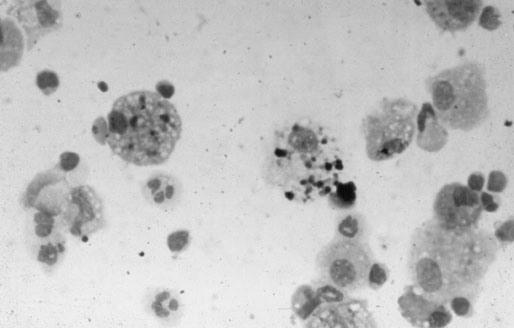
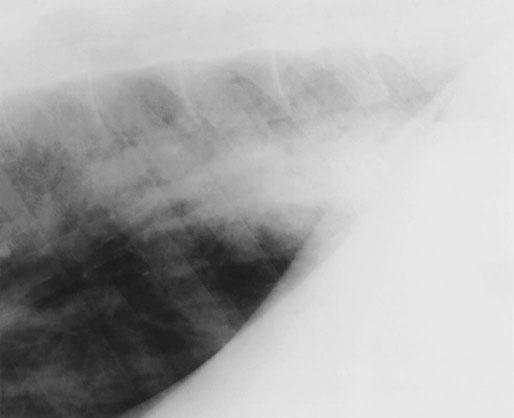
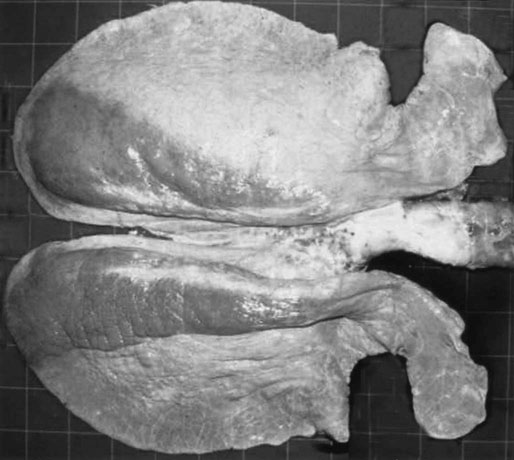
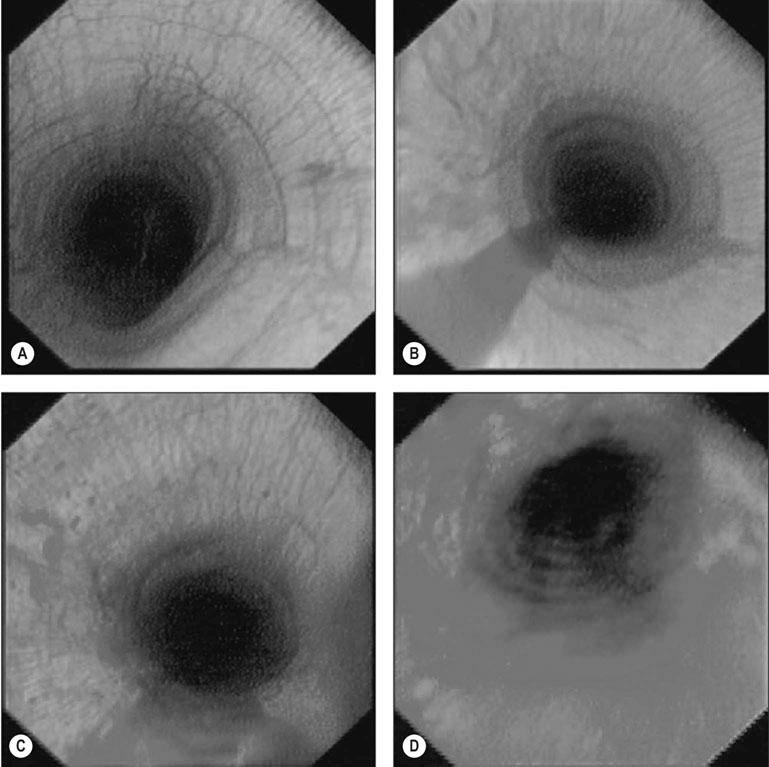
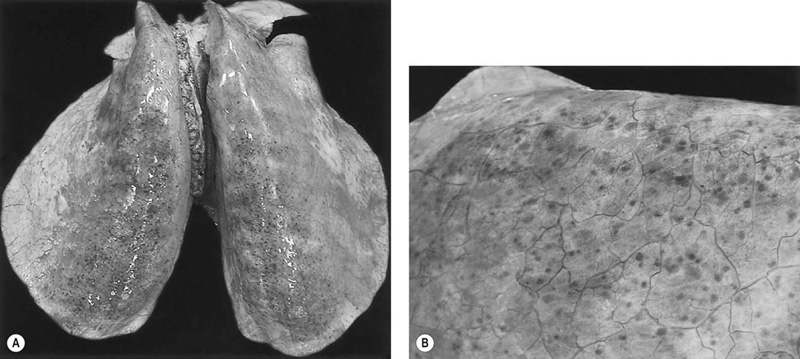
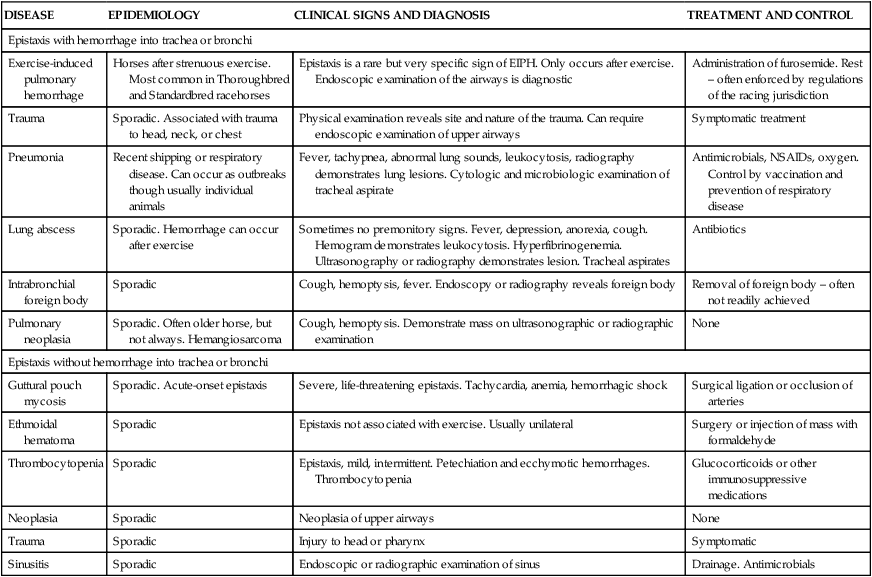
• Exercise-induced pulmonary hemorrhage is a common disorder of athletic horses, among which it occurs worldwide. • EIPH is a cause of poor performance and infrequently manifests as epistaxis during or after exercise. It rarely causes death. • Diagnosis is based on demonstration of blood in the airways after exercise either by tracheobronchoscopy or examination of fluid obtained by tracheal aspiration or bronchoalveolar lavage. • Furosemide is commonly used to treat EIPH and is efficacious in reducing both severity and frequency of bleeding – efficacy of other medications has not been demonstrated under field conditions. • EIPH is likely caused by rupture of pulmonary capillaries with subsequent development of pulmonary inflammation, fibrosis and angiogenesis contributing to continued hemorrhage during exercise. Failure of racehorses to perform to the expected standard (poor performance) is often attributed to EIPH likely because many horses with poor performance have cytologic evidence of EIPH on microscopic examination of tracheobronchial aspirates or bronchoalveolar lavage fluid or have blood evident on endoscopic examination of the tracheobronchial tree.1,2 A relationship between finishing position and incidence of EIPH, diagnosed by bronchoscopic examination, was not detected in a number of studies of relatively small numbers of horses or a non-random selection of horses.3,4,5 In contrast, a prospective observational study with strict entrance criteria and which included examination of over 700 horses, approximately 50% of all horses racing during the period of the study, demonstrated that exercise-induced pulmonary hemorrhage is a cause of poor performance in Thoroughbred racehorses.6 Horses with EIPH of grade 1 or less (on a scale of 0–4)7 were 4.0 times more likely to win, 1.8 times more likely to finish in the top three positions, 3.0 times more likely to earn above the 90th percentile of earnings than horses with EIPH of grade 2 or greater.6 Horses with EIPH of grade 2 or greater finished significantly further behind the winner than did horses with less severe hemorrhage or no evidence of hemorrhage. These findings are consistent with a study of 452 Thoroughbred horses examined after racing in Hong Kong which demonstrated that those finishing in the first three positions had less severe EIPH than did horses finishing in lower positions.8 Of horses finishing in the first three places, 43.9% had evidence of EIPH on tracheobronchoscopic examination after racing, whereas 55.9% of horses finishing in 4th to 14th place had evidence of EIPH. Exercise-induced pulmonary hemorrhage is an important cause of reduced athletic performance in Thoroughbred racehorses because of its high frequency and the magnitude of its association with impaired performance. Results of studies in Standardbred racehorses indicate either a lack of effect of EIPH on performance or an association between EIPH and superior performance. There was not a relationship between presence of EIPH and finishing position in 29 Standardbred racehorses with intermittent EIPH examined on at least two occasions,9 nor in 92 Standardbred racehorses examined on one occasion.10 However, of 965 Standardbred racehorses examined after racing, those finishing first or second were 1.4 times more likely (95% CI 0.9–2.2) to have evidence of EIPH on tracheobronchoscopic examination than were horses that finished in 7th or 8th position.11 The relationship between EIPH and performance in Standardbred horses is unclear, largely because of the lack of appropriately designed large-scale studies. An association between EIPH and athletic performance has not been demonstrated for other breeds. Exercise-induced pulmonary hemorrhage is infrequently associated with sudden death during racing or training. Of 143 horses subject to detailed post-mortem examination after death during racing or training, 50 died with severe pulmonary hemorrhage (the presumed cause of death).12 Apart from epistaxis in a small proportion of EIPH-affected horses, there are few abnormalities detectable on routine physical examination of horses with EIPH.13 Rectal temperature and heart and breathing rates are elevated as a consequence of exercise in horses examined soon after exercise, but values of these variables in horses with EIPH at rest are not noticeably different to horses with no evidence of EIPH.14 Affected horses might swallow more frequently during recovery from exercise than do unaffected horses, probably as a result of blood in the larynx and pharynx.15 Coughing is common in horses recovering from strenuous exercise and horses with EIPH are reported to have a hacking cough, although this observation is not very specific.3 After recovery from exercise, horses with EIPH are no more likely to cough than are unaffected horses.16 Other clinical signs related to respiratory abnormalities are uncommon in horses with EIPH. Respiratory distress is rare in horses with EIPH and when present indicates severe hemorrhage or other serious lung disease such as pneumonia, pneumothorax or rupture of a pulmonary abscess. Lung sounds are abnormal in a small number of EIPH-affected horses and when present are characterized by increased intensity of normal breath sounds during rebreathing examination.14 Tracheal rales can be present in horses with EIPH but are also heard in unaffected horses.15 Epistaxis associated with exercise is almost always attributable to pulmonary hemorrhage. The severity of epistaxis ranges from flecks or a small amount of blood at one nostril present after the horse lowers its head at the end of exercise to profuse hemorrhage from both nostrils occurring during exercise (Fig. 29.1). Epistaxis occurs in a small proportion racehorses.3,6,15,17–21 The prevalence of epistaxis in racehorses varies between 0.1 and 9.0%, with the frequency depending on the breed, age and sex of horses selected for study, the type of racing, and the timing and frequency of observation of horses after racing (See ‘Epidemiology’). Epistaxis occurs in 0.13% of Thoroughbred racehorses in Japan,18 5.9% of Thoroughbreds in Hong Kong,8 0.8% of Thoroughbreds in California,3 9.0% of Thoroughbreds in Pennsylvania,4 0.8% of Thoroughbreds in Australia,6 and 3.5% of Quarter Horses in the USA.20 The recurrence rate after one episode of epistaxis in Thoroughbred horses is approximately 13.5% despite affected horses not being permitted to race for one month after the initial episode of epistaxis.18 For this reason most racing jurisdictions do not permit horses with epistaxis to race for a period of weeks to months after the initial instance, with more prolonged enforced rest after a subsequent episode of epistaxis and retirement from racing after a third bout. This high rate of recurrence suggests that the inciting pulmonary lesions have not healed. There are not clinically important abnormalities in routinely measured hematologic, blood gas and blood biochemical tests in resting horses with EIPH.13 Observation of blood in the trachea or large bronchi of horses 30–120 minutes after racing or strenuous exercise provides a definitive diagnosis of EIPH. The amount of blood in the large airways varies from a few small specks on the airway walls to blood covering most of the luminal surface of the trachea and extending into the larynx, nasopharynx and nasal cavities (Fig. 29.2).7 If there is a strong suspicion of EIPH and blood is not present on a single examination conducted soon after exercise, the examination should be repeated in 60–90 minutes. Some horses with EIPH do not have blood present in the rostral airways immediately after exercise, but do so when examined 1–2 hours later. Blood is detectable by tracheobronchoscopic examination for 1–3 days with some horses having blood detectable for up to seven days. Bronchoscopic examination can be used to estimate the severity of EIPH through use of a grading system.3,7–9,22 A validated grading system has a scale of 4 levels (Fig. 29.2): 7 • Grade 0 = no blood detected in the pharynx, larynx, trachea, or mainstem bronchi • Grade 1 = presence of 1 or more flecks of blood or 2 or fewer short (less than one-quarter the length of the trachea) narrow (<10% of the tracheal surface area) streams of blood in the trachea or mainstem bronchi visible from the tracheal bifurcation • Grade 2 = 1 long stream of blood (greater than half the length of the trachea) or more than 2 short streams of blood occupying less than a third of the tracheal circumference • Grade 3 = multiple, distinct streams of blood covering more than a third of the tracheal circumference, with no blood pooling at the thoracic inlet • Grade 4 = multiple, coalescing streams of blood covering more than 90% of the tracheal surface with blood pooling at the thoracic inlet. There is a high concordance amongst trained observers using this grading system (weighted kappa of 0.75 to 0.80) with fewer than 0.5% of observations differing by two or more grades.7 It is assumed that a higher score represents more severe hemorrhage, but while the repeatability of this scoring system has been established, the relationship between the amount of blood in the large airways and the actual amount of hemorrhage has not been established. The presence of red cells or macrophages containing either effete red cells or the breakdown products of hemoglobin (hemosiderophages) in tracheal or bronchoalveolar lavage fluid provides evidence of EIPH (Fig. 29.3). Detection of red cells or hemosiderophages in tracheal aspirates or bronchoalveolar lavage fluid is believed to be both sensitive and specific in the diagnosis of EIPH.1,23 Examination of airway fluids indicates the presence of EIPH in a greater proportion of horses than does tracheobronchoscopic examination after strenuous exercise or racing. The greater sensitivity of examination of airway fluid is likely attributable to the ability of this examination to detect the presence of small amounts of blood or its residual products and the longevity of these products in the airways. While endoscopic examination detects blood in occasional horses up to seven days after an episode of EIPH, cellular evidence of pulmonary hemorrhage persists for weeks after a single episode.1,23–26 Red blood cells and macrophages containing red cells are present in bronchoalveolar lavage fluid or tracheal aspirates for at least one week after strenuous exercise or instillation of autologous blood into airways and hemosiderophages are present for at least 21 days and possibly longer.1,23–26 Red cell numbers in bronchoalveolar lavage fluid are used as a means of detecting EIPH, a quantitative indicator of severity of EIPH and for monitoring efficacy of treatments.25,27–30 However, identification of hemosiderophages or red blood cells in tracheal aspirates, or hemosiderophages in bronchoalveolar lavage fluid, does not provide a reliable measure of the severity of pulmonary haemorrhage in a model using intrapulmonary administration of blood.24 The assumptions underlying the use of this technique are that it is a more sensitive indicator of EIPH than tracheobronchoscopic examination of airways, and that the red blood cell count in lavage fluid is proportional to the severity of haemorrhage. While it is very probable that detection of red blood cells in bronchoalveolar lavage fluid is a more sensitive indicator of EIPH than tracheobronchoscopic examination,31 the usefulness of red cell counts in bronchoalveolar lavage fluid as an indicator of severity of haemorrhage is less clear given that an unknown area, although presumably small, of the lung is examined by lavage and there is a risk that this area of lung might not be representative of the lung as a whole, similar to the situation of examination of bronchoalveolar lavage fluid of horses with pneumonia.32,33 However, other methods of determining severity of EIPH, including pulmonary scintigraphy and pulmonary function tests,34,35 have to date proved unable to detect or quantify hemorrhage, leaving measurement of red cell count in bronchoalveolar lavage fluid as a viable but perhaps less than optimal method of quantification. For both endoscopic and lavage tube collection of bronchoalveolar lavage fluid the horse is restrained and sedated (xylazine 0.5–1.0 mg/kg iv, detomidine 20–40 micrograms/kg IV). Some clinicians administer butorphanol (0.02–0.5 mg/kg IV) or local anesthetic (lidocaine, 20 mL of a 2% solution diluted with saline to a total volume of 100 mL and administered into the trachea) to suppress coughing. Application of a nose twitch may be necessary in some horses. The endoscope or lavage tube is passed into the trachea and then advanced caudally until it wedges in the distal airway. The cuff of the lavage tube is then inflated and a quantity of fluid (150–300 mL) of isotonic fluid (phosphate buffered 0.9% sodium chloride or similar) rapidly injected. After allowing the horse several breaths, the fluid is aspirated with the first 20 mL being discarded. Blind passage of the lavage tube usually results in its lodging in the dorsocaudal lung region.36 Thoracic radiography is of limited sensitivity in detecting horses with EIPH. Radiographs can demonstrate the presence of densities in the caudodorsal lung fields of some horses (Fig. 29.4),37–39 but many affected horses have minimal to undetectable radiographic abnormalities and unaffected horses can have marked abnormalities. The severity of radiographically apparent pulmonary abnormalities was not significantly different between horses with EIPH and control horses.13 Examination of thoracic radiographs of horses with EIPH can be useful in ruling out the presence of another disease process, such as a pulmonary abscess, contributing to the horse’s pulmonary hemorrhage or poor athletic performance, but are not sensitive for the detection of EIPH. During incremental exercise on a treadmill, horses with EIPH have more severe exercise-induced arterial hypoxemia, hypercapnia and higher blood lactate concentrations than do control horses41 although this is not a consistent finding.42 These changes indicate abnormalities in gas exchange in horses with EIPH but are not sufficiently large; nor do they have sufficient sensitivity to be useful clinically. Blood gas tensions in resting horses with EIPH are within the normal ranges. Exercise-induced pulmonary hemorrhage is a rare cause of death of racehorses. Necropsy examination of affected horses is usually incidental to examination for another cause of death. Pertinent abnormalities in horses with EIPH are restricted to the respiratory tract. Grossly, horses examined within hours of strenuous exercise, such as horses necropsied because of catastrophic musculoskeletal injuries incurred during racing, can have severe petechiation in the caudodorsal lung fields (Fig. 29.5). Horses with chronic disease have blue/gray or blue/brown discoloration of the visceral pleural surfaces of the caudodorsal lung fields that is often sharply demarcated, especially on the diaphragmatic surface (Fig. 29.6).43 The discoloration affects both lungs equally with 30–50% of the lung fields being discolored in severe cases.43 Affected areas do not collapse to the same extent as unaffected areas and, in the deflated lung, have a spleen-like consistency.43 On cut surface, the discolored areas of lung are predominantly contiguous with the dorsal pleural surface and extent ventrally into the lung parenchyma. Areas of affected lung may be separated by normal lung. There is proliferation of bronchial vessels, predominantly arteries and arterioles, in affected areas.44 Histologically, affected areas exhibit bronchiolitis, hemosiderophages in the alveolor lumen and interstitial spaces, and fibrosis of interlobular septa, pleural and around vessels and bronchioles.45 There are a variety of causes of epistaxis, pulmonary hemorrhage or both in horses,46 although most are not associated solely with exercise (Table 29.1). Presence of EIPH is most immediately confirmed by tracheobronchoscopic examination of the horse after strenuous exercise. Detection of red blood cells or hemosiderophages in tracheal aspirates or bronchoalveolar lavage fluid is also indicative of EIPH. The finding of hemorrhage in the airways of a horse soon after exercise allows a strong presumptive diagnosis of EIPH. Table 29.1 NSAIDs – non-steroidal anti-inflammatory drugs. Modified from Radostits et al. Veterinary Medicine. A textbook of the diseases of cattle, horses, sheep, goats and pigs. 10th edition W.B. Saunders. London. Therapy for EIPH is controversial in that a wide variety of treatments are used but only one, furosemide, has demonstrated efficacy under conditions of racing (Table 29.2).47,48 There is evidence, based on studies of small numbers of horses running on a treadmill, of efficacy for a small number of other substances but care should be taken in extrapolating results of these studies to horses in the field. Conversely, failure to detect a beneficial effect of a compound or substance during testing using a small number of horses might be related to the low statistical power of the study rather than lack of efficacy.49,50 Table 29.2 Pharmacotherapeutic and management interventions used in an attempt to prevent exercise-induced pulmonary hemorrhage in horses
Exercise-induced pulmonary hemorrhage (EIPH)
Introduction
Exercise-induced pulmonary hemorrhage
Recognition
History and presenting complaint
Physical examination
Diagnostic tests
Tracheobronchoscopy
Examination of airway secretions or lavage fluid
Radiography
Exercise testing
Necropsy examination
Diagnostic confirmation
DISEASE
EPIDEMIOLOGY
CLINICAL SIGNS AND DIAGNOSIS
TREATMENT AND CONTROL
Epistaxis with hemorrhage into trachea or bronchi
Exercise-induced pulmonary hemorrhage
Horses after strenuous exercise. Most common in Thoroughbred and Standardbred racehorses
Epistaxis is a rare but very specific sign of EIPH. Only occurs after exercise. Endoscopic examination of the airways is diagnostic
Administration of furosemide. Rest – often enforced by regulations of the racing jurisdiction
Trauma
Sporadic. Associated with trauma to head, neck, or chest
Physical examination reveals site and nature of the trauma. Can require endoscopic examination of upper airways
Symptomatic treatment
Pneumonia
Recent shipping or respiratory disease. Can occur as outbreaks though usually individual animals
Fever, tachypnea, abnormal lung sounds, leukocytosis, radiography demonstrates lung lesions. Cytologic and microbiologic examination of tracheal aspirate
Antimicrobials, NSAIDs, oxygen. Control by vaccination and prevention of respiratory disease
Lung abscess
Sporadic. Hemorrhage can occur after exercise
Sometimes no premonitory signs. Fever, depression, anorexia, cough. Hemogram demonstrates leukocytosis. Hyperfibrinogenemia. Ultrasonography or radiography demonstrates lesion. Tracheal aspirates
Antibiotics
Intrabronchial foreign body
Sporadic
Cough, hemoptysis, fever. Endoscopy or radiography reveals foreign body
Removal of foreign body – often not readily achieved
Pulmonary neoplasia
Sporadic. Often older horse, but not always. Hemangiosarcoma
Cough, hemoptysis. Demonstrate mass on ultrasonographic or radiographic examination
None
Epistaxis without hemorrhage into trachea or bronchi
Guttural pouch mycosis
Sporadic. Acute-onset epistaxis
Severe, life-threatening epistaxis. Tachycardia, anemia, hemorrhagic shock
Surgical ligation or occlusion of arteries
Ethmoidal hematoma
Sporadic
Epistaxis not associated with exercise. Usually unilateral
Surgery or injection of mass with formaldehyde
Thrombocytopenia
Sporadic
Epistaxis, mild, intermittent. Petechiation and ecchymotic hemorrhages. Thrombocytopenia
Glucocorticoids or other immunosuppressive medications
Neoplasia
Sporadic
Neoplasia of upper airways
None
Trauma
Sporadic
Injury to head or pharynx
Symptomatic
Sinusitis
Sporadic
Endoscopic or radiographic examination of sinus
Drainage. Antimicrobials
Treatment and prognosis
Treatment
PUTATIVE MECHANISM AND CONTRIBUTING FACTOR
INTERVENTION
EVIDENCE OF EFFICACY
High pulmonary capillary pressure
High cardiac output
Furosemide
Dehydration
Other diuretics
Evidence of efficacy of furosemide in control of EIPH
Insufficient pulmonary vasodilation
Antihypertensive agents:
Guanabenz
Clonidine
No studies to investigate efficacy or effect on PAP
Enalapril
No effect on PAP during intense exercise
Nitric oxide donors/analogues:
Nitroglycerin
Nitroprusside
L-arginine
NG reduces PAP of standing horses. No evidence of effect on PAP during exercise No blockade by L-NAME does not affect PAP during intense exercise
Phosphodiesterase inhibitors:
Sildenafil (Viagra)
Aminophylline![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree

 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access