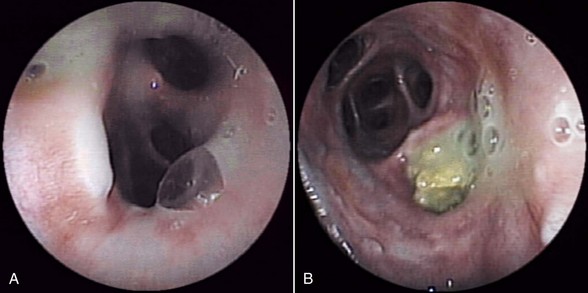
Chapter 163 Eosinophilic bronchopneumopathy (EBP) is a disease characterized by eosinophilic infiltration of the lung and bronchial mucosa. Several terms, including pulmonary infiltration with eosinophils, pulmonary eosinophilia, and eosinophilic pneumonia have been used in the literature to describe the same disease (Clercx et al, 2000). Possible causes include occult heartworm disease due to Dirofilaria immitis, migration of larvae of Angiostrongylus vasorum through pulmonary parenchyma, and infection with a parasite such as Oslerus osleri, Filaroides hirthi, Crenosoma vulpis, or Paragonimus kellicotti. Suspected but unconfirmed causes in dogs include allergic bronchopulmonary aspergillosis, chronic pulmonary infections caused by mycobacteria or fungi, drug reactions, and tumors (lymphoma and mast cell tumor). However, a specific cause is rarely identified even with extensive diagnostic workup, and most cases of EBP are considered to be idiopathic, although a hypersensitivity to aeroallergens is suspected. In idiopathic EBP, a dominant helper T cell type 2 (TH2) immune response is suspected, based on a selective increase in CD4+ T cells in bronchoalveolar lavage fluid (BALF) (Clercx et al, 2002) and increased levels of messenger RNA encoding for eotaxins, the strongest chemoattractants for eosinophils, in bronchial biopsy specimens from dogs with EBP (Peeters et al, 2006). The cause of these changes is unknown. A limited number of positive intradermal skin test reactions have been described in affected dogs; however, the relationship between positive intradermal skin test results and detection of aeroallergens responsible for EBP is still unclear. Lower airway and pulmonary destruction and remodeling observed in canine EBP may be connected to up-regulation of collagenolysis, related perhaps to increased activity of matrix metalloproteinase 8 (MMP-8), MMP-9, and MMP-13 (Rajamaki et al, 2002). Thoracic radiographs always show diffuse pulmonary lesions of variable intensity with a moderate to severe bronchointerstitial pattern. Peribronchial cuffing, marked thickening of the bronchial walls, alveolar infiltration, and bronchiectasis are other reported findings. Hematologic abnormalities include leukocytosis in up to half of cases, eosinophilia in up to 60%, neutrophilia in about 25%, and basophilia in up to 50% (Clercx et al, 2000). It is important to note that an absence of peripheral eosinophilia does not exclude a diagnosis of EBP. Serum biochemistry values are unremarkable. Bronchoscopy allows observation of macroscopic findings typical of EBP, such as the presence of a moderate to large amount of yellow-green secretions (Figure 163-1), moderate to severe thickening of the bronchial mucosa with an irregular to polypoid aspect, bronchiectasis, and possibly bronchomalacia in chronic cases. Eosinophils constitute the predominant inflammatory cell type seen on BALF smear cytology or brush cytology. Secondary bacterial infection is uncommon but should be recognized and treated promptly before treatment with glucocorticoids is initiated. Histopathologic examination of perendoscopic mucosal bronchial biopsy specimens also can reveal eosinophilic infiltrates. Figure 163-1 Endoscopic view of the bronchi of a 5-year-old female rottweiler with eosinophilic bronchopneumopathy showing a large amount of sticky yellow material (A) and bronchiectasis with the presence of almost solid material (B).
Eosinophilic Pulmonary Diseases
Definition and Causes
Pathogenesis
Diagnosis
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


