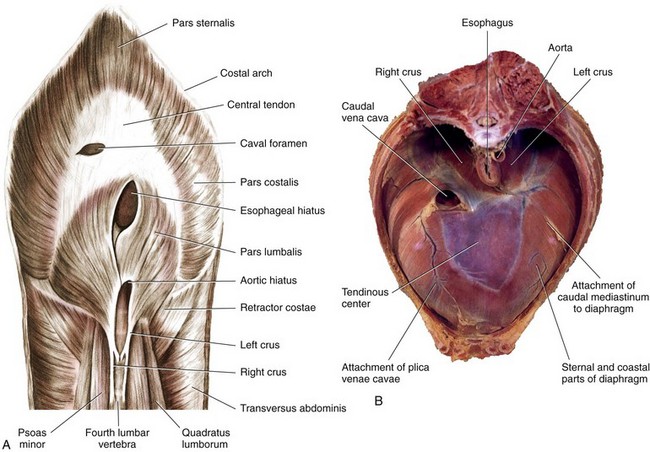
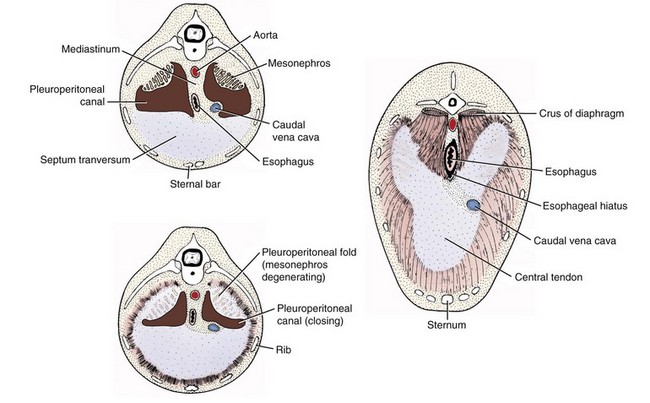
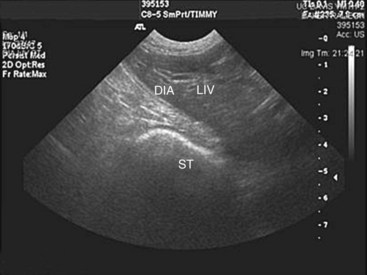
Chapter 85 The diaphragm is a musculotendinous partition that separates the abdominal and thoracic organs, assists in ventilation, and has a role in movement of lymphatic fluid. The diaphragm is composed of a strong central tendinous section, which makes up 21% of its surface area. The tendon is approximately Y shaped, with each arm of the Y extending dorsally from the central region up to the thirteenth rib. The tendon is composed of two layers of fibers and, around the foramen venae cavae, these fibers have a strong, concentric arrangement.31 The central tendon is surrounded on all sides by diaphragmatic muscle. The diaphragmatic muscle is divided into the pars lumbalis and pars sternalis dorsally and ventrally, respectively, and a pars costalis on each side (Figure 85-1). The paired lumbar muscles form the diaphragmatic crura, with the right crus being considerably larger than the left. Each crus has a bifurcate tendon arising from the bodies of the third and fourth lumbar vertebrae medial to the psoas minor muscles.31 The musculature of each crus is further differentiated into lateral, intermediate, and medial portions. Splanchnic nerves and the sympathetic trunk pass into the abdomen between the lateral portion of the crus and the thirteenth rib on each side.31 The left and right costal muscles of the diaphragm form a uniform sheet arising from the medial proximal portion of the thirteenth rib, distal part of the twelfth rib, costochondral junction of the eleventh rib, all of the tenth and ninth ribs, and the eighth costal cartilages.31 The costal muscles extend centrally and insert on the abaxial borders of the diaphragmatic central tendon. The sternal muscle is an unpaired medial muscle continuous with the left and right costal muscles.31 It originates on the base of the xiphoid cartilage, adjacent transverse fascia, and the eighth costal cartilages and extends forward to insert dorsally on the body of the central tendon. The diaphragm has three openings: the aortic hiatus, esophageal hiatus, and caval foramen. The caval foramen lies within the dorsal portion of the central tendon to the right of the median plane. Adventitia of the caudal vena cava, which passes through the foramen, fuses with the tendon at that site to leave no surrounding space. The esophageal hiatus is more dorsal, lying between the two medial divisions of the right crus. It transmits the esophagus and its blood supply and the dorsal and ventral vagal trunks. The aortic hiatus is the most dorsal. It is bordered dorsally by bodies of the lumbar vertebrae and ventrally by extensions from the left and right crural tendons.31 The aorta, azygos, and hemiazygos veins and lumbar cistern of the thoracic duct pass through the aortic hiatus. The margins of the esophageal and aortic hiatus can slide over structures passing through. The convex, thoracic surface of the diaphragm lies adjacent to the lungs and is covered by endothelial fascia and pleura, the pleura being continuous with that of the mediastinum.31 Dorsal to the esophagus, the mediastinum attaches to the diaphragm on the midline. Ventral to the esophagus, it deflects to the left in a wide semicircle across the left diaphragmatic costal muscles and returns to the midplane just at the sternum. A pleural reflexion (plica vena cava), caudal to the heart around the caudal vena cava, is attached to the diaphragm on the right side. Cranial to the diaphragmatic central tendon, the plica vena cava and the mediastinum form a median cul-de-sac that surrounds the accessory lung lobe.31 The concave, abdominal side of the diaphragm is covered by microscopically thin layers of transverse fascia and peritoneum.1,31 Stomata in the diaphragmatic peritoneum provide the major lymphatic drainage from the peritoneal cavity to the sternal lymph nodes.1,31,47 In dogs, the parietal surface of the liver is in contact with most of the diaphragm.31 The blood supply to the diaphragm is derived principally from the main phrenic arteries.31 They arise from the paired phrenicoabdominal arteries and extend forward to ramify subperitoneally on the crura of the diaphragm. These vessels then pass medial to the dorsal extensions of the tendinous center, divide over the tendinous part, and redivide farther in the peripheral musculature. Terminal branches of the phrenic arteries follow the muscular fibers of the costal muscle and anastomose with the phrenic branches of the tenth, eleventh, and twelfth intercostal arteries. Each side of the diaphragm is drained by a single phrenic tributary that begins in the ventral part of the muscular diaphragmatic periphery. The phrenic veins empty into the caudal vena cava as it passes through the caval foramen.31 The sole motor innervation of the diaphragm is from the phrenic nerves.31 In dogs, these arise from the ventral branches of the fifth, sixth, and seventh cervical nerves, and occasionally a small twig comes from the fourth nerve.31 Cranial to the diaphragm, the right and left phrenic nerves are invested by the plica vena cava and mediastinum, and each divides into approximately three branches to innervate all three diaphragmatic muscles.31 In cats, the phrenic nerves are derived from the fourth, fifth, and sixth cervical nerves. The costal muscles are supplied by axons derived partly from the fourth nerve but mainly from the fifth nerve, and the crural musculature is supplied by axons mainly from the sixth and partly from the fifth cervical nerves.77 Embryogenesis of the diaphragm is complex.66 Initially, the transverse septum forms an incomplete partition between the pericardial and peritoneal cavities (Figure 85-2). This septum originates in the region of the cervical vertebrae and, during embryogenesis, migrates caudally to the level of the first lumbar vertebrae, where it becomes the central tendon. The cervical origin of the diaphragm explains the location of the phrenic nerve roots in the cervical intumescence. The dorsal mesentery of the esophagus appears at the same time as the transverse septum and constitutes the median portion of the diaphragm dorsal to the transverse septum. In adults, this mesentery forms the diaphragmatic crura, including the esophageal hiatus and aortic hiatus. The pleuroperitoneal folds develop along the lateral body walls and migrate medially, where they close the pleuroperitoneal canals by fusion with the esophageal mesentery and dorsal portion of the transverse septum, thereby completing the diaphragmatic partition. Finally, as the pleural cavities enlarge, myoblasts from the body wall invade the peripheral border of the diaphragm to form the costal muscles.66 Contraction of the diaphragm during inspiration pushes caudally on the viscera, displacing the abdominal wall outward.24 In conjunction with this action, contraction of the diaphragmatic costal muscles produces expansion of the caudal ribcage.24,43,59 Contraction of the diaphragmatic crura normally has no net effect on caudal ribcage dimensions except when the abdominal cavity is open. In that instance, it produces a paradoxic inward displacement of the caudal ribcage during inspiration. After bilateral phrenicotomy (phrenic nerve transection) in normal dogs, the diaphragm is paralyzed. Although chest wall expansion is produced by contraction of inspiratory intercostal muscles on the lateral walls of the ribcage, the parasternal intercostal muscles are responsible for inspiratory dorsal displacement of the sternum.25 In normal dogs bilateral phrenicotomy was claimed not to adversely affect ventilation or produce exercise intolerance;31 however, diaphragmatic paralysis resulting from motor unit diseases is a cause of respiratory insufficiency.42,112 Midline celiotomy is the preferred approach for most traumatic diaphragmatic hernias and all congenital peritoneopericardial hernias unless dense adhesions are present between herniated viscera and intrathoracic structures.2,39,72,110 The midline approach allows inspection of all the abdominal viscera, can be extended to a sternotomy for thoracic exposure, causes less postoperative pain than a thoracotomy, and provides access to all of the diaphragm. Using this approach, it is not necessary to know the position of the diaphragmatic tear before surgery. A disadvantage of this approach is that the diaphragm is viewed from its concave surface, making suturing more difficult. Another disadvantage is that adhesions of abdominal viscera to intrathoracic structures may not be easily or safely broken down without enlarging the opening in the diaphragm or extending the celiotomy to a median sternotomy. A ninth intercostal lateral thoracotomy approach provides adequate exposure of herniated viscera and diaphragmatic tears, as long as the hernia side is known, and allows inspection of the convex pleural surface.92 Adhesions can be easily seen and transected, although significant adhesion formation in chronic diaphragmatic hernia is rarely a complication. With a lateral thoracotomy, it is mandatory to make the approach on the side of the hernia. Exposure is limited if the hernia is on the contralateral side or extends bilaterally or if intervention on abdominal cavity viscera is needed. The surgeon must then perform either a contralateral intercostal thoracotomy or celiotomy. The lateral thoracotomy approach is contraindicated for peritoneopericardial hernias. Diaphragmatic hernias are generally categorized by etiology because, except for hiatus hernia, true diaphragmatic hernias are rare.104 Herniated viscera in true diaphragmatic hernia are contained within a sac of peritoneum.104 Pathophysiology: Trauma is the most common cause of diaphragmatic hernia in dogs and cats, comprising up to 85% of cases.15,110,111 Automobiles are the chief source of trauma, with kicks, falls, and fights reported less frequently.15,105,110 Soft tissue fragility was implicated in the development of a diaphragmatic hernia, independent of a serious traumatic event, in a cat with cutaneous asthenia.12 Injury to the diaphragm can be either direct or indirect in origin. Direct injuries from thoracoabdominal stab and gunshot wounds are rarely encountered in animals13 but are a frequent cause of diaphragmatic injury in humans.30 Iatrogenic injury of the diaphragm may occur during thoracentesis,27 with inappropriately positioned chest drains, or by extension of a midline celiotomy incision lateral to the xiphoid process. Hernias are unlikely to occur from dehiscence of diaphragmatic incisions or herniation through gaps remaining after transdiaphragmatic implantation of cardiac pacemaker electrodes.41 Mechanism for indirect injury to the diaphragm is suspected to be a sudden increase in intraabdominal pressure (IAP) with the glottis open. Normally, during quiet inspiration, the pleuroperitoneal pressure gradient varies from 7 to 20 cm H2O. On maximal inspiration, however, it increases beyond 100 cm H2O.64 The high pleural pressure provides some stabilization to the diaphragm. Application of force to the abdominal cavity with the glottis open increases the peritoneal-to-pleural gradient, and herniation of viscera is usually immediate after the diaphragm ruptures.30 Because of the nature of automobile trauma, multisystem injury and shock are potential complications in patients with traumatic diaphragmatic hernia. The thoracic cavity and organs are severely injured in more than 39% of dogs and cats with musculoskeletal trauma.88,97 Pulmonary contusion, pleural effusion, hemothorax, pneumothorax, and rib fractures are the most common of these injuries. About 2% of dogs with fractures have a diaphragmatic hernia.88 Male dogs 1 to 3 years old are at significantly greater risk for traumatic diaphragmatic hernia.15,92 With traumatic diaphragmatic hernia, the diaphragmatic costal muscles are more often ruptured than the central tendon, and the stronger crural muscles are seldom ruptured.2,92,110 Overall, left-to-right distribution is probably uniform in dogs and cats, with about 15% being bilateral or multiple.2,39,92,110 Whereas the orientation of tears in the costal muscle at surgery in dogs was circumferential (40%), radial (40%), or a combination (20%), cats had a preponderance of circumferential tears (59%) and fewer radial tears (18%).39 The liver is the organ most often herniated, being found in the thoracic cavity in 88% of patients.15,110 Other organs herniated, approximately in order of decreasing frequency, are the small intestine, stomach, spleen, omentum, pancreas, colon, cecum, and uterus.10,15,39,110 The extent and location of the diaphragmatic rent, together with anatomic proximity and length of supporting ligaments or mesentery of individual organs, have an influence on which abdominal organs herniate. In right-sided tears, the liver, small intestine, and pancreas tend to herniate, but on the left, herniation of the stomach, spleen, and small intestine is more common.39 Pathologic effects from diaphragmatic hernias result from effects on cardiorespiratory dynamics or on the herniated organs themselves. Herniated viscera can become inflamed, incarcerated, obstructed, or strangulated.15 These detrimental effects often result from pressure applied by the edge of the diaphragmatic tear as the organs pass over it or from formation of fibrous adhesions and strictures. Incarceration of the stomach and intestine in a diaphragmatic hernia may cause partial or complete obstruction to flow of ingesta. Gastric tympany may occur after stomach herniation. Unrelieved compression of caudal vena cava and lungs by distended organs is rapidly fatal.39,105 The consequences of obstruction of the gastrointestinal tract depend on the level at which the blockage occurs.67 Gastric outflow and proximal duodenal obstruction were reported in one dog to cause recurrent vomiting, which in turn resulted in dehydration, metabolic alkalosis, electrolyte derangements, altered cardiac electrical conduction, and muscle weakness.74 A severely compromised blood supply can also induce ischemic necrosis, intestinal perforation, and abscessation.48 Gastric dilatation volvulus has been reported in cats with traumatic diaphragmatic hernia.36 In right-sided hernias, one or more lobes of liver often move into the thorax. Liver herniation may occur with left-sided diaphragmatic defects as well. Major effects of liver herniation include hepatic venous stasis, hepatic necrosis, biliary tract obstruction, and jaundice. Bacterial proliferation in devitalized traumatized liver or herniated liver could also potentially occur, and vascular obstruction followed by systemic release of toxins after repositioning of liver lobes may be a concern. Although not well documented, endogenous Clostridia-like anaerobic bacteria are said to be normally resident in healthy canine liver, and they proliferate when the hepatic blood supply is curtailed, resulting in death in a few days unless penicillin is administered.60 Pleural effusion may develop with herniation of the liver into the pleural cavity. Normally, a gradation of pressure exists throughout the hepatic venous system. Portal vein pressures are the highest (8 to 12 mm Hg) followed by those in the intrahepatic sinusoids (3 to 4 mm Hg) and hepatic veins and caudal vena cava (0.5 to 1 mm Hg).85 Because of their low pressures and thin walls, the caudal vena cava and hepatic veins are easily compressed. With liver herniation, compression or kinking of these vessels results in occlusion to hepatic venous outflow. With increased hepatic venous or caudal vena caval pressure to 0.85 mm Hg beyond intrahepatic sinusoidal pressure, the involved liver lobes become congested.16,52,60 As a result, hepatic lymphatic vessels distend, and copious quantities of hepatic lymph are extravasated through the capsule of the liver. Depending on the location of the lobe, rapid accumulation of pleural fluid, pericardial fluid, ascites, or a combination, occurs.85 Hydrothorax and ascites develop in about 30% of animals with liver herniation15,111 and were reported to cause cardiac tamponade in a German shepherd with traumatic diaphragmatic hernia.58 The fluid is typically a modified serosanguineous transudate.76 Pleural effusion occasionally accompanies herniated viscera other than the liver.15 Hemothorax, chylothorax, bile pleuritis, and pneumothorax also can complicate hernia.11,15,27,51,73 Diaphragmatic rupture with concomitant biliary tract injury, bile peritonitis, and bile pleuritis has been reported in a dog.27 Hemiurothorax was reported in a cat with diaphragmatic hernia and kidney prolapse.93 Two cats presented primarily with icterus as a result of extrahepatic biliary obstruction complicating chronic diaphragmatic hernias.21 Dyspnea is the most common clinical sign in diaphragmatic hernia. In addition to a lack of a functioning diaphragm, lung compression, and shock, respiratory insufficiency may result from dysfunction of the chest wall, pleural space, lungs, airway, and cardiovascular system.15 All of these pathophysiologic alterations are interrelated.15 Parietal pleural contact with the lungs is normally maintained by negative intrapleural pressure of 0.5 to 1.0 mm Hg. With rupture of the diaphragm, parietal pleural contact with the lungs is lost.64 Pleural and peritoneal pressure equalize, and the abdominal and thoracic wall muscles take over the function of the diaphragm. Pain and mechanical factors associated with concurrent chest wall contusion, rib fractures, and flail chest limit thoracic expansion. Compression and atelectasis of the lung lobes by herniated organs, fluid, or air in the pleural cavity cause hypoventilation, ventilation-perfusion mismatch, and hypoxia. Trauma that resulted in the hernia may also cause shock, reduction in effective perfusion, tissue hypoxia, and multiorgan failure. Cardiac dysrhythmias, especially ventricular tachycardia, are present in about 12% of hernia patients and may decrease tissue perfusion and aggravate shock.15 Pulmonary function deteriorates further in shock with increase in pulmonary vasculature permeability, pulmonary edema, and hypoventilation, which cause further ventilation-perfusion mismatching. Because affected patients may be on the edge of fatal cardiopulmonary decompensation, great care is needed in their handling.48 Clinical Signs.: A high index of suspicion for diaphragmatic hernia needs to be maintained in trauma patients so the condition is not overlooked. The reported interval between trauma and diagnosis ranged from hours to 6 years, with a mean of several weeks.15,39,92 Acute trauma patients may have severe injuries other than the hernia and generally have signs of hypovolemic shock. Although no pathognomonic signs have been identified for diaphragmatic hernia, respiratory signs predominate, and 38% of affected animals have dyspnea and exercise intolerance.92 Some animals adopt a sitting or standing position, with the elbows abducted and head extended.48 Vomiting, dysphagia, diarrhea, and constipation may indicate gastrointestinal involvement. Other signs include lethargy, weight loss, and difficulty in lying down.92 Respiratory distress caused by increased IAP during parturition has been reported in a Chihuahua, necessitating emergency cesarean section.55 Physical Examination.: Findings on physical examination are normal in some animals. The abdomen may appear tucked up or empty, especially in chronic cases.39 On auscultation, heart sounds are muffled, abnormally positioned, or more intense on the side contralateral to the hernia.92,99 Whereas pleural effusion causes a hyporesonance of the chest wall on percussion, gastric tympany causes hyperresonance. Some animals may have auscultable borborygmi from herniated viscera, but this finding is not reliable.48 With experience, thoracic palpation for localization of the cardiac apex beat is 80% accurate in determining the side of the hernia.92 Radiographs.: Radiography is the most useful test for diagnosis of diaphragmatic hernia. Thoracic radiographs should be taken of all patients that have experienced serious trauma, especially those with any evidence of dyspnea or fractures.88,97 Undue restraint and struggling should be avoided, however, because animals with diaphragmatic hernia may already have severe respiratory and cardiovascular dysfunction. On lateral radiographs, the normal diaphragmatic silhouette has a curved profile, with the dome-shaped cupula in contact with or overshadowing the cardiac silhouette.41 The crura are parallel in right lateral recumbency but cross each other in left lateral recumbency. In the ventrodorsal view, the diaphragm casts either a single-domed shadow or a triple-domed cloverleaf shadow, which includes the crura. Radiographic appearance of the diaphragm is mainly influenced by respiration, gravity, conformation, and radiographic positioning.41 The single most useful view for diagnosis of diaphragmatic hernia is the lateral projection.95 Partial loss of the normal line of the diaphragm is present in 66% to 97% of animals with diaphragmatic hernia; this finding alone is not diagnostic and needs to be interpreted in conjunction with other findings.62,95 Visualization of viscera in the thorax is diagnostic (Figure 85-3). In one report, the small intestines appeared herniated on 61% of radiographs and spleen, liver, or stomach in 35%.95 Other abnormalities detectable on lateral radiographs include an obscured or displaced cardiac shadow. Additionally, the pylorus and duodenum may be pulled cranially from traction on the gastrohepatic ligament by a herniated liver even though they may not be prolapsed through a diaphragmatic tear. Lung lobe collapse and pleural fluid were more readily detectable on the dorsoventral view and are found in 20% to 31% of cases.76,95,110 When present, pleural fluid may complicate the diagnosis by obscuring other radiographic details. Thoracocentesis may be performed for fluid analysis, to alleviate hypoventilation, and to improve radiographic quality. This can be a frustrating exercise, however, and diagnostic radiographs may not be obtained even after removal of large volumes of fluid.95 Alternate radiographic views (positional radiography) may assist detection of visceral shifting in animals with diaphragmatic hernia by allowing comparison with standard views. In the erect ventrodorsal projection, the animal is held in a standing or sitting position, and a horizontal radiograph is taken in an attempt to demonstrate reduction of herniated viscera back into the abdominal cavity.109 Contrast Studies.: Although rarely indicated, diaphragmatic hernia may be diagnosed with contrast studies of the gastrointestinal tract. The presence of barium-filled viscera within the thoracic cavity is definitively diagnostic for the condition. In one study, contrast radiographs were helpful in making a diagnosis in 11 of 14 dogs in which initial plain radiographs were nondiagnostic.95 Barium studies of the gastrointestinal tract may be nondiagnostic because of partial gastrointestinal obstruction and subsequent delayed transit of the contrast medium. Other radiographic imaging techniques that have been recommended historically include pneumoperitonography, positive-contrast pleurography, portography, cholecystography, and angiography.109 If the diaphragmatic defect is plugged by viscera, false-negative results are obtained by pneumoperitonography and positive-contrast peritoneography.20,91 Otherwise, positive-contrast peritoneography is a sensitive technique for diagnosis except when contrast medium is diluted by pleural or ascitic fluid.91 Ultrasonography.: Ultrasonography was shown to have an accuracy of 93% for the diagnosis of diaphragmatic hernia.89 One false-negative result was reported in a cat in which adhesions between the liver and the diaphragm disguised the diaphragmatic rupture, and a false-positive result was reported in one dog in which a pulmonary abscess was misdiagnosed as the stomach.89 Ultrasonography is particularly useful in animals with pleural effusion because fluid is an excellent ultrasound-transmitting medium. By positioning the transducer head at an intercostal space just cranial to the expected location of the diaphragm and scanning forward, the herniated organs can be identified and differentiated from pleural fluid (Figure 85-4). Alternatively, the caudal thorax can be examined ultrasonographically for diaphragmatic lesions through the subcostal approach using the liver or herniated organs as a window.94 In this view, the diaphragm is oriented perpendicular to the ultrasound beam and can be identified adjacent to the cranial surface of the liver.94 In some patients, remnants of the torn diaphragmatic muscle can be seen in the anechoic pleural fluid, moving in unison with respiratory motion.94 The liver and spleen have characteristic echogenic patterns; location of these organs adjacent to the heart without an intervening diaphragmatic line may indicate a diaphragmatic hernia. With ultrasonography, the diaphragmatic rent or herniated organs cannot always be identified; however, ultrasonography can be used to detect viscera in abnormal positions without the need to drain off the pleural fluid. Timing of Surgery: Surgical correction of traumatic diaphragmatic hernia is performed at the earliest opportunity in a stable patient, taking into account other injuries.15 An early report suggested that timing of surgery affected survival rates, and two significant peaks in mortality were noted.15 Survival rates were 67% for 40 dogs operated on within 24 hours and 37% for 8 dogs operated on after 1 year.15 Whereas death in the early group was entirely a result of shock and trauma, death in the late group was largely unrelated to the hernia. By delaying surgery until 1 to 3 weeks after trauma, survival rates were greater than 90%.15 In a more recent case series, no adverse effects were associated with early surgery. Of 63 patients that underwent surgery within 24 hours of trauma, 59 (93.7%) were discharged alive from the hospital.40 These results suggest that surgery should be undertaken as soon as the patient has been adequately stabilized after the initial injury. Continuous monitoring of animals with diaphragmatic hernia in the interval between diagnosis and surgery is mandatory because of the risk of sudden respiratory decompensation. Delays in surgery place the patient at risk of life-threatening hypoventilation from compression of the lungs by the abdominal viscera. This situation can develop rapidly in animals with left-sided diaphragmatic rupture and herniation of the stomach. Acute gastric gaseous distension effectively produces a tension pneumothorax. Emergency decompression of the stomach with a hypodermic needle inserted through the left chest wall into the stomach is performed followed by surgery.92 Alternatively, passage of an orogastric tube may be attempted.
Diaphragmatic Hernias
Anatomy
Embryology
Physiology
Surgical Approaches
Hernias
Traumatic Diaphragmatic Hernia
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Diaphragmatic Hernias
Only gold members can continue reading. Log In or Register to continue