Chapter 7 Diseases and Surgery of the Lens
Diseases of the lens in horses are not common but when present and significant, render the animal devalued, dangerous for some uses, and predisposed to self-injury. This may possibly lead to euthanasia because of the horse’s inability to work or produce. The most common lens disease in all species is cataract—opacity of the lens and/or its capsule. Cataracts can occur congenitally or be acquired postnatally. It is estimated that cataracts are present in 5% to 7% of all horses with otherwise normal eyes.1 These range from incipient opacities to larger visually disturbing cataracts. Other less common lens diseases include abnormal shape and abnormal position of the lens. Diagnosis and treatment of these diseases of the lens will be described in detail in this chapter.
Clinical Anatomy and Physiology
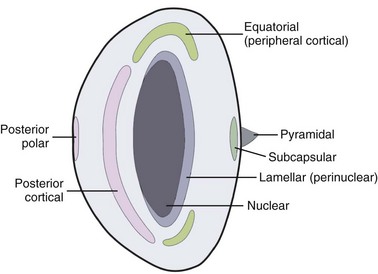
The crystalline lens is the second most important refractive structure of the eye. Its role is to focus incoming light onto the area centralis. The lens is unique insofar as it is transparent, devoid of innervation and vascular structures, yet it grows throughout embryologic development and continues until the death of the horse. Lens embryology, anatomy, physiology, and function differ little between terrestrial species.2 Lens epithelial cells (LECs) line the anterior aspect of the lens in a monolayer and perform the majority of the metabolic functions for this structure (Fig. 7-1). They transport solutes between the lens and the aqueous humor, are important for enzymatic activity, secrete capsular material, and their metabolism maintains lens transparency.3 Any imbalance in enzymatic activity or lens metabolism due to DNA or protein damage to the LEC can lead to cataractogenesis.3
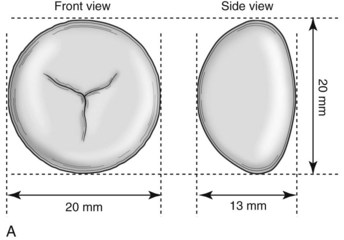
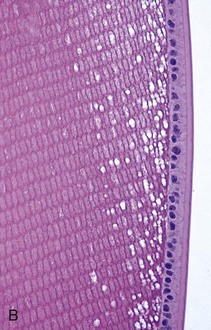
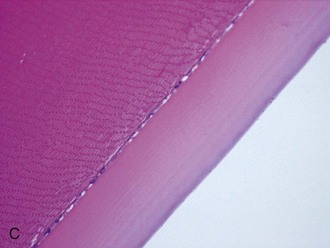


Figure 7-1 A, Schematic cross-section of the adult equine lens. B, Photomicrograph of the anterior lens capsule from a 2-day-old Thoroughbred foal.137 Note the prominent lens epithelial cells and thin anterior capsule compared with C (H&E ×400). C, Photomicrograph of the anterior lens capsule from a 10-year-old Quarter Horse (QH) gelding (H&E ×400). D, Photomicrograph of the lens bow in the foal from B (H&E ×100). E, Photomicrograph of the lens bow from the QH gelding in C. (H&E ×100).
The remainder of the lens is made up of terminally differentiating and differentiated lens fiber cells. The process of terminal differentiation begins in the equatorial (or lens bow) region (see Fig. 7-1) that entails elongation, loss of cellular structures, posttranslational modification of proteins, and gradual migration into the cortex. During this migration, they lose their nuclei through an apoptosis-like mechanism.4 Losing cellular structures ensures the clarity of the lens by removing potentially light-scattering elements from the incoming light pathway. The region immediately inside the area of organelle loss is called the organelle-free zone (OFZ)5 and begins in the peripheral adult nucleus.
