Drugs Used in Cardiovascular System Disorders
Learning Objectives
After studying this chapter, you should be able to
1. Describe the basic anatomy and physiology of the cardiovascular system.
2. List four compensatory mechanisms of the cardiovascular system.
3. List five basic objectives of the treatment of cardiovascular disease.
4. Differentiate between an inotropic and a chronotropic drug.
6. List the four categories of antiarrhythmic drugs and give an example from each category.
7. List potential adverse side effects of the antiarrhythmic drugs.
8. Describe the actions and potential side effects of the vasodilator drugs.
11. Describe the purpose of dietary sodium restriction in the therapy of cardiovascular disease.
12. List ancillary drugs or procedures that may be used in the treatment of cardiovascular disease.
Key Terms
Afterload
Arrhythmia (Dysrhythmia)
Automaticity
Bradyarrhythmia
Bradycardia
Cardiac remodeling
Chronotropic
Depolarization
Inotropic
Preload
Premature ventricular contraction
Repolarization
Stroke volume
Tachyarrhythmia
Tachycardia
Introduction
Heart disease has a relatively high incidence in veterinary medicine. Studies have found that approximately 11% of all dogs presented to veterinary clinics exhibited some degree of heart disease (Roudebush et al, 2000). Heart disease may be congenital or acquired. However, the acquired form accounts for most cases. The incidence and cause may vary from location to location. Heartworm disease accounts for a large percentage of heart disease in some parts of the country, whereas acquired disease of the atrioventricular valves or myocardium has a more uniform distribution. Acquired disease is encountered more often in older animals, and congenital disease is more prevalent in younger ones.
Whatever the cause, treatment of heart disease is often individualized to the particular patient according to cause, degree of progression, and owner cooperation. The response to treatment must be monitored carefully and adjusted while the disease progresses, which may cause poor liver or kidney function, or while toxic side effects develop. Some cardiovascular drugs have a narrow margin of safety (i.e., they are potentially toxic at low doses), and failing liver and kidney function may reduce the body’s ability to metabolize or eliminate these drugs.
Because veterinary technicians are often the persons who monitor the progress of hospitalized patients, they must be aware of the signs of cardiovascular disease and of normal and abnormal responses to drugs used to treat this disease.
Anatomy and Physiology of the Heart
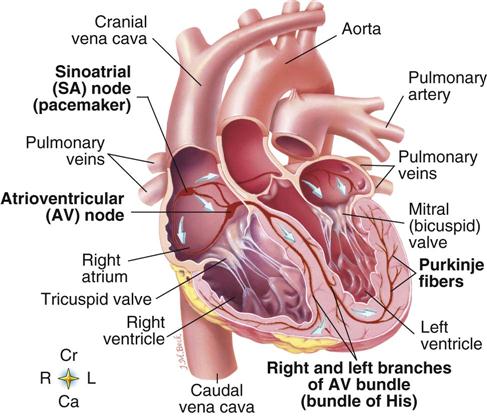
The heart is a four-chambered pump that is responsible for moving blood through the vascular system. The two dorsal chambers are called atria, and the two ventral chambers are called ventricles (Figure 7-1). Each of the chambers is composed primarily of strong muscle tissue called myocardium, which contracts to eject the blood. Even though the heart is considered one organ, it functions as two pumps (Spinelli and Enos, 1978).
The right atrium and ventricle constitute the “right-side pump,” and the left atrium and ventricle make up the “left-side pump.” Blood from the general circulation returns by way of the vena cava to the right atrium, enters the right ventricle through the right atrioventricular valve (tricuspid valve), and is pumped through the pulmonary artery to the lungs. In the lungs, the blood gives up carbon dioxide and picks up oxygen. The oxygenated blood returns to the heart via the pulmonary veins, where it fills the left atrium, passes through the left atrioventricular valve (mitral valve), and enters the left ventricle. The mitral and tricuspid valves swing open when the atria contract and snap shut when the ventricles contract. The closing of the valves as the ventricles contract prevents blood from flowing back into the atria. The left ventricle then contracts and ejects the oxygenated blood through the aorta into the branching arteries. These arteries divide into arterioles and end in the thin-walled capillaries throughout the body, where carbon dioxide is loaded to the blood and oxygen is unloaded to the tissue. Because the left ventricle must work harder to pump blood throughout the body than the right ventricle must work to pump blood to the lungs, the left ventricular wall is thicker than the right ventricular wall.
The pumping action of the heart is divided into two phases—systole and diastole. Systole is the period of contraction of the chambers, and diastole represents the relaxation phase when the chambers are filling with blood. Because each cell in the heart is capable of contracting spontaneously, the interaction of these two phases must be carefully coordinated to create an efficient pumping action. Diastolic time must be adequate to allow the atria to fill completely, and atrial systole must occur shortly before ventricular systole to allow the ventricles to fill maximally. Coordination of these two phases is achieved primarily through a wave of electric activity that arises in a specialized group of cells in the right atrium and then is conducted throughout the myocardium by a special conduction system.
The structures that make up the cardiac conduction system (see Figure 7-1) include the sinoatrial node, the atrioventricular node, the bundle of His and its branches, and the Purkinje system. Under abnormal conditions, parts of the myocardium and conduction system are capable of spontaneous discharge. Normally, however, the sinoatrial node discharges most rapidly and spreads a wave of depolarization over remaining areas of the heart before they can depolarize spontaneously. The rate of discharge of this node therefore controls the heart rate and is called the cardiac pacemaker. Impulses generated by the sinoatrial node travel over the atria to the atrioventricular node, face a brief delay (about 0.1 second) in the atrioventricular node, travel down the bundle of His to its left and right branches, and pass into the ventricular muscle via the Purkinje fibers. Myocardial cells are joined together by structures called intercalated disks and by fusing of cell membranes into an interconnected mass of cells called a syncytium. The syncytium of cells in the atria is separate and is insulated from the syncytium in the ventricles (Ganong, 2003). An electric stimulus from the sinoatrial node is transmitted over the entire atrial mass by the syncytial arrangement of cells. The impulse is not, however, transmitted directly into the ventricular syncytium. The impulse first must be picked up and transmitted by the atrioventricular node through its conduction system to the ventricular syncytium. Stimulation of a single atrial or ventricular muscle fiber causes the entire atrial or ventricular muscle mass to contract as a unit. When situations cause spontaneous depolarization of cardiac muscle or abnormalities of the conduction system, arrhythmias may occur.
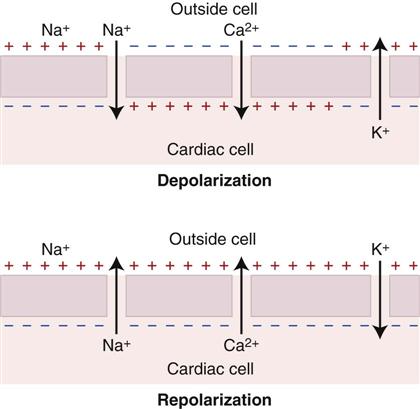
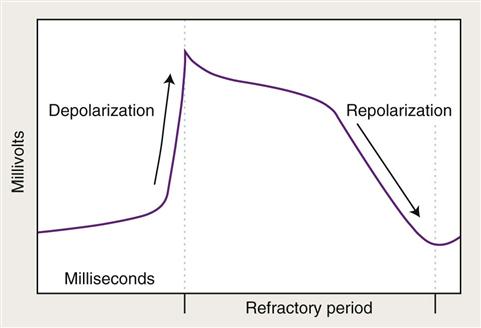
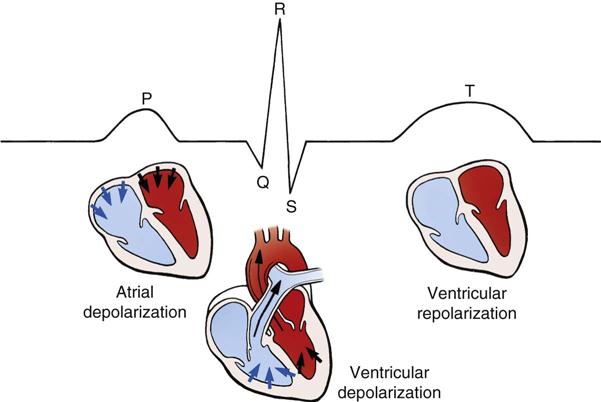
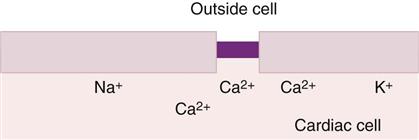
When a cardiac cell is stimulated by electric activity that arises in the sinoatrial node, it undergoes depolarization and contracts. Depolarization is characterized by the rapid influx of sodium ions into the cell through channels or “gates,” the slower influx of calcium ions, and the outflow of potassium ions (Figure 7-2). Until the sodium, potassium, and calcium ions have returned to the positions they had before depolarization, the cell is in a refractory period (Figure 7-3). A cell in an absolute refractory state cannot normally depolarize. In a relative refractory period, however, a cardiac cell can depolarize again, but the stimulus must be stronger than normal. A refractory period is essential for a cardiac cell to prevent it from remaining in a constant state of contraction as the result of stimulation by recycling impulses. The return of the ions to their original positions is brought about in part by the sodium–potassium pump and is an essential part of the repolarization process. Summed electric activity arising from the contraction of all heart cells represents the electrocardiogram (Figure 7-4), and each of its waves signifies activity in a particular area.
Even though the heart establishes its own inherent rate of beating, this rate is subject to outside influences through the autonomic nervous system. The sympathetic portion of the autonomic nervous system, through beta1 receptors, produces positive chronotropic and inotropic effects on the heart. The parasympathetic branch of the autonomic nervous system causes negative chronotropic effects through cholinergic receptors.
The heart pumps blood through a series of arteries (arterial tree) to deliver it to the tissues. The larger of these arteries have elastic properties, which allow them to stretch and recover when blood is pumped into them, thereby serving as a second pump (Upson, 1988). The smaller arteries are capable of changing their diameter (constricting or dilating) through the action of smooth muscle in their walls to increase or decrease the resistance against which the heart must pump. Stimulation of alpha-1 receptors causes vessels to constrict, and stimulation of beta2 receptors causes vessels to dilate.
The amount of blood that the heart is capable of pumping per minute is called cardiac output; this value is calculated by multiplying the heart rate by the stroke volume. The stroke volume is determined in part by the amount of blood that fills the ventricle during diastole, called the preload, and the arterial resistance that the ventricle must pump against, called the afterload.
Compensatory Mechanisms of the Cardiovascular System
The cardiovascular system has a built-in reserve capacity, which allows it to increase its output during times of need (e.g., athletic performance) and to compensate for cardiac disease. The four basic factors of cardiac reserve or compensation are described as follows:
Many disorders can result in cardiac disease. However, most that respond to pharmacologic therapy fall into one of the following categories:
Cardiovascular diseases with the greatest prevalence include mitral disease in dogs, hypertrophic cardiomyopathy in cats, dilated cardiomyopathy in dogs, “Boxer” cardiomyopathy, and heartworm disease (Hamlin, 2003).
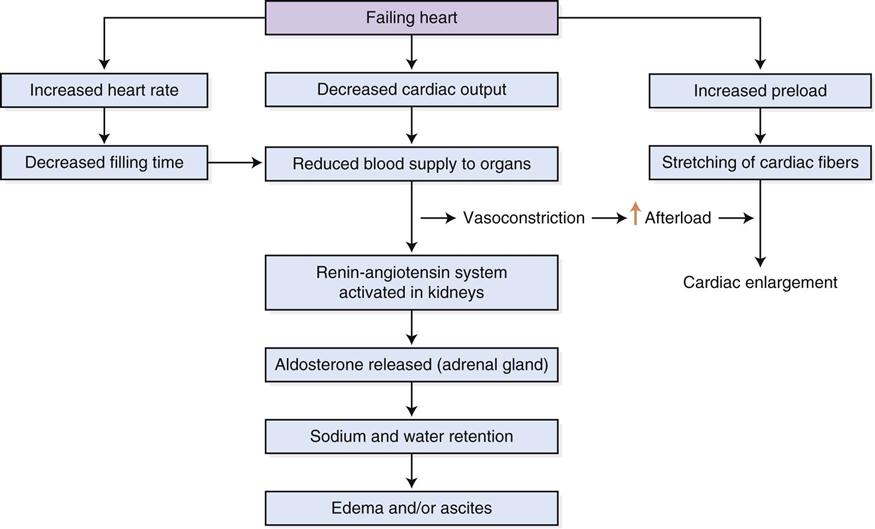
Congestive heart failure (CHF) (Figure 7-5) occurs when the pumping ability of the heart is impaired to the extent that sodium and water are retained in an effort to compensate for inadequate cardiac output. It is associated with exercise intolerance, pulmonary edema, and ascites. The heart usually becomes structurally remodeled in this condition.
Because cardiac disease is a progressive condition in which structural changes occur before clinical signs appear, a classification scheme has been adapted from human medicine to categorize veterinary patients into four categories according to the course of the disease and the treatment for each stage (DeFrancesco, 2013). Table 7-1 lists these stages and general treatment options for each.
TABLE 7-1
Stages and Treatment of Cardiac Disease
| STAGE | DESCRIPTION/SIGNS | TREATMENT |
| A | High risk for development of heart failure but no structural abnormality of the heart | None |
| B | Structural abnormality present but no signs of heart failure | ACEI? Beta blockers? Restricted sodium diet? |
| C | Structural abnormality present and current or previous signs of heart failure/coughing, reduced exercise tolerance | Dog: diuretic, pimobendan ACEI, sodium restricted diet? Cat: diuretic, ACEI |
| D | End stage signs of heart failure resistant to standard treatment/dyspnea at rest | Multimodal therapy |
Basic Objectives in the Treatment of Cardiovascular Disease
Basic objectives in the treatment of cardiovascular disease include the following (Ettinger, 2000):
Categories of Cardiovascular Drugs
 Positive Inotropic Drugs
Positive Inotropic Drugs
The general principle involved in the use of drugs that improve the strength of contraction is that the heart, even in the presence of disease, has reserve capacity for contraction that can be called on to improve cardiac output. Some clinicians advise cautious use of positive inotropic drugs because these can increase the oxygen demand of cardiac muscle, can potentially damage the contractile apparatus, and can increase the tendency for arrhythmias. Proof of clinical efficacy of positive inotropic drugs is lacking, and their use is controversial (Boothe, 2012). Their popularity has waxed and waned through the years as newer, more effective products have come into use.
Cardiac Glycosides (Digitalis)
The digitalis compounds (digoxin and digitoxin) are obtained from the dried leaves of the plant Digitalis purpurea. The beneficial effects of these compounds have been known for hundreds of years and include (1) improved cardiac contractility, (2) decreased heart rate, (3) antiarrhythmic effects, and (4) decreased signs of dyspnea.
Digitalis increases the strength of contraction by increasing the level of calcium ions available in the contractile filaments within cardiac muscle cells. This action occurs as a result of inhibition of sodium–potassium–adenosine triphosphatase (Figure 7-6). The heart rate is slowed by prolonging atrioventricular conduction time and by increasing parasympathetic, autonomic stimulation. The primary actions of the digitalis drugs are to (1) increase the force of contraction, (2) decrease the rate of contraction, and (3) improve baroreceptor function (Hamlin, 2003).
Digitalis use is indicated in patients with cardiac disease that results from impaired cardiac contraction or atrial arrhythmias as suggested by clinical signs such as exercise intolerance, weak peripheral pulses, pulmonary edema, and coughing—or by electrocardiographic diagnosis.
Clinical Uses
Clinical uses of the digitalis compounds include the treatment of CHF, atrial fibrillation, and supraventricular tachycardia.
Dosage Forms
Dosage forms include tablets and elixirs.
• Veterinary approved products are no longer available.
• Digoxin for injection (Lanoxin, 0.25 mg/mL or 0.1 mg/mL in ampules)
• Digoxin tablets (Lanoxin, 0.125 mg, 0.25 mg)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree