Chapter 14 Dysrhythmias
cardiac pacing and electrical cardioversion
INTRODUCTION
Cardiac cells, due to their excitable properties, are capable of being depolarized by an external stimulus such as an electrical pulse. Such depolarization will only occur if the external stimulus has sufficient strength to reach the threshold for stimulation and provided that the stimulus is not delivered while the cell is in a refractory period.1,2 As atria and ventricles act as a pseudosyncytium, depolarization of a few atrial or ventricular cells leads to depolarization of the whole atrium or ventricle, respectively. As such, by delivering electrical stimuli at a precise location in or around the heart, one can selectively induce atrial or ventricular contractions at a specific rate and this is called atrial or ventricular pacing. Certain pacing techniques can be performed in the standing, unsedated horse without being sensed as the required electrical stimuli are of relatively low intensity.
CARDIAC PACING
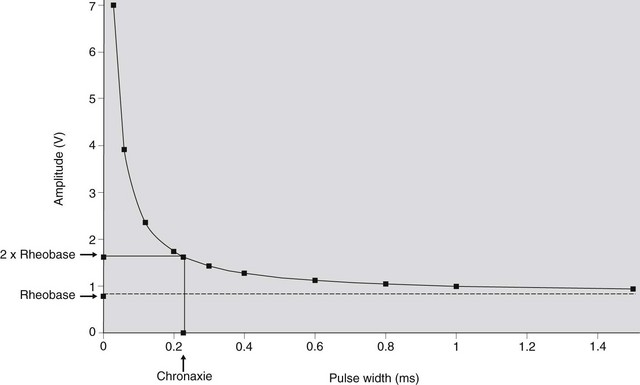
During pacing, current pulses with specific amplitude, duration and interval are transmitted to the atrium or ventricle via appropriately positioned electrodes. Only when the current is able to reduce the resting potential of the cardiac cell by a critical amount and within a critical time, will “capture” be achieved, which means that a depolarization of that chamber will follow. The intensity of the electrical pulse required to reach the threshold for stimulation is determined mainly by the position of the electrodes in relation to the heart. This intensity is expressed by the pacing amplitude (strength, V) and the pulse width (duration, ms) of the electrical stimulus. A stimulus that is large in amplitude requires a shorter duration to reach threshold, and vice versa. At a given pulse duration, the corresponding threshold amplitude can be easily determined by the stimulus reduction method. With a fixed pulse duration, pacing is started at a high amplitude, which results in consistent capture. Every few beats the amplitude is gradually reduced until, finally, capture is lost. The lowest amplitude resulting in capture represents the threshold value for that pulse duration. Similarly, the threshold pulse duration can be determined for a fixed pulse amplitude. Threshold values describe a hyperbolic-like strength-duration curve (Fig. 14.1), which is a means of verifying that a given electrode position is likely to achieve safe and effective cardiac pacing.2 Two important features of the strength-duration curve are the rheobase and chronaxie. The rheobase is the lowest voltage that results in capture at “infinitely” long pulse duration (usually less than 1.5 ms). The chronaxie is the required pulse width when pacing at two times the rheobase voltage. When two random points of the strength-duration curve are determined, the rheobase, the chronaxie and the remaining points of the curve can be calculated using the following equation3:
It is critical that a stimulus is not delivered near the end of the refractory period, i.e. the “vulnerable” period, because this might initiate fibrillation4 and is extremely dangerous in case of ventricular stimulation. For this reason, most pulse generators (pacemakers) are able to “sense” each cardiac depolarization, thereby temporarily inhibiting the pacing function.
ELECTRODES
An electrical current flows between two electrodes, the cathode and the anode. The number of electrodes in contact with or close to the heart determines whether unipolar or bipolar pacing is performed. The electrode nearest to the myocardium should be the cathode (negative) because cathodal stimulation is less likely to induce arrhythmias.5 For unipolar pacing, one electrode, the cathode, is in contact with the heart while the second electrode is at a remote site of the heart. In case of bipolar pacing, cathode and anode are, within a short distance of each other, in contact with the heart. Unipolar pacing results in a much larger pacing artifact on the surface ECG and is more likely to induce skeletal muscle stimulation (near the anode) than bipolar pacing. Finally, recording an intracardiac ECG through a unipolar lead is more susceptible to muscle potential artifacts than bipolar recordings.
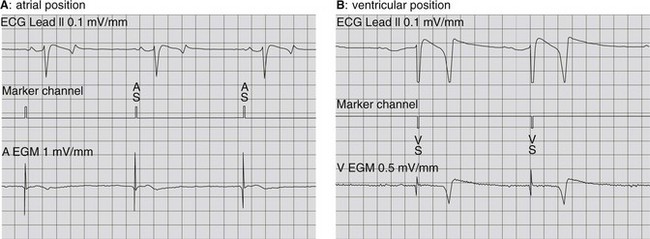
The most suitable and safest approach for atrial and ventricular pacing in horses utilizes a lead or catheter with electrodes on its tip, inserted transvenously and positioned in the respective right cardiac chambers, to allow stimulation of the endomyocardium.6 Due to the close contact between electrode and myocardium, a minimal amount of energy, usually between 0.5 and 7.5 V and 0.3 and 1.2 ms, is sufficient to achieve consistent capture. Therefore, pacing will not be sensed by the patient. Positioning of the electrode is guided by fluoroscopy and echocardiography. In addition, the electrode position is verified by recording the intracavitary electrogram from the lead simultaneously with a surface ECG.6 During transvenous insertion of the lead the intracavitary electrogram will successively show: (1) no or minimal deflections during passage through the vein, (2) a deflection simultaneous with the P wave from the surface ECG during right atrial positioning (Fig. 14.2A) and (3) a deflection simultaneous with the QRS complex when located in the right ventricle (see Fig. 14.2B). Additionally, electrode position is verified by connecting the lead with a pacing device and applying testing stimuli of sufficient strength. An intravenous position will not result in capture, while an atrial or ventricular position will produce a P wave or QRS complex, respectively.
THERAPEUTIC USE OF PACING
Permanent pacing
Bradydysrhythmias such as third-degree AV block and sick sinus syndrome are the major indications for permanent pacing, requiring implantation of an artificial pacemaker.7 The pacemaker is a multi-programmable and implantable battery-powered pacing device. It is connected with one or more leads towards the right atrium or ventricle (single chamber pacemaker) or towards both (dual chamber pacemaker) to stimulate a specific chamber at a specific rate (e.g. 35 bpm) so that symptomatic bradycardia is avoided. However, because an intrinsic atrial and/or ventricular rhythm might still be present, pacemakers have the ability to sense this intrinsic rate via the implanted leads and can be programmed to respond in a specific way to an intrinsic beat. Besides the treatment of bradydysrhythmias, in humans, pacemaker implantation is also used to prevent induction of certain tachydysrhythmias.8 However, this technique has never been used in horses.
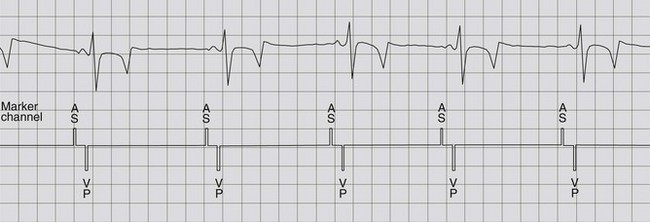
Depending on the kind of dysrhythmia, different types of pacemakers can be applied. If the cause of bradycardia is a depressed or absent AV node conduction, a “simple”, single chamber (ventricular) pacemaker can be implanted. When this pacemaker is programmed to the VVI mode, with a minimal ventricular rate of, for example, 35 beats per minute, syncope will be prevented by preserving this minimal heart rate. However, no adaptation of heart rate to the physical needs (e.g. exercise) will occur. Rate-modulation, for example, based upon an activity sensor, is achieved with a VVIR pacemaker. However, much more efficient in case of a third-degree AV block, is to implant a dual chamber pacemaker. Such a pacemaker can be programmed to prevent a too slow atrial and ventricular rate but also to “look for” (sense) an intrinsic atrial depolarisation and to deliver (trigger) a ventricular stimulus for each sensed atrial signal, which is achieved in the DDD function (Fig. 14.3). As sinus node function in an animal with third-degree AV block is usually intact, a fairly normal paced ventricular rate, which adapts with stress or exercise, can then be obtained. If bradycardia is caused by an abnormal sinus node function, adaptation of pacing rate with exercise can only be achieved by using a pacemaker with an incorporated sensor (e.g. VVIR, DDIR).
In horses, both epicardial and transvenous lead placement has been described. The epicardial lead placement requires general anaesthesia and thoracotomy, which implies a risk, especially in an animal with a compromised cardiovascular system.9,10 This method has successfully been applied in a healthy pony and in two donkeys with third-degree AV block for implantation of a single chamber or dual chamber pacemaker.11,12,13 The pacemaker device was inserted underneath the pectoral muscle or, subcutaneously, caudal to the left elbow. In the donkeys, successful pacing was obtained for 6 weeks in one and more than 1 year in the other. During an attempt to place an epicardial lead in a mature horse with third-degree AV block, the horse developed ventricular fibrillation during general anaesthesia and died.14
Transvenous lead placement is a much safer and simpler procedure to achieve cardiac pacing and is widely used in human and small animal medicine. It requires a vein that is located relatively close to the heart (maximal lead length is around 110 cm), that is large enough to introduce one or two leads and that can be ligated permanently. A standardized approach has been described to implant a dual chamber pacemaker via the cephalic vein.6 As the whole procedure can be performed in the standing, sedated horse, the additional risk of anaesthesia can be avoided. During the implantation procedure, an atrial and a ventricular active fixation lead are inserted through a surgically exposed cephalic vein. Lead placement is guided by both echocardiography and by measuring the electrical characteristics of the lead. After permanent ligation of the vein a pacemaker pocket is created between the lateral pectoral groove and the manubrium sterni. Successful clinical application of transvenous lead placement was first reported by Reef et al.,15 implanting a single chamber (ventricular) pacemaker in a horse with third-degree AV block. Under general anaesthesia, a passive fixation lead was inserted in the jugular vein and placed in the right ventricular apex under echocardiographic guidance. The pacemaker pocket was created dorsal to the jugular vein. Although the horse remained asymptomatic, 16 months later, a second lead with active fixation was implanted in the right atrium and the pacemaker was updated to a dual chamber model, allowing AV sequential pacing of the ventricles. Consequently, a physiological rate response to exercise and stress occurred. With the dual chamber pacemaker the horse was able to perform exercise with a maximal achievable heart rate of 150 beats per minute. About 3 years after the initial implantation, however, the horse suddenly died due to a suppurative endocarditis and suspected terminal bacteraemia.16 Implantation of a dual chamber rate-adaptive pacemaker has also been used in a horse with post-exercise bradycardia and syncope due to sinus node dysfunction.17 At 7-year follow-up, proper dual chamber pacing was still achieved.
Temporary pacing
A transvenously inserted catheter, electrode or lead within the right atrium or right ventricle can directly stimulate the endomyocardium, requiring only low pulse intensity, and is a safe and effective means to obtain consistent cardiac pacing. As the pacing stimuli are not sensed by the horse the technique can be used without sedation or anaesthesia. Temporary transvenous pacing has been used in horses with symptomatic bradycardia to avoid syncope prior to the permanent implantation of a pacemaker.13–15,17,18 Transvenous temporary pacing has also been used to treat transient asystole following electrical cardioversion of atrial fibrillation (AF) in a horse.19
In human beings, temporary pacing is also used to terminate tachydysrhythmias such as atrial flutter, AV node tachycardia and sustained ventricular tachycardia.7 During such a transvenous overdrive pacing procedure, a train of electrical pulses is repeatedly given at a fixed rate in excess of the basic natural rhythm. The purpose is to entrain and interrupt the tachydysrhythmia by depolarizing regions of the excitable gap of the re-entry cycle.8,20 This technique has been successfully applied in a horse with persistent, medically resistant atrial flutter.21 In this horse, right atrial pacing at a rate slightly higher (300 ms cycle length) than the atrial flutter rate (365 ms cycle length) terminated the re-entry phenomenon and re-established sinus rhythm. The procedure was performed in the standing unsedated horse and was well tolerated. However, because overdrive pacing can accelerate tachycardia and result in fibrillation, the technique is not recommended for ventricular tachycardia in horses.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree