Drugs Used in Renal and Urinary Tract Disorders
Learning Objectives
After studying this chapter, you should be able to
1. Identify the anatomic features of the urinary system.
3. Compare the different classes of drugs and describe the indications for each class.
Key Terms
Agonist
Antagonist
Atony
Catecholamine
Detrusor
Detrusor areflexia
Erythropoiesis
Erythropoietin
Hematuria
Hypertension
Hypertonus
Hypokalemia
Lower motor neurons
Nephrology
Nephron
Polydipsia
Polyuria
Retroperitoneal
Upper motor neurons
Uremia
Urinary incontinence
Urinary tract infection
Introduction
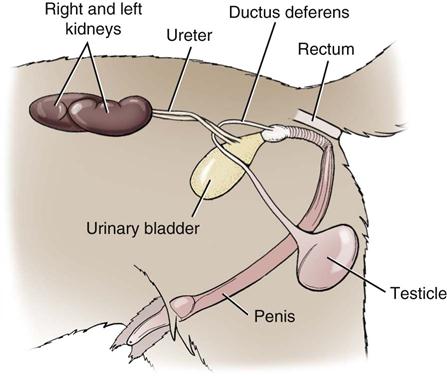
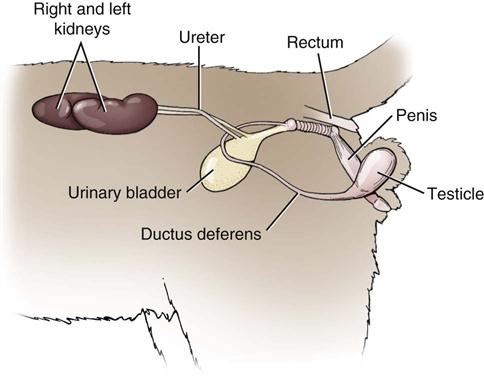
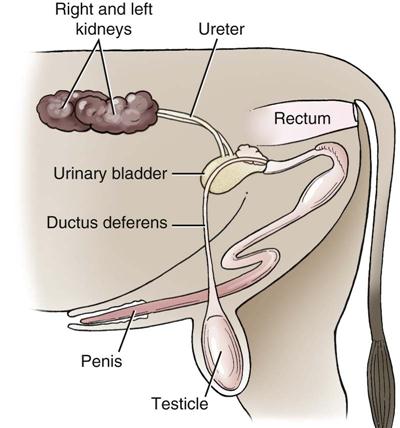
The urinary system (i.e., the renal system) is composed of two kidneys, two ureters, a urinary bladder, and a urethra (Figures 6-1 to 6-4). The medical study of the renal system is known as nephrology because the basic functional unit of the kidney is the nephron. The kidneys work in the body similar to the way in which a fish aquarium filter works. All the water in an aquarium is sent through the filter to capture waste products in the water so that the tank is kept clean. Thus, the kidneys filter all waste products from the bloodstream but allow those elements needed by the body to remain. The kidneys are bean shaped and lie on each side of the spine. They are also retroperitoneal.
The job of the nephron is to regulate water and soluble matter (especially electrolytes) in the body. Nephrons filter the blood under pressure and then reabsorb necessary fluid and molecules back into the blood. The kidneys thus excrete a variety of waste products produced by metabolism such as urea, uric acid, and water. The kidneys are involved in factors of homeostasis such as acid–base balance, regulation of electrolyte concentrations, blood volume control, and regulation of blood pressure. The kidneys communicate with other organs in the body through hormones that are secreted into the bloodstream.
Veterinary technicians should educate clients about the importance of nutrition, especially in those dog breeds predisposed to developing urinary bladder stones (e.g., dalmatians, miniature schnauzers). Fresh water should be available for animals at all times. Companion animals observed straining to urinate or with bloody urine (i.e., hematuria) should be brought to the veterinary hospital immediately.
