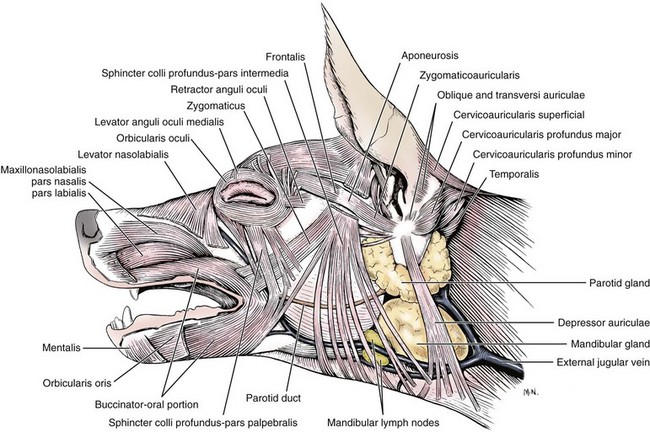
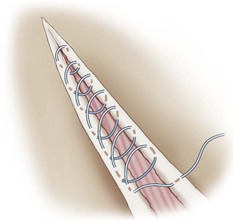
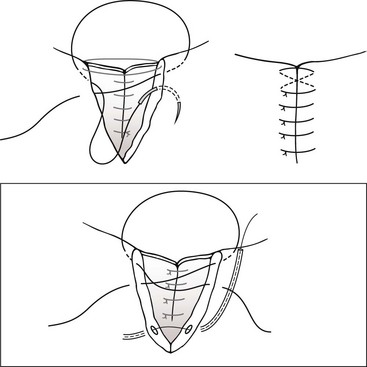
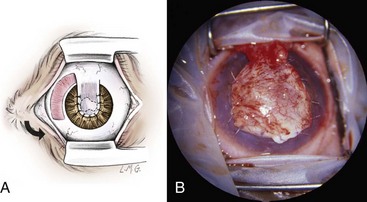
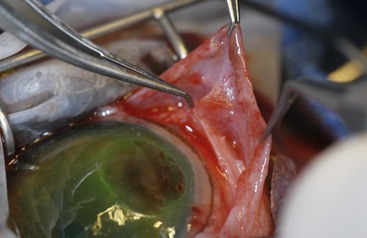
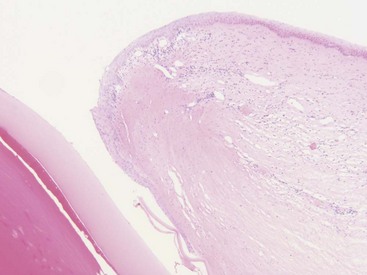
Chapter 125 Ophthalmic surgery often requires advanced training and special instrumentation. In some situations, however, referral may not be an option. This chapter covers emergency surgical procedures for the eye and adnexa. Information on anatomy, instrumentation, and basic surgery principles of the eye and surrounding structures is available in Chapter 124. Eyelid lacerations in small animals are generally associated with sharp trauma. Meticulous anatomic reapposition is necessary to enhance cosmesis and ensure proper postoperative eyelid function, which is necessary to maintain corneal health. The typical full-thickness eyelid laceration (including skin, muscle, fibrous tissue, and conjunctiva) is an L-shaped lesion that carries perpendicularly through the eyelid margin for 5 to 10 mm and then runs parallel to the eyelid margin for a variable distance (Figure 125-1). These wounds probably commence at the margin, with the perpendicular tear turning parallel as it meets the natural junctions between the pretarsal and preseptal sections or preseptal and preorbital sections of the orbicularis oculi muscle (Figure 125-2). Eyelid laceration treatment is based on the duration, type of wound, and likelihood of infection. Lacerations of several days’ duration that are associated with obvious signs of infection are best left to granulate after antiseptic flushing and appropriate antibiotic therapy. More acute lacerations with relatively clean margins and minimal discharge should be sutured as soon as possible to minimize tissue contracture and optimize eyelid margin–corneal relationships. This is particularly true of lesions that include the eyelid margin. The rich vascular supply of the eyelids provides fertile ground for rapid wound healing, but tissue handling and debridement are minimized to decrease microthrombus formation.27 If dangling pedicles of eyelid tissue are present, they should be maintained, as all but the most severely devitalized will survive because of the robust and redundant eyelid vasculature. The eyelid is composed of four surgical layers: the outer skin, subjacent muscular and fibrous layers, and inner palpebral conjunctiva. The skin and muscular layers constitute the anterior lamella, and the fibrous and conjunctival layers constitute the posterior lamella. Full-thickness wounds are best closed in two layers: a deep closure of muscle and fibrous tissue together followed by skin closure. Muscle and fibrous layers can be closed with 5-0 or 6-0 polyglactin 910 (Vicryl) or irradiated polyglactin 910 (Vicryl Rapide) in a variety of simple continuous approaches. The author’s preferred approach to the deep layer is to start just proximal to the eyelid margin, entering the muscle layer just beneath the skin. The bite is directed perpendicular to the eyelid and exits the wound just above the palpebral conjunctiva. It is imperative that the bite exits above the conjunctiva and does not actually penetrate it; exposure of suture material to the corneal surface could result in a postoperative suture-associated corneal erosion. The bite is then carried across the wound and enters the opposite side just above the conjunctiva. It is advanced perpendicular to the eyelid surface toward the skin and exits the muscle layer just beneath the skin. The knot is tightened securely within the interstitial tissue of the wound, and the process is repeated in a simple continuous fashion until the wound is closed (Figure 125-3). If the muscle and fibrous layers have been properly apposed, the skin will already be relatively well apposed, and final closure will be straightforward. The most important part of skin closure is the eyelid margin itself. Meticulous marginal apposition is the single best predictor of perfect postoperative eyelid function and corneal health. Many marginal closure techniques have been described;23,28,38 however, the easiest and most versatile is the figure of eight closure (Figure 125-4). The figure of eight, when properly executed, ensures perfect apposition and places the suture knot several millimeters away from the corneal surface. In this technique, 5-0 or 6-0 polyglactin 910 or irradiated polyglactin 910 is directed into the skin 4 mm proximal to the eyelid margin and 2 mm to one side of the wound. This bite exits the interstitial tissue of the wound edge and enters the interstitial tissue on the opposite side of the wound 2 mm proximal to the eyelid margin. The needle is then directed to exit the eyelid margin itself 1 mm away from the wound. The thread is pulled through, and the needle reenters the eyelid margin on the first side of the wound 1 mm away from the wound. This bite exits the interstitial tissue of the wound and reenters the interstitial tissue of the opposite side, at which point the needle is directed to exit the skin 4 mm proximal to the eyelid margin and 2 mm away from the wound. After this is accomplished, there should be a total of eight entry and exit sites of the needle, with four on each side of the wound. If the four on each side are mirror images of each other with respect to distances from the wound and the eyelid margin, then perfect apposition will result. In medial canthal lesions, especially those of the inferior eyelid, damage to the nasolacrimal puncta or canaliculi may occur. If the canaliculi are severed and not reapposed, chronic postoperative epiphora will result. Actual suturing of the canaliculi requires advanced microsurgical capabilities and is generally not necessary for a satisfactory outcome. If the puncta and sites of canaliculus severance can be identified, the canaliculus can be cannulated with 2-0 monofilament nylon suture material or silicone stent tubing (0.125 mm inner diameter; 0.250-mm outer diameter) before completing the two-layer closure as described above (see Figure 125-4). The cannula is preferably advanced out the nostril and anchored to the skin near the medial canthus proximally and near the nares distally. It should be left in place for 2 to 4 months. During that time, the torn edges of the canaliculus will reconnect, allowing for proper nasolacrimal drainage.27 Lacerations of the bulbar or third eyelid conjunctiva generally do not require suturing because they often heal quickly by second intention.3 Lesions involving the margin of the third eyelid or resulting in exposure of the third eyelid cartilage may benefit from closure with simple interrupted sutures of 6-0 or 7-0 polyglactin 910 to prevent corneal damage. Rapidly deepening corneal ulcers can result in corneal perforation quite quickly and should thus be considered true emergency situations (Figure 125-5). A number of pharmacologic approaches may be used to retard the activity of the matrix metalloproteinase and serine protease enzymes that degrade the corneal stroma, but these therapies do not improve the tectonic stability of weakened corneas.7,30 Surgical therapy is usually advocated to diminish matrix metalloproteinase activity, provide immediate structural support, and allow for proper corneal reconstruction. The most useful surgical approaches involve some variation of either autografting or allografting. The most widely used autograft in veterinary ophthalmology is the bulbar conjunctival graft, also referred to as Gunderson’s graft, in which a portion of the bulbar conjunctiva is harvested and transposed to the ulcerated area.14 Most of these grafts are actually flaps and thus are designed to maintain a patent conjunctival blood supply, which provides a constant infusion of the matrix metalloproteinase and serine protease inhibitor α2-macroglobulin and the serine protease inhibitor α1-antitrypsin. In addition, structural support is provided by conjunctival epithelium and its subjacent collagenous stroma.7,9 Pedicle Graft: There are several variations on the basic conjunctival grafting theme, with the most versatile being the rotational conjunctival pedicle or “racquet” graft or flap (Figure 125-6).10,16,17,29 The animal is ideally positioned in dorsal recumbency with the neck slightly ventroflexed and turned slightly away from the affected side. This should put a plane tangential to the corneal axis parallel to the floor. Before surgery, samples are obtained for corneal cytology and bacterial culture and sensitivity. Proper planning of the graft is essential. The superotemporal bulbar conjunctiva is the easiest to harvest, and a lateral canthotomy improves exposure tremendously. The distal end of the graft should extend just ventral to the inferior edge of the ulcer; the pedicle arm must be long enough to easily reach from the hinge region to the distal edge of the ulcer without being stretched too tightly. The pedicle arm should be 3 mm wider than the ulcer to allow for tissue contracture. The surgeon should bear in mind that after preparation of the ulcer bed (see below), ulcer size may increase, so the pedicle width may need to be wider than originally expected. The incision for development of a rotational pedicle graft begins 1 mm temporal to the limbus at a position tangential to the inferior edge of the ulcer and is continued perpendicular to the limbus (see Figure 125-6, A). The incision is made by lifting the conjunctiva with Colibri forceps; multiple small snips are made with strabismus scissors until the incision is 3 mm longer than the ulcer is wide. The scissors are then introduced into the resulting pocket and directed toward the hinge region while bluntly dissecting Tenon’s capsule away from the underside of the conjunctiva. A second incision is then made with strabismus scissors from the temporal extent of the first incision superiorly and parallel to the limbus. This second incision continues to a point level with a vertical tangent to the temporal edge of the ulcer. Any remaining Tenon’s capsule is now dissected away (Figure 125-7). Finally, a third incision begins at the nasal extent of the first incision and is carried superiorly parallel to the limbus to a point level with a vertical tangent to the nasal edge of the ulcer. The second and third incisions are therefore staggered to create a broad hinge with ample blood supply that will not kink when the pedicle is rotated over the ulcer. At this point, any remaining Tenon’s capsule attached to the pedicle is removed. It is imperative that as much of the remaining Tenon’s capsule as possible is gingerly dissected from the underside of the graft to reduce tension on the graft and postoperative contracture by Tenon’s fibroblasts, both of which are risk factors for graft dehiscence.14 Preparation of the ulcer bed is crucial to graft success. The ulcer bed, including the stromal walls and Descemet’s membrane, should be gently swabbed with cellulose sponges or a 6400 Beaver blade to ensure that it is free of corneal epithelium. This will improve the chance of adherence of the graft to the lesion. If the ulcer is actively melting, soft ulcer edges should be trimmed out to good cornea that will hold sutures. Before suturing, the graft is rotated into position and laid atop the ulcer; it should easily remain in place without being stretched. If it is too taut, the second and third incisions should be extended to relax the graft. It is important to make sure the pedicle is not twisted as it is rotated; when in its final position, the stromal side of the pedicle should face in toward the anterior chamber, and the epithelial side should face out. The preferred suture is either 7-0 or 8-0 polyglactin 910 placed in a simple interrupted pattern. The first suture should be placed at the 6 o’clock position, with additional sutures every 1.5 to 2 mm along the temporal and nasal edges of the ulcer. To avoid compromising the blood flow, sutures are not placed through the portion of the pedicle arm superior to the ulcer. However, if the ulcer is leaking aqueous humor, one or two sutures should be placed through the pedicle arm and into the superior edge of the ulcer, passing sutures parallel to the pedicle arm to minimize negative effects on blood supply. Sutures should be placed so that the edge of the pedicle abuts the edge of the ulcer without “overriding” onto normal cornea. Otherwise, normal corneal epithelium may proliferate beneath the graft, preventing its adherence (Figure 125-8). After suturing the graft in place, the bare sclera left in the donor site can be covered with adjacent conjunctiva using 6-0 or 7-0 polyglactin 910 in a simple continuous pattern to appose the edges. The donor site for particularly wide pedicles may be too large to cover without placing undue strain on the conjunctiva. In this instance, the scleral bed can be left to heal by second intention. It is the author’s impression that animals with open scleral beds are more painful compared with those in which the bare sclera is covered. In brachycephalic animals, a partial temporary tarsorrhaphy is placed and left up for 1 to 2 weeks to reduce tension exerted by the physiologic exophthalmia.
Emergency Ophthalmic Surgery
Adenexa
Nasolacrimal Lacerations
Conjunctival and Third Eyelid Lacerations
Corneal Reconstruction
Autografts
< div class='tao-gold-member'>
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Emergency Ophthalmic Surgery
Only gold members can continue reading. Log In or Register to continue