The fetlock joint is a rotary joint that can exhibit the greatest range of motion of any equine joint, ranging from 120° of extension to 120° of flexion, particularly during athletic events such as racing or jumping (Fig. 15.1). This high degree of activity makes this joint particularly susceptible to exercise-induced wear and indeed, the fetlocks are commonly associated with injury and signs of degenerative joint disease. The pastern joint, by contrast, is a low range of motion joint exhibiting ~30° range of motion in the normal horse (Fig. 15.2). The pastern is less frequently afflicted with injury or degenerative wear than the fetlock, although its location just above the hoof and at the termination of the suspensory apparatus makes it vulnerable to high-impact, traumatic injury. Degenerative joint disease (high ringbone) frequently follows pastern joint injury. The combination of high-impact loading during sport performance and the distal location of these joints puts them at higher risk for fractures and breakdown. • Signs include acute lameness that often resolves in days, joint effusion and pain on flexion. • Radiography confirms the diagnosis. • Treatment is arthroscopic removal or internal fixation based on size and location of fragment. Most articular chip fractures of the fetlock are of the eminences of the proximal phalanx (P1) and are relatively common in the forelimb of the horse, particularly the sport horse (Fig. 15.3). In racehorses, the left forelimb and medial eminence are affected more often. Other less frequently occurring fractures of the fetlock include fractures of the palmar/plantar eminences which, if articular and small, can be successfully removed arthroscopically with a good prognosis (~70%) for return to performance. These fractures, however, may be associated with subluxation of the fetlock joint and/or disruption of a palmar/plantar osteochondrosis lesion.1–3 Careful evaluation of the joint is indicated to identify this more complex injury which can include injury to the collateral ligaments and distal sesmoidean ligaments. Palmar/plantar fractures of the proximal phalanx are uncommon and should not be confused with osteochondral fragmentation of this site in young growing horses.3 Developmental osteochondral fragmentation of the caudal eminences of the proximal phalanx occurs in ~5% of Standardbreds and Thoroughbreds without clinical signs in most horses. Clinical signs can occur as a high-performance lameness in which case fragments can be arthroscopically removed. True fractures of the caudal eminences of the proximal phalanx usually cause lameness and soreness to direct pressure over the eminence. Developmental osteochondral fragmentation in this location should not induce pain to pressure. Diagnosis is confirmed with radiography, to include four views of the affected fetlock joint and the contralateral fetlock if surgery is to be considered. Osteochondral fragments are readily visible on the oblique radiographic views (see Fig. 15.3). Nuclear scintigraphy can be used to distinguish fractures from incidental caudal eminence fragments. In horses with continued athletic expectations, acute fractures are preferably removed arthroscopically unless they are completely non-displaced. In non-displaced fractures a follow-up radiograph at 30 days is indicated as many of these fragments go on to displace and result in a non-union. In chronic chip fractures, other lesions commonly seen include proliferative synovitis of the dorsal metacarpal synovial pad (32% of which have chip fracture) and cartilage erosion of the metacarpal condyle.4 Two to four months’ rest is recommended before training is resumed depending on the degree of joint damage and cartilage debridement. • Sesamoid fractures are most common in racehorses. • Apical fractures occur most commonly, followed by basilar and midbody fractures. • Treatment is excision for fragments less than one-third the size of the entire bone and internal fixation for larger fractures. Fractures of the proximal sesamoid bones are a common fracture of the fetlock joint. Most are articular although non-articular (suspensory avulsion) fractures occur and can be distinguished by lack of joint effusion and firm swelling over the caudal aspect of the bone. Fetlock breakdown, including sesamoid fractures, is the most common fatal fracture in racing Thoroughbreds and Quarter Horses.9 Sesamoid fractures are categorized as apical, abaxial (articular and non-articular), midbody, basilar (articular and non-articular), sagittal and comminuted.10 Sesamoid fractures are most common (53.4%) in two-year-old and then three-year-old (23%) racehorses. Apical sesamoid fractures are the most common, comprising over 88% of sesamoid fractures with an approximately equal distribution between the right and left limbs (Fig. 15.5). Apical fractures are frequently articular and singular, rarely comminuted and usually involve less than one-third of the bone. Abaxial fractures appear to be more common in Thoroughbreds and Quarter Horses than in Standardbreds (3% of sesamoid fractures).11,12 These can be difficult to diagnose and may require an additional tangential projection on the radiographic examination to identify their exact location or can be identified on the craniocaudal view.13 Articular abaxial fractures will have joint effusion. The midbody transverse fracture is seen most frequently in the Thoroughbred, older Standardbreds (mean age 6.5 years) and in young foals under two months of age. Most have a several millimeter gap and are distracted at the caudal surface. Fracture of both sesamoids usually results in complete loss of suspensory support and a ‘dropped’ fetlock (hyperextended during loading).10 Diagnosis is confirmed with radiography (see Fig. 15.5). Non-displaced fractures may be hard to see with plain radiography. The addition of the skyline projection of the abaxial surface of the sesamoid bone may help identify the exact location of fractures on the abaxial surface.13 Suspicious but unconfirmed fractures should have a repeat radiograph taken after 2–4 weeks of stall rest or nuclear scintigraphy can be performed. Preferred treatment for articular sesamoid fractures (apical, basilar or abaxial) of less than one-third of the bone is arthroscopic removal to provide the most rapid return to athletic use and least risk of degenerative joint disease and sesamoid reinjury. Stall rest (with or without soft cast or external coaptation) for 3–4 months may achieve fibrous or partial bony union, but management is prolonged, weakening of the bone is anticipated and continued soreness or refracture can occur due to failure of complete bony union.12–17 Non-articular fractures can be removed, but conservative treatment is considered to produce similar outcomes and is generally recommended. Midbody transverse fractures affecting the middle third of the proximal sesamoid bones can be treated successfully with lag screw fixation or circumferential wiring to provide postoperative bone compression and immobilization.13,18–21 Fractures involving disruption of both sesamoid bones are a common cause of breakdown in speed horses.9 Many of these horses are humanely euthanized due to compounding of the injury (disruption of the skin) or loss of vascular supply. Horses without an open injury and with immediate support to the limb with a support splint can be salvaged for breeding or retirement. The preferred management is appropriately timed surgical arthrodesis for the fastest return to comfort and to reduce the risk of contralateral laminitis from overloading22 (see Fetlock luxation below). Fractures of the sesamoid can occur in conjunction with a condylar fracture of the metacarpus or metatarsus. This concomitant injury significantly reduces the prognosis for returning to sport athletics even with repair of the condylar fracture.23 These sesamoid fractures are usually sagittal and axial from avulsion of the intersesmoidean ligament that occurs when the condylar fracture displaces. The fractures indicate significant soft tissue injury to the fetlock joint and degenerative joint disease is likely to develop. The prognosis for most simple sesamoid fractures ranges from fair to excellent. Eighty-eight percent of Standardbreds with apical fractures,24 71% of Thoroughbred or Quarter Horse racehorses with abaxial fractures,12 50–60% of Thoroughbreds with basilar fractures14,17 and 50–60% of Standardbreds with midbody fractures repaired by either lag screw fixation or circumferential wiring can return to racing.18,19 Conservatively managed basilar or midbody fractures are most likely to develop significant degenerative joint disease and restricted range of joint motion. If both sesamoids are fractured, the prognosis is less favorable. Sesamoid fractures are a result of excessive forces within the bone, generated by the tension of the suspensory apparatus during loading and occasionally contributed by direct concussion with the ground during fatigue–fetlock ‘rundown’11,13,14,23 (see Fig. 15.4). The forelimbs are most frequently affected in flat racing, whereas the hindlimbs are more frequently affected in Standardbreds. Displaced fractures are common due to the pull of the suspensory ligament proximally and the distal sesamoidean ligaments distally. Although the vascular pattern of sesamoid bones may be implicated in site selection of fractures as the orientation and distribution of vessels correspond to the configuration of apical fracture patterns,25 the sesamoid fracture or the predisposition for sesamoid fracture has not been associated with the presence of sesamoiditis. Sesamoiditis describes a condition of sesamoid pain that demonstrates radiographic lucencies which parallel vascular channels seen radiographically.25 • Fractures may be complete or incomplete. • Most fractures are treated with internal fixation. • Some proximal incomplete fractures will heal with stall rest. The first phalanx is prone to sagittal and, less commonly, frontal plane longitudinal fractures that occur during heavy exercise (Fig. 15.6). Almost all of these fractures are initiated at the articular surface of the fetlock joint and propagate distally.26 Patterns of propagation for sagittal fractures include spiral fractures toward the pastern joint and/or lateral deviation toward the cortex (Fig. 15.7). If fractures extend into the pastern joint or exit the lateral cortex, they are considered complete. Many sagittal fractures are incomplete and propagate distally for varying distances, ranging from < 1 cm (short incomplete) to 5–6 cm (long incomplete) and ending just above the pastern joint.27,28 Complete fractures can be displaced or non-displaced. Incomplete fractures are non-displaced or minimally displaced. A small proportion of sagittal fractures can also contain frontal plane fractures (Fig. 15.8). If this combination of fractures occurs, it is highly predisposed to displacement (comminution) since the sagittal ridge of the metacarpus/tarsus acts as a pile driver upon loading, even with the limb in a cast or splint. Securely positioning the limb vertically on the toe minimizes this effect. A portion of these fractures will also have a third fracture plane (transverse or coronal) which commonly results in complete instability and displacement of the fragments (comminution). Displaced, comminuted fractures are categorized by the presence or absence of an intact strut of bone from the proximal metacarpal/tarsophalangeal joint to the proximal interphalangeal joint. Prognosis for successful surgical reconstruction is greater if an intact strut of bone is present due to the longitudinal support to prevent collapse and providing a secure anchor for reconstruction of fragments.26 Frontal single plane longitudinal fractures can occur in the first phalanx, but are much less common than sagittal fractures (see Fig. 15.6). Clinical signs, treatment and outcome are as for sagittal fractures.29 If a frontal plane fracture is identified on a lateral radiograph, an additional sagittal plane fracture should be suspected and ruled out. Most sagittal and frontal plane first phalanx fractures are best treated with surgical lag screw compression if the fracture length on radiograph is > 1 cm26–29 (see Fig. 15.7, Fig. 15.8). In non-displaced fractures, screws can be placed in lag fashion through small stab incisions. In displaced fractures an incision can improve exposure to ensure anatomic reduction prior to screw placement. Comminuted fractures that have lost an intact strut of bone support from the fetlock to the pastern joint are best treated ideally for several weeks with diverted loading through coaptative devices.30 Positive profile transfixation pins in the metacarpus/tarsus supported with a cast or use of an external fixator apparatus have been successful in managing these fractures and can be used in the presence of open wounds. The prognosis for return to athletic use following repair is good to excellent (> 70%) for non-comminuted, incomplete, non-displaced fractures and complete fractures that exit the lateral cortex.26–28 The prognosis following repair for complete fractures that enter the pastern joint is lower (49%).27 The prognosis for complete fractures is also good if surgical repair effectively compresses the fracture with minimal displacement in the pastern joint. Repair of displaced complete fractures or comminuted fractures can achieve pasture soundness and breeding soundness, but athletic soundness is usually compromised. Sagittal first phalanx fractures occur as the sagittal ridge of the metacarpal/tarsal condyle is loaded rapidly into the first phalanx during galloping (see Fig. 15.1). The shape of the bones and the rotation during movement create torsional forces within the bone, resulting in the classic spiraling fracture. • Lameness localized to the fetlock and suspensory branches. • Radiographically apparent widened vascular channels in the sesamoid confirms the diagnosis. • Reduced exercise level and time for bone remodeling are necessary. Treatment is palliative, including anti-inflammatory medications, physical and adjunctive therapy and supportive wraps in the acute phases. 31 Bisphosphonate therapy has been anticipated to assist with bone quality is sesamoiditis, but these medications have not yet been approved for use in horses in the United States. The intraosseous blood supply to the sesamoid bone enters through a series of abaxial vascular channels that correspond to the enlarged channels seen radiographically in sesamoiditis, indicating bone resorption. This may represent the initiation of the remodeling response to bone stress of training or may reflect an increase in blood flow due to inflammation and injury to the suspensory ligament, or both.25 Sesamoid bone remodeling is a normal response to training and only if stresses exceed the capability to strengthen bone would microfracture and bone damage occur. Although radiographic vascular changes of bone remodeling were not associated with sesamoid fracture, the vascular structures course along known lines of fracture in adult racehorses. The sesamoid bones have an extensive sensory nerve supply that may explain bone pain associated with trabecular bone injury.33 A separate condition of the axial border of the sesamoid bones, an osteomyelitis, has also been called sesamoiditis. Horses with axial sesamoid osteomyelitis are quite lame at the walk and radiographs reveal surface bone lysis at the attachment of the intersesamoidean ligament. The lesions and clinical signs suggest a septic condition in some animals but on histology infarction and necrosis predominate. Presumably an injury to the attachment of the intersesamoidean ligament and possibly seeding with bacteria from intra-articular injections may be associated with the condition. The prognosis for soundness with or without surgical debridement is poor.34 • This injury is unique to the racehorse. • Fractures of the sesamoid bones and/or suspensory ligament disruption occur. • First aid splinting should be done to preserve soft tissues and the local blood supply. • Surgery is done to stabilize the joint for salvage as a breeding animal. Disruption of the suspensory apparatus is a common cause of acute breakdown in the racing Thoroughbred and frequently results in humane destruction of the animal.9,22 Disruption can occur because of rupture of the suspensory ligament, fracture of both proximal sesamoid bones or avulsion of the distal sesamoidean ligaments. Due to the violent nature of these injuries, open fractures, fetlock joint luxation and loss of the vascular supply to the distal limb are associated complications. Successful treatment of these injuries requires immediate and appropriate emergency management of the horse, including sedation, possibly general anesthesia, ambulance service and limb stabilization. Commercial splints such as the Kimzey Leg Saver Splint (Kimzey Welding Works, Woodland, CA) have been designed for this purpose. Euthanasia may be chosen due to the extent of the injuries, risk of treatment failure, lack of sentimental or breeding value of the horse and cost of treatment.22
Distal limb
Fetlock and pastern
Introduction
Fractures of the fetlock joint
Osteochondral (chip) fractures
Recognition
History and presenting complaint
Diagnostic confirmation
Treatment and prognosis
Therapy
Proximal sesamoid bone fractures

Recognition
Diagnostic confirmation
Treatment and prognosis
Therapy
Prognosis
Etiology and pathogenesis
Etiology
Pathophysiology
Longitudinal fractures of the first phalanx
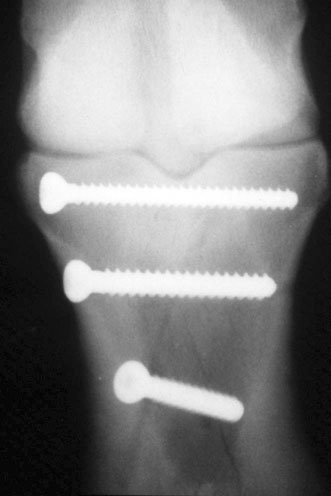

Treatment and prognosis
Therapy
Prognosis
Etiology and pathogenesis
Etiology
Proximal sesamoiditis
Treatment and prognosis
Therapy
Etiology and pathogenesis
Pathophysiology
Prevention
Rupture of the suspensory apparatus