Physiologic Principles
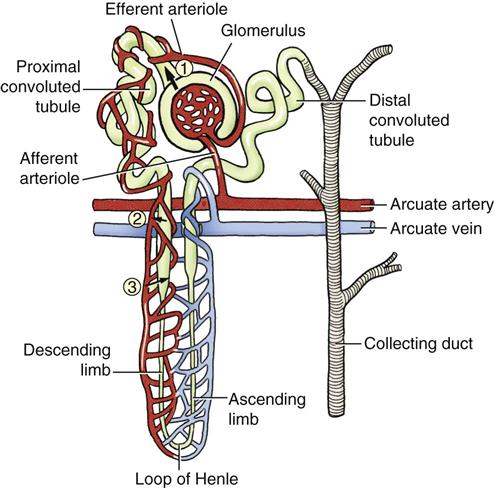
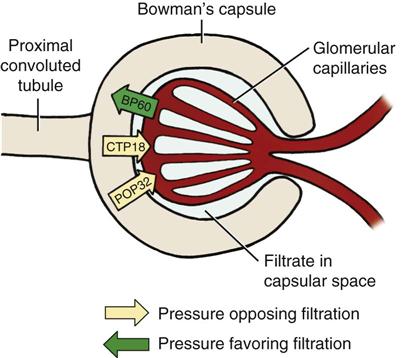
The formation of urine is a rather complex process that involves glomerular filtration, tubular reabsorption, and tubular secretion (Figure 6-5). The glomerular filtrate is composed of water and dissolved substances, which pass from the plasma into the glomerular capsule. The formation of glomerular filtrate is controlled by effective filtration pressure (EFP = arterial blood pressure – [plasma osmotic pressure + capsule pressure]). The amount of glomerular filtrate is directly proportional to the EFP (Figure 6-6). Changes in blood flow through the glomerulus, glomerular blood pressure, plasma osmotic pressure, and capsule pressure affect glomerular filtration.
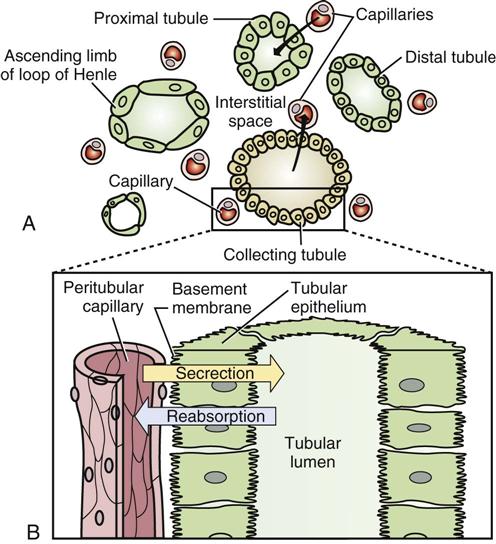
The kidney tubules are responsible for the reabsorption or the secretion of specific substances. Substances needed by the body are reabsorbed from the filtrate, pass through the tubular cell wall, and reenter the plasma. This process filters needed substances and returns them to the body. Reabsorbed materials include water, glucose, amino acids, urea, and ions such as Na, K, Ca2+, Cl−, HCO3−, and HPO42−. Any excess of these substances or of substances that are not useful remain in the filtrate and are excreted in the urine.
Tubular secretion occurs when substances are carried to the tubular lumen. This involves the active transport of certain endogenous substances and many exogenous substances. These secreted substances include potassium and hydrogen ions, ammonia, creatinine, and some drugs. The main effects of tubular secretion are to rid the body of certain materials and to help control blood pH (Figure 6-7). The kidneys are active in the metabolism and excretion of many drugs and their metabolites. Therefore, it is very important to remember that these actions may be inhibited in cases of renal failure or dysfunction. Drug therapy in animals with renal dysfunction has increased risks. Renal failure can impair a drug’s absorption from an administration site, affect a drug’s distribution in the body, and affect the elimination of the drug from the body.
If the kidneys’ functionality is decreased, erythropoiesis may not occur correctly. Erythropoiesis is the formation of erythrocytes. Erythropoietin is a hormone secreted by the healthy kidney that communicates with the bone marrow to make more red blood cells. In diseased kidneys, this hormone is secreted in reduced amounts or not at all, and the animal may develop a nonregenerative anemia as a result. Injections of human recombinant erythropoietin may be given to animals to treat this anemia.
Uremia can increase the sensitivity of some tissues to certain drugs. For example, sensitivity to central nervous system depressants is increased; therefore the dose of opiates, barbiturates, and tranquilizers should be reduced in uremic patients. Xylazine (Rompun) and ketamine hydrochloride (Ketaset) are contraindicated in uremic patients. Impaired renal excretion or biotransformation causes delayed elimination of many drugs and enhances their toxicity and duration of action.
Box 6-1 lists drugs that commonly require dosage modification in renal insufficiency. Modifications can be made by measuring the plasma concentration of a drug and adjusting the dose accordingly. However, this is impractical in most clinical settings, so a veterinarian may use the normal dose but lengthen the time intervals at which it is administered or give a smaller dose at normal time intervals. Technicians may be responsible for administering anesthesia, and it is important to remember that patients with renal failure are at greater anesthetic risk and require even closer monitoring than patients with normal renal function.
Renal Failure
Renal failure is among the major causes of nonaccidental death in dogs and cats. Although the disease is most common in older animals, it may be diagnosed in younger animals. Renal damage may stem from many causes including: infectious disease, diabetes mellitus, toxins, neoplasia, congenital disorders, immunologic problems, and amyloidosis. Diets with excessive protein, phosphorus, and sodium are other factors that may cause renal damage. Renal damage may be categorized as prerenal, renal, or postrenal. Renal failure may be differentiated as acute, chronic, or end-stage, according to parameters common to each stage.
Drugs Commonly Used for the Treatment of Renal Dysfunction and Associated Hypertension
 Diuretic Drugs
Diuretic Drugs
Diuretics are drugs used to remove excess extracellular fluid by increasing urine flow and sodium excretion and by reducing hypertension. A number of conditions may indicate the need for a diuretic drug. Classifications of commonly used diuretics include loop diuretics, osmotic diuretics, thiazide and thiazide-like diuretics, potassium-sparing diuretics, and carbonic anhydrase inhibitors.
Loop Diuretics
Loop diuretics are highly potent diuretics that inhibit the tubular reabsorption of sodium. Once these drugs are administered, their actions are generally rapid. Additionally, loop diuretics promote the excretion of chloride, potassium, and water. Some patients receiving long-term loop diuretic therapy may also need potassium supplementation.
Clinical Uses
Loop diuretics are useful in the treatment of congestive heart failure (CHF) in canines and felines, pulmonary edema, udder edema, hypercalcemic nephropathy, and uremia, as an adjunct in the treatment of hyperkalemia, and sometimes as an antihypertensive agent (Plumb, 2011).
Dosage Forms
Adverse Side Effects
These include hypokalemia (because of the increased excretion of potassium), other fluid and electrolyte abnormalities, ototoxicity, gastrointestinal distress, hematologic effects, weakness, and restlessness (Plumb, 2011).
Osmotic Diuretics
Osmotic diuretics can be administered intravenously to promote diuresis by exerting high osmotic pressure in the kidney tubules and limiting tubular reabsorption. Water is drawn into the glomerular filtrate, which reduces its reabsorption rate and increases the excretion of water. These drugs may be used to treat oliguric acute renal failure and to reduce intracranial pressure.
Clinical Uses
These drugs are used for oliguric renal failure, reduction of intraocular and cerebrospinal fluid (intracerebral) pressure, and rapid reduction of edema or ascites (Plumb, 2011).
Dosage Forms
Adverse Side Effects
These drugs should not be used in patients with anuria secondary to renal disease, in patients that are severely dehydrated, or in patients with pulmonary congestion or edema. Osmotic diuretics may cause fluid and electrolyte imbalances (Plumb, 2011).
Thiazide Diuretics
Thiazide diuretics reduce edema by inhibiting reabsorption of sodium, chloride, and water. Their duration of action is longer than that of loop diuretics.
Dosage Forms
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree