Drugs Used in Respiratory System Disorders
Learning Objectives
After studying this chapter, you should be able to
1. Describe the basic anatomy and physiology of the respiratory system.
2. List the protective mechanisms of the respiratory system.
3. Describe the fundamental principles of treatment of the respiratory system.
4. List the differences between the actions of expectorants, antitussives, and mucolytics.
5. Describe the action of bronchodilators.
6. Describe the use of antihistamines and decongestants in respiratory disease.
7. List potential uses for respiratory stimulants.
8. List the advantages and disadvantages of inhalant therapy.
Key Terms
Aerosolization
Antitussive
Bronchoconstriction
Bronchodilation
Decongestant
Expectorant
Humidification
IgA
Inspissated
Mucolytic
Nebulization
Nonproductive cough
Productive cough
Reverse sneeze
Surfactant
Viscid
Introduction
Veterinary references list a wide variety of diseases of the respiratory system. A partial listing of general origins includes the following:
The respiratory system has a series of defense mechanisms by which it protects itself from disease. These natural defenses can be damaged by management practices such as those that cause a buildup of ammonia in enclosed, poorly ventilated housing. They can also be suppressed by inappropriate therapy, such as the use of cough suppressants for a productive cough. Because it is essential that these defense mechanisms function optimally for prompt recovery from respiratory disease, it is very important that technicians have a basic understanding of respiratory anatomy and physiology, respiratory defense mechanisms, and respiratory therapeutics.
Respiratory Anatomy and Physiology
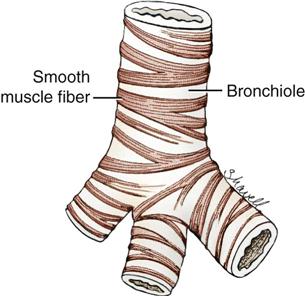
The respiratory system consists of the lungs and the passageways that carry air to and from the lungs (Figure 5-1). These passageways include the nostrils, nasal cavity, pharynx, larynx, trachea, bronchi, and bronchioles.
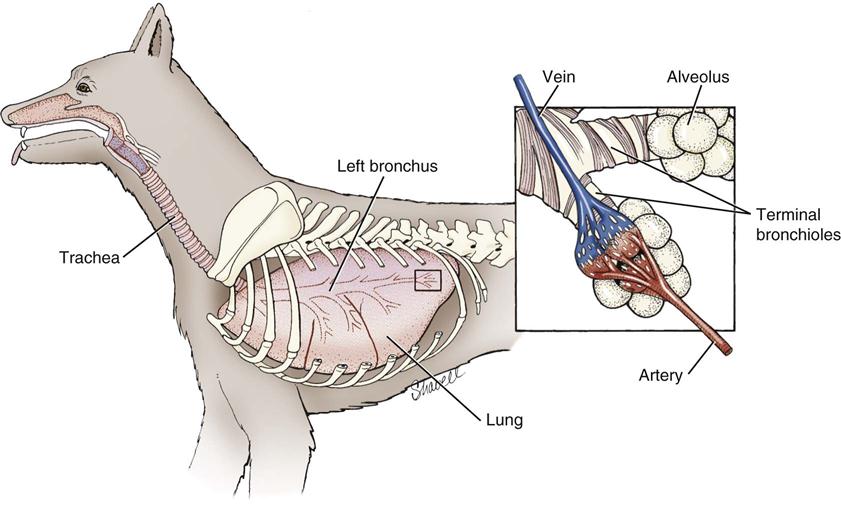
The passageways that lead to the lungs are referred to as the upper respiratory system. The upper respiratory system begins with the nostrils, which open into the nasal cavity. The nasal cavity contains turbinates that are covered with mucous membranes. These turbinates increase the surface area of the nasal cavity to allow humidification and warming of inspired air. Air that passes out of the nasal cavity moves, in turn, through the pharynx and the larynx into the trachea. The trachea bifurcates into right and left bronchi, which lead to right and left lungs, respectively. Each bronchus then divides into a series of passageways of decreasing size, called bronchioles. Smooth muscle fibers are found in the walls of the bronchioles. Contraction of smooth muscle fibers decreases the diameter of the bronchioles, and relaxation of fibers allows the diameter to return to normal size (Figure 5-2).
The upper respiratory tract is lined with ciliated, pseudostratified columnar epithelial cells. Interspersed between the epithelial cells are goblet cells capable of secreting mucus. Mucus is secreted onto the surface of the epithelial cells and is moved toward the pharynx by movement of the cilia (mucociliary apparatus).
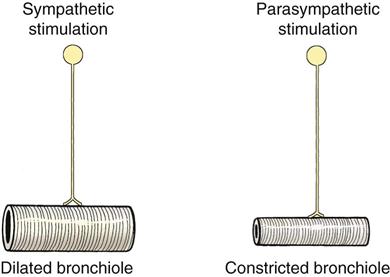
Sympathetic stimulation results in decreased production of mucus by the goblet cells and relaxation of smooth muscle in the walls of the bronchioles, leading to bronchodilation.
Parasympathetic stimulation causes increased secretion of mucus and constriction of smooth muscle (bronchoconstriction) (Figure 5-3).
The bronchioles terminate in small, saclike structures called alveoli. The alveoli are arranged in grapelike clusters and are lined with a chemical substance called surfactant, which reduces the surface tension of the alveoli and helps to keep them from collapsing. The alveoli are surrounded by capillaries; this makes it possible for the blood to unload its carbon dioxide into the alveoli and to pick up oxygen from the alveoli.
Functions that the respiratory system serves include the following:
The work of the respiratory system can be divided into the following four parts:
1. Ventilation—movement of air into and out of the lungs. The inspiratory portion of ventilation is usually an active process, whereas expiration is usually a passive process. Forced inspiration may be associated with upper airway obstruction, and active expiration may be related to intrathoracic airway obstruction (Tilley and Smith, 2000).
2. Distribution—distributing of inspired gases throughout the lungs.
3. Diffusion—movement of gases across the alveolar membrane.
Respiratory Defense Mechanisms
The respiratory system has several effective methods of defense against disease processes, including the following:
Principles of Respiratory Therapeutics
It is important that a specific diagnosis be made through radiology, cytology, or appropriate culture before treatment of respiratory disease is initiated because the correct treatment for one type of disease may be contraindicated for another. Once the diagnosis has been made, treatment for respiratory disease is divided into the following three general goals (McKiernan, 1988):
Inhalation Therapy for Respiratory Disease
Although drugs used to treat respiratory disease are often administered by the oral or parenteral route, inhalation therapy may also be useful. Aerosolization (nebulization) of drugs allows their delivery at high concentrations directly into the airways while minimizing their blood levels—a feature that may reduce the chance of a toxic reaction. The efficacy of an inhaled drug depends on the dose and on how well it is distributed in the lungs. Distribution of an aerosol depends on several factors such as the size, shape, and pattern of the airways and the breathing pattern of the animal. The size of the inhaled particle plays a significant role in its distribution. The optimum particle size for entry into the peripheral airways is 1 to 5 microns (Lavoie, 2001). Particles smaller than 0.5 micron are likely to be exhaled, and those larger than 5 microns could be deposited in the upper airways. Airway pathology (e.g., excessive mucus or exudate) can interfere with distribution of the drug, causing some clinicians to assert that inhalation therapy should always be accompanied by systemic treatment (Boothe, 2012). Concurrent use of a bronchodilator and/or a mucolytic may be a helpful adjunct to inhalation therapy.
Two basic types of aerosol delivery systems are available for inhalation therapy: nebulizers and metered dose inhalers (MDI). Generally, nebulizers produce and deliver smaller particles that reach deep into the respiratory system whereas MDIs deliver particles to the upper airways. Nebulizers use compressors to create an aerosol that can be inhaled without the necessity of using positive pressure to force the aerosol into the airways. Nebulizers produce the aerosol using a jet or ultrasonic mechanism. In jet nebulizers, compressed air or oxygen is forced through a small orifice to create the aerosol. Drugs in solution are drawn from a fluid reservoir and shattered into droplets by the gas stream. Ultrasonic nebulizers use high-frequency vibrations from a piezoelectric crystal to create the aerosol. Ultrasonic nebulizers are more efficient at creating smaller aerosol droplets and are gentler on drug molecules than the jet nebulizers. Aerosolized drugs can be delivered to cats and dogs in a tentlike structure, closed container, or face mask, but a tight fitting face mask, endotracheal tube, or tracheostomy tube probably delivers the most efficient concentration of the drug to the patient (Reinero and Selting, 2013). Nebulizers must be kept meticulously clean to avoid iatrogenic infection of a patient already compromised with an airway pathology. Small inexpensive nebulizers are available for adaption for veterinary use (Omron) (Figure 5-4).

MDIs are designed for home use by animal owners. The aerosol of an MDI is driven by a propellant. Older MDIs used chlorofluorocarbons (CFCs) as the propellant, but CFCs are being replaced by hydrofluoroalkanes (HFAs), which contain no chlorine and do not affect the ozone. HFA propellants allow drugs to be delivered as a solution rather than a microsuspension, which, in turn, allows the production of a smaller particle that can reach deeper in the airways (Boothe, 2012). The use of spacers and holding chambers with the MDIs makes delivery to the patient more efficient and directed.
Clinical Uses
Nebulizers have been used primarily in the treatment of respiratory infections. Nebulizers are used to provide airway humidification (saline), mucolytics, bronchodilators, and antimicrobials. Mucolytics and saline can help treat pneumonia and other airway infections by decreasing the viscosity of airway secretions and improving their clearance from the airway. Bronchodilators increase flow through the airways, and antimicrobials counter infectious agents. A potential use of nebulizer therapy may be for inhaled chemotherapy, which would take advantage of the concept that high doses of the agents may be delivered to the lung while avoiding the potential side effects of intravenous use.
MDI therapy has been used primarily for feline lower airway disease (asthma), lower airway disease in horses (heaves or recurrent airway obstruction [RAO]), and, occasionally, in lower airway disease (bronchitis) in dogs. MDIs frequently contain bronchodilators like albuterol or clenbuterol and/or corticosteroids.
Box 5-1 lists drugs frequently used in inhalation therapy.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree