the catheter is secured to the skin with a fingertrap suture technique.45
Feeding Tubes
Methods Of Delivering Enteral Nutrition
Nasoesophageal Tubes
Technique
Complications
Pharyngostomy Tubes
Technique
Complications
Esophagostomy Tubes
Technique
Aftercare
Complications
Gastrostomy Tubes
Techniques
< div class='tao-gold-member'>
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Feeding Tubes
Only gold members can continue reading. Log In or Register to continue