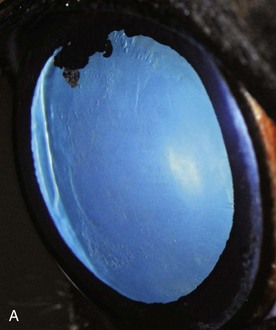
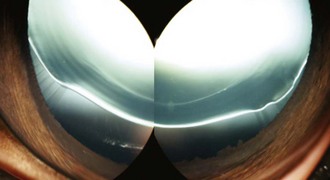
Clinically, there are three major regions that are important: the nucleus, the cortex, and the lens capsule. Beginning from the middle towards the outside, the nucleus is the oldest section of the lens. There are three subdivisions of the nucleus, based on the age of the animal (see Fig. 7-1). The innermost nucleus is the embryonic nucleus that is formed from primary lens fibers at the earliest time of lens development. The region that then surrounds the embryonic nucleus is the fetal nucleus. These are the first secondary lens fibers, and they form until the animal is born, so at birth, the lens is only made up of the embryonic and fetal nuclei surrounded by the lens capsule. The lens capsule is continually produced by the anterior lens epithelial cells throughout development and postnatal life. Postnatally, the secondary lens fibers create the cortical region and begin to form the future adult nucleus. In a young adult horse (approximately 5 to 7 years of age), the lens will have an obvious area between the lens capsule and the outermost nucleus that is the cortical region. The cortical region is composed of the newest cells that are continually being moved inward; therefore, any random elongating cortical fiber cell is surrounded on the inner aspect by an older fiber cell, on each side by similar-aged fiber cells, and at its outer aspect by a newer fiber cell. At approximately 15 to 20 years of age, the entire nucleus is more obvious owing to the layers of cells that have been compressed over time and begin to refract light. This is termed nuclear sclerosis and is a typical aging change in all eyes (Fig. 7-2).
Congenital Diseases
Ocular abnormalities of the neonatal foal may be congenital, inherited, or acquired. Congenital defects may be due to genetic causes/inheritance, toxins, nutritional imbalance, ionizing radiation, or other idiopathic causes.6,7 Cataracts are the most common congenital abnormality present in foals, with a 33.6% to 35.3% incidence in cases of congenital ocular defects.7,8 Other lens anomalies include spherophakia, lenticonus, and coloboma.
Congenital Cataracts
Congenital cataracts are the largest group of developmental lens opacities in horses. Inherited congenital cataracts have been documented in Thoroughbreds, Quarter Horses, and Morgans.9–11 Rocky Mountain horses can also develop congenital nuclear cataracts but have concurrent multiple anterior segment anomalies.12 It is sometimes possible to estimate the time a cataract originated and also determine whether it will progress. Nuclear cataracts involving the embryonic or fetal nuclei do not progress and usually become smaller relative to the rest of the lens as the animal ages. Perinuclear cataracts, by nature of when the cortex begins to develop relative to the date of birth, occur just after the animal is born. The nucleus and the inner nuclei are usually clear. This type of cataract or nuclear cataracts are inherited in the Morgan horse.9 Cataracts are often seen in equine eyes with other anomalies like microphthalmia and anterior segment dysgenesis (Fig. 7-3). They are present in Rocky Mountain Spotted horses with multiple ocular anomalies.13,14 Congenital cataracts can occur with other anomalies such as persistent pupillary membranes and aniridia.15,16
Primary Aphakia, Microphakia, and Coloboma
Primary aphakia and microphakia (Fig. 7-4) are extremely rare and occur with other anomalies in the eye, including coloboma (Fig. 7-5) due to inadequate insertion of zonules at the lens equator.17,18 In cases of presumed aphakia or microphakia without other ocular anomalies, it is possible that the lens developed a cataract in utero, and it was resorbed prior to birth or soon after.



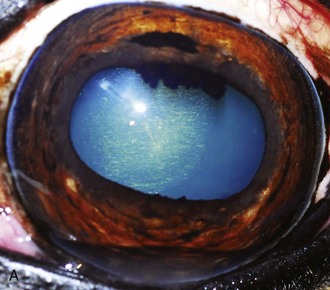
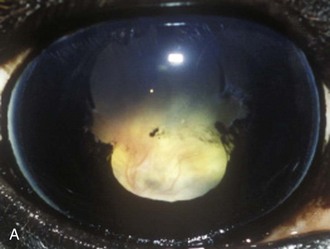
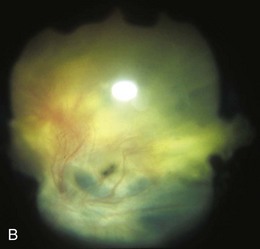
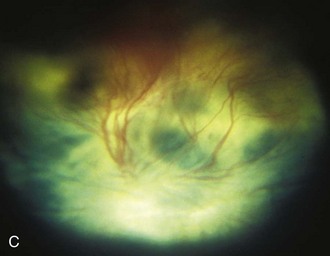
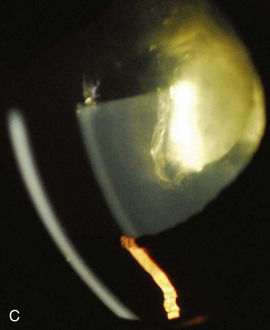
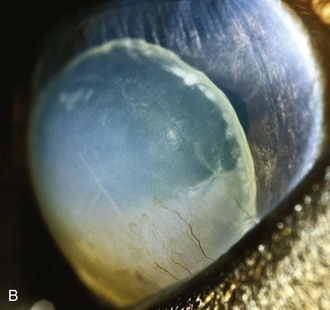
Figure 7-4 A, Anterior lens luxation, mild corneal edema and keratitis, and microphthalmia in a foal. B, Lens resorption (possible microphthalmia) in a 4-day-old Thoroughbred foal. C, Left eye from foal in Fig. 7-3, B with further lens resorption and cataract density. Note lack of zonular attachment.
(A Courtesy Dr. David Wilkie. B and C Courtesy Dr. Ricardo Stoppini.)
Ectopia Lentis
Ectopia lentis, also rare, occurs when the lens vesicle fails to enter the optic cup, and the lens attempts to form in the anterior chamber. In one case, the lens was also microphakic and spherophakic.18 Congenitally displaced lenses are often abnormal in shape (spherophakia) and smaller than normal (microphakia). The early contact between the optic vesicle and the surface ectoderm, and its subsequent appropriate changes, result in a normally positioned, normally shaped, transparent lens. If anything changes any of these steps, the lens will be abnormal in position, shape, and opacity. The most severe anomaly occurs when this initial contact does not separate appropriately; this results in anterior segment dysgenesis, anterior lenticonus, and anterior capsular cataracts.14,19 Anterior segment dysgenesis often occurs with microphthalmia.17,20–22
Congenital Anomalies That May Be Associated With Cataracts
Examples of congenital anomalies that may be associated with cataracts include persistent pupillary membranes, persistent hyaloid artery, persistent hyperplastic primary vitreous/persistent hyperplastic tunica vasculosa lentis (PHPV/PHTVL [Fig. 7-6]), posterior lenticonus, microphakia, microphthalmos, and lens coloboma. The hyaloid artery system is typically resorbed in the first few weeks postnatally. However, complete regression of the hyaloid system, including its remnants, occurs by 6 to 9 months of age in horses.23
Persistent pupillary membranes (PPMs) are often seen in clinically normal horses. One study including 169 neonatal Thoroughbred foals found PPMs in 28% of left eyes and 25% of right eyes; 23% of the foals had bilateral involvement.24 However, PPMs that arise from the iris collarette and attach to the anterior lens capsule are rare.16 The same study of neonatal foals found the hyaloid artery or its remnants present in 83% of left eyes and 87.5% of right eyes; 80% were bilateral.24 One horse in this survey had bilateral capsular cataracts related to the hyaloid remnant.24 In a survey of Thoroughbred racehorses in Australia, one horse from a total of 204 was found to have a hyaloid remnant.25 PHPV/PHTVL (see Fig. 7-6) has not been described in the equine literature. Mittendorf’s dot, the anterior attachment of the hyaloid artery to the posterior lens pole, has been documented and can occur in a triradiate configuration.16 Bergmeister’s papillae, a remnant of the hyaloid artery seen protruding from the optic nerve head, is rare in horses.
Acquired Diseases
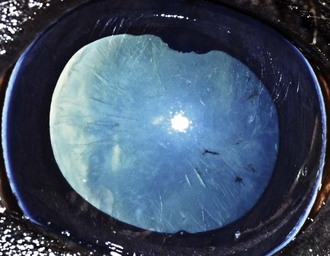
Acquired diseases of the lens in mature horses that will be discussed in this section include subluxation, luxation, puncture or laceration, expansion, rupture, and opacity of the lens or lens capsule (cataract). Although several of the lesions discussed in the following section may also be encountered in foals, they are most commonly identified during ophthalmic examination of the adult horse. There is a recent description of lens opacities, with representative photographs providing an extensive classification system based on etiology.1 Most cataracts in horses develop secondary to intraocular disease such as uveitis (ERU and other forms of anterior and/or posterior uveitis), retinal detachment, neoplasia, coup-contrecoup or whiplash injury to the globe, advanced age, or metabolic diseases or toxins.1,26 Senile cataracts (Fig. 7-7) can be frequently encountered in horses older than 18 years of age and may interfere with vision.1 Many geriatric horse lenses show increased nuclear delineation, or nuclear sclerosis (see Fig. 7-2), which may be associated with the development of senile cataracts. Occasionally, increased brunescence (Fig. 7-8) of the lens nucleus can be seen in such instances.1
Cataracts
As in other animal species and humans, cataract development is a common sequela of uveitis (Fig. 7-9) and trauma (Fig. 7-10). The rate of cataract progression is dependent upon the underlying cause. ERU and other forms of uveitis are associated with an accelerated rate of cataract progression, and it is still generally accepted that inflammation of the anterior uvea (e.g., ERU) is the most common cause of acquired cataracts in horses.1,10,16,27–44
Clinical Appearance
The classification of adult cataracts can follow several different schemas. Briefly, cataracts can be described by their age of onset (congenital, juvenile, or senile/geriatric), cause (e.g., hereditary, secondary to uveitis, trauma, toxin, nutritional, or metabolic disease), or location within the lens (anterior polar, anterior subcapsular, anterior cortical, lamellar/perinuclear, equatorial, peripheral cortical, posterior cortical, posterior subcapsular, or posterior polar [Figs. 7-11 to 7-18]). Several characteristics of a cataract, including location, density, size of a focal cataract, and blockage of the fundic reflex, determine its effect on vision.10,45

Figure 7-13 Diffuse, incipient, anterior subcapsular cataract in the right eye of a 19-year-old Morgan gelding.

Figure 7-14 Focal, incipient, anterior cortical cataract in the left eye of a 12-year-old Thoroughbred gelding.
Common Differential Diagnoses
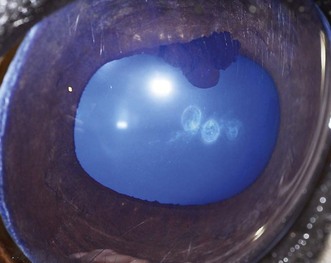
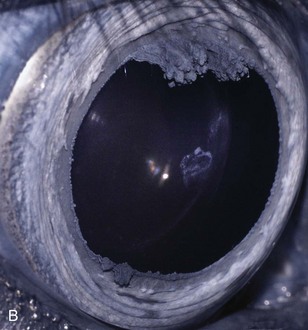
Acquired cataracts in horses are often caused by uveitis (Fig. 7-19) or trauma (Fig. 7-20).* Juvenile cataracts, common in many canine breeds, are uncommon in horses.10,47,48 Cystic lesions associated with the anterior lens capsule and/or anterior subcapsular cortex (Fig. 7-21) are being identified more frequently; they appear to precede anterior uveitis and are independent of ocular trauma.10,16,35 Senile cataracts significant enough to interfere with vision are also uncommon in horses.49 Nuclear sclerosis is a relatively common finding among aged horses, but vision remains clinically unaffected.35,50

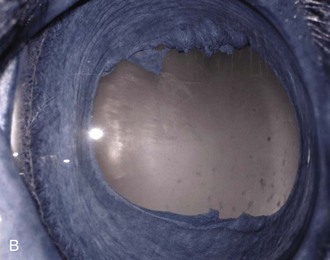
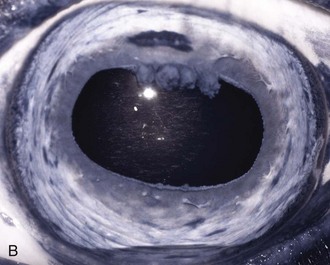
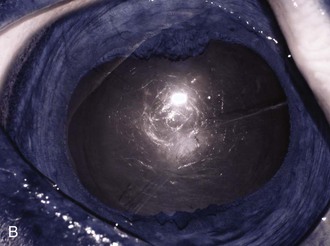
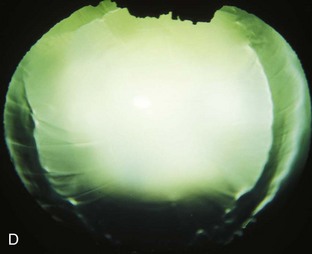
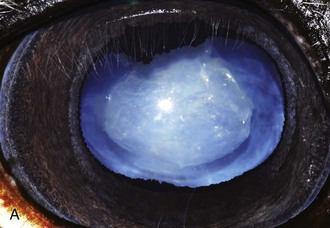
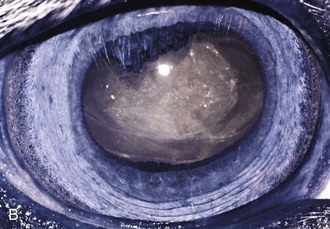
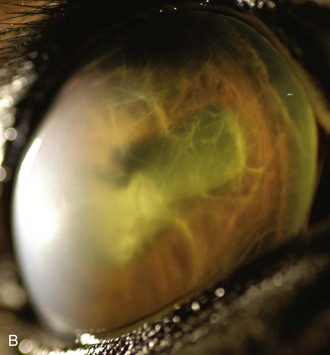
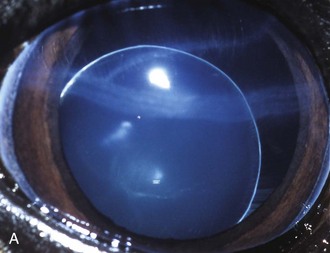
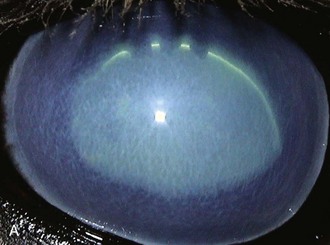
Figure 7-19 A, Complete mature cataract associated with chronic equine recurrent uveitis. B, Infrared. Note bluish-gray color of the pupil, consistent with cataractous changes, or opacifications, of the lens.136
Lens suture lines (Y sutures) can be visualized in most foals and adult horses during routine ophthalmic examination, and it is important to differentiate these opacities from cataracts.6,7,50,51 In a group of 144 foals ranging in age from 5 days to 19.5 weeks (mean age 9.4 weeks), lens sutures were visible in 137 animals.6
Treatment
Historically, horses with cataracts associated with ERU were not considered appropriate candidates for cataract surgery. Concurrent pathologic ocular changes in the eye and the high rate of postoperative complications resulted in very low surgical success rates.45,52 However, horses with well-controlled uveitis should be considered reasonable candidates for cataract surgery to restore vision.32,53–55
Lens Luxation
Lens luxation or subluxation may be caused by congenital anomalies of the zonules, chronic uveitis, or glaucoma and may be exacerbated by trauma.† A luxated lens will usually become cataractous, with focal or diffuse opacification appearing immediately or weeks following a traumatic incident as a result of the disruption in the protein exchange between the aqueous humor and the lens.41,57,58
†References 36, 37, 41, 43, 46, and 56.
Clinical Appearance
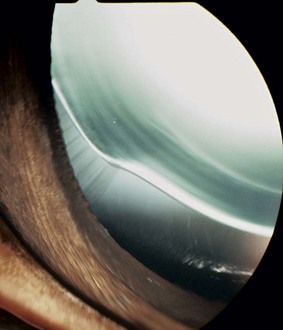
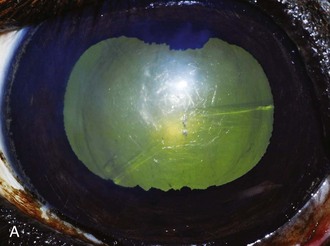
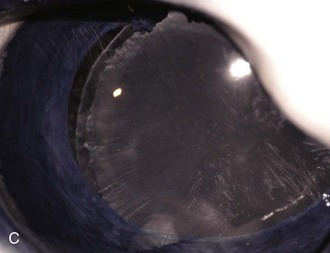
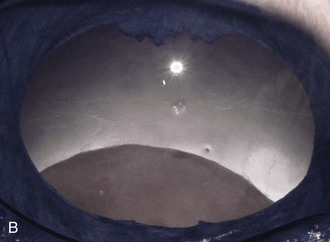
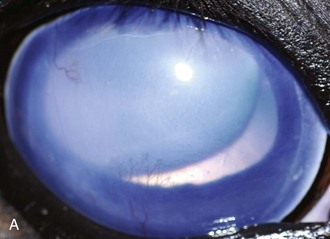
Lens luxation and subluxation are rare in horses.55 A subluxated lens is one that has partially broken free from its zonular attachments, but the lens remains within its normal position behind the iris and within the patellar fossa (Fig. 7-22). Slight displacement of the lens, however, allows the edge of the lens to be visible within the pupil, producing the appearance of an aphakic crescent (Fig. 7-23). Complete luxation manifests as displacement of the lens into either the anterior chamber (i.e., anterior lens luxation [Fig. 7-24]) or into the vitreous body (i.e., posterior lens luxation [Fig. 7-25]).13
Because of the lack of physical contact between the posterior iris surface and the anterior surface of the lens in cases of either subluxation or luxation of the lens, iridal instability manifests as a slight vibration of the iris (iridodonesis) that can be visualized during ophthalmic examination. Although primary (hereditary) lens luxation has not been documented in the adult horse, there are reports of congenital bilateral lens subluxation in an Arab cross foal59 and subluxation and cataract formation associated with the multiple congenital ocular anomalies syndrome described in Rocky Mountain Spotted horses.13 The prognosis for vision and globe retention is dependent upon the nature and severity of the primary ocular disease.55,60
Common Differential Diagnoses
A rare, presumably congenital anomaly that must be differentiated from a lens subluxation is a lens coloboma (Fig. 7-26).18 Faulty lens zonular formation, and therefore lack of insertion at the lens equator, results in an area where the lens equator is not stabilized and held in its normal position. This results in a focal flattened area or notch in the peripheral lens equator, associated with the missing zonules. An aphakic crescent can usually be identified (Fig. 7-27), but signs of ocular inflammation (e.g., aqueous flare, miosis) are not generally associated with lens colobomas and should be differentiated from a subluxation of the lens secondary to anterior uveitis or glaucoma (Fig. 7-28).
Treatment
Intracapsular lens extraction has historically been recommended in cases of lens luxation in an attempt to preserve vision.9,10,61,62 Recent retrospective long-term evaluation in such cases has revealed that surgical intervention is coupled with an extremely poor prognosis for both retention of vision and the globe.60 However, prior to surgical intervention being considered, an attempt should be made to determine the underlying cause for the displacement. Because extensive uveal tissue damage may be incurred as a result of the underlying uveitis or trauma precluding lens luxation, phthisis bulbi or blindness associated with retinal degeneration may result, especially in cases involving posterior lens luxation.55,63 As an alternative to lens removal in uncomfortable blind eyes with secondary lens luxation, enucleation or evisceration with insertion of intrascleral silicone prosthesis may be considered.64–68
Lens Capsule Rupture
Blunt and penetrating ocular trauma is relatively common in the horse, and lens capsule rupture may be incurred as a result. Lens capsule ruptures are usually associated with rupture, laceration, or puncture of the cornea or sclera. Uveal or retinal tissue exposure as well as herniated lens material may develop leading to severe uveitis or blindness.9,61,69
Clinical Appearance
Any penetrating ocular injury has the potential to cause damage to the lens capsule, and corneal lacerations are relatively common in the horse.46,70–73 Thorough evaluation of the lens capsule is required following any case involving penetrating or perforating corneal injuries. The inherent nature of such injuries often make it difficult, if not impossible, to adequately evaluate the lens capsule simply using direct ophthalmoscopy or slit-lamp biomicroscopy. Ocular ultrasonography, or if available, high-resolution ocular ultrasonography, should be performed to increase the probability of identifying a disruption of the anterior lens capsule.14,74–77
In severe cases, the anterior chamber may be collapsed, uveal prolapse may be present, and lens material may be extruding from the lens capsule or corneal wound. Even in cases without full-thickness corneal defects, signs of anterior uveitis will usually be present and include fibrin formation, hyphema, and miosis, making examination of the lens nearly impossible. Clinical evaluation of the lens can be facilitated by removal of the intraocular fibrin, irrigating the anterior chamber, and dilating the pupil with dilute (1:10,000) intracameral epinephrine, with the horse in lateral recumbency under general anesthesia prior to surgical correction of the corneal defect.55 It is important to have the animal paralyzed or to have performed a retrobulbar block in order to fully manipulate the globe and minimize tension from the extraocular muscles when performing these procedures.
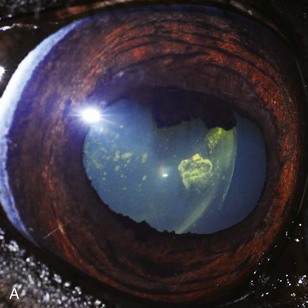
Common Differential Diagnoses
Chronic and insidious intraocular inflammation may torment a horse following a penetrating ocular injury. Endophthalmitis may be caused by intraocular sequestration of bacterial or fungal organisms, deposition of foreign material such as plant debris, the release of lens proteins, and/or an unrelenting inflammatory response to these insults (Fig. 7-29). Thorough ocular examination, aerobic and anaerobic bacterial and fungal culture and sensitivity of corneal scrapings and intraocular fluids, as well as ocular ultrasonography are necessary to help identify the underlying cause of the ocular inflammation prior to deciding which medical or surgical approach is most appropriate.
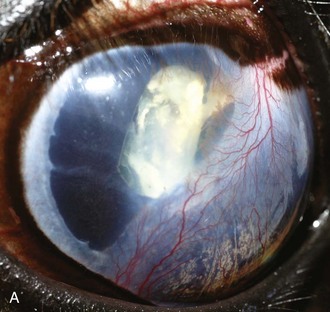
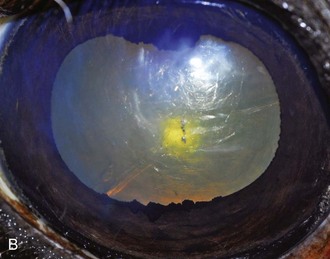
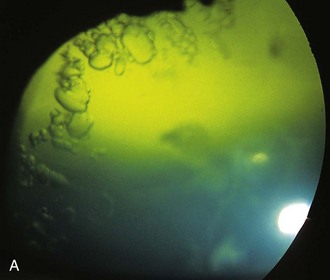
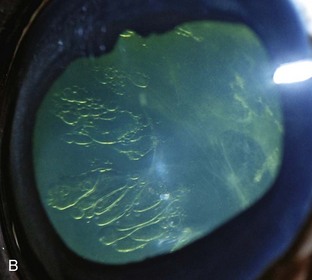
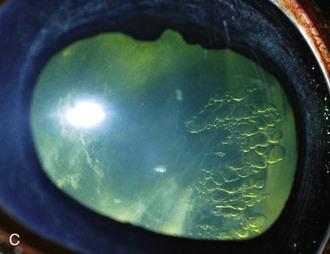
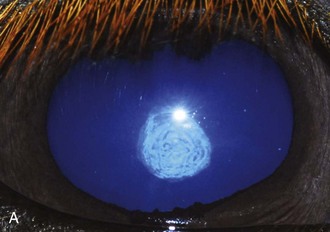
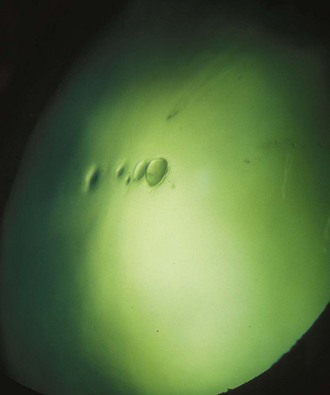
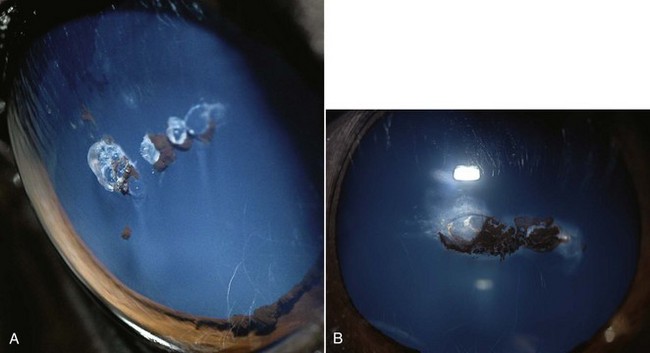
Anterior subepithelial cysts (Fig. 7-30) are an additional poorly characterized ocular disease that appears to involve the anterior subcapsular epithelium and/or subepithelial anterior cortex. They should be considered when confronted with a case of recurrent anterior uveitis or ocular trauma with anterior lens involvement. Although very little information exists on this presumably congenital abnormality, it is being identified with increasing frequency (Fig. 7-31). Usually, horses will present with a history and/or clinical signs of chronic recurrent uveitis (i.e., blepharospasm, epiphora, and miosis with mild aqueous flare) that are associated with active and quiescent periods of inflammation. Generally, these lesions respond rapidly to topical and systemic antiinflammatory medications and topical mydriatics, with signs subsiding within 1 or 2 weeks. As with chronic recurrent uveitis, however, they tend to go through a vaguely predictable period of quiescence prior to additional phases of acute inflammation. With the exception of pigment deposition surrounding the cystic lesion on the anterior lens capsule, the iris itself does not usually show signs of chronic inflammation (i.e., corpora nigra degeneration, iridal hyperpigmentation). Cases that prove more resistant to tradition medical therapy alone may benefit from surgical implantation of a suprachoroidal cyclosporine implant78,79 for long-term suppression of inflammation or lens extraction with intraocular lens implantation if the lesion is large enough that it is also affecting vision.10,16
Treatment
Surgical lens removal is the treatment of choice in dogs following capsule rupture and should be performed at the same time as surgical correction of the corneoscleral injuries.66,69,80 Although little information pertaining to this manifestation of lens disease in the horse has been published, phacoemulsification following acute anterior lens capsule rupture has been successfully performed.81 Prognosis for vision is poor following blunt trauma, because it can result in cataract development, lens capsule rupture, and staphylomas at the limbus66 and subsequent retinal detachment. Evisceration with intrascleral silicone prosthesis or enucleation may be indicated.62,64,67,68
Evaluation and Treatment of Cataracts
Evaluation of the Equine Patient with Cataracts
An ophthalmic examination should be a routine part of any prepurchase or insurance examination and should be conducted during the initial physical examination on all newborn foals.26,62,83 Prompt and complete pupillary light responses (PLRs) and a blink response to bright light (dazzle) are generally indicative of adequate retinal function.62 A focal light source such as a penlight or Finnoff transilluminator generally allows for identification of diffuse or focal axial cataracts (Fig. 7-32), but complete evaluation of the lens requires pharmacologic mydriasis.61 Two doses of topical 1% tropicamide, 0.1 to 0.2 mL topically at 5-minute intervals, will generally provide adequate mydriasis of the equine pupil to facilitate ophthalmic examination within 15 to 30 minutes. Focal incipient cataracts (Fig. 7-33) do not prevent evaluation of the equine ocular fundus. However, if diffuse cataracts are present, both ocular ultrasonography14 and electroretinography84 should be performed (see Chapter 1 for more details) to evaluate retinal integrity and function.10,55,61
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree