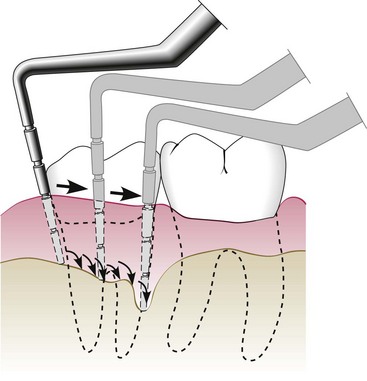
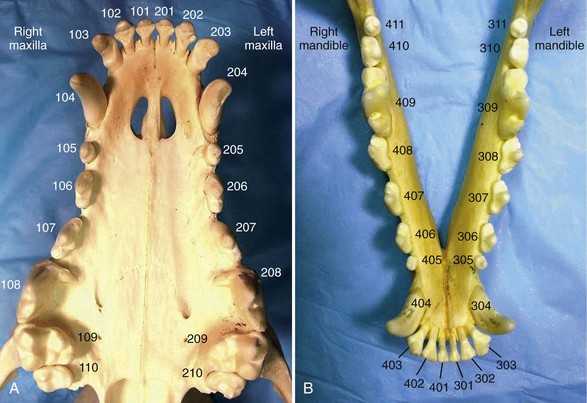
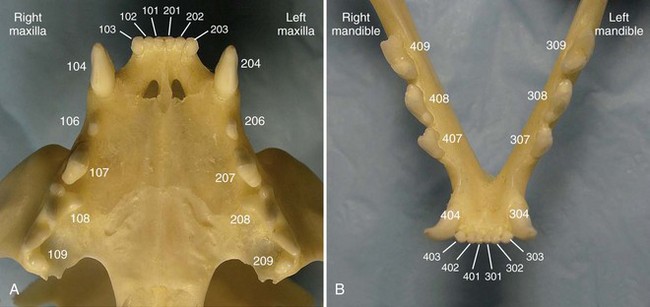
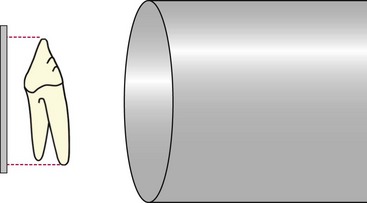
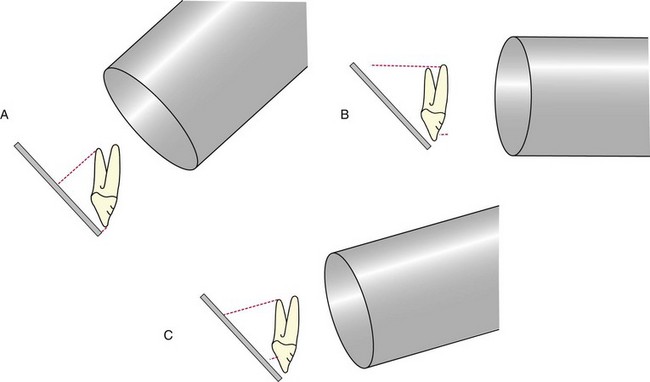
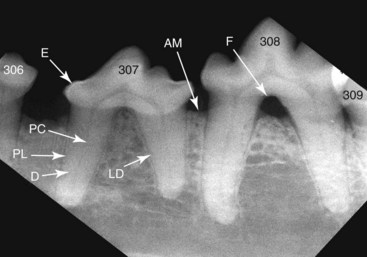
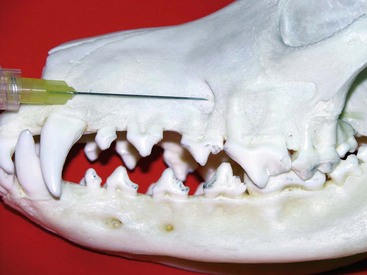
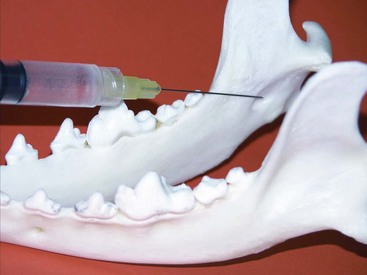
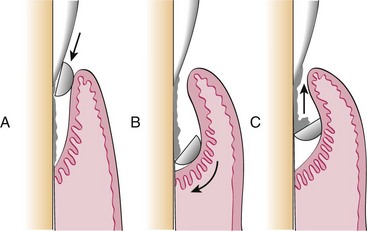
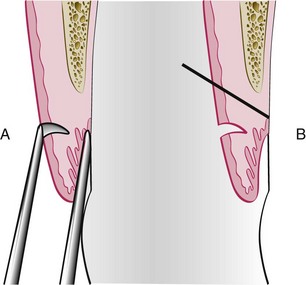
Chapter 66 Clinical signs may not be apparent to the owner until the disease is well advanced. A full patient history is imperative and should include questions about appetite, eating and drinking patterns, prehending, chewing, swallowing, access to treats and chew toys, medications (and responsiveness to medications), and the animal’s environment. The presence of halitosis, preferential chewing on one side of the mouth, inability or reluctance to open or close the mouth, dropping food from the mouth, drooling of saliva, inappetence, weight loss, sneezing, nasal discharge, pawing at the face, and other abnormal clinical signs should be assessed. It is often helpful for the examiner to watch the animal eat and drink if the owner reports any abnormal behavior during eating and drinking.21,32 Examination for systemic disease is important to assess anesthetic risk or to determine the possibility of dental and oral lesions occurring secondary to a systemic condition. Preanesthetic blood tests should include a complete blood count and biochemical profile. Clotting factor tests may be indicated occasionally. Urinalysis and cardiac examination are performed as necessary. Cats with acute or chronic oral inflammation (beyond gingivitis) should be tested for feline leukemia virus (FeLV), feline immunodeficiency virus (FIV), and, occasionally, feline bartonellosis.21,32 The skilled operator examines the eyes, ears, nose, masticatory muscles, face, lips, and jaws. Extraoral tissues are evaluated to determine the presence of airflow from each nostril (one is closed with a thumb while airflow from the other nostril is evaluated); discharge from oral, nasal, and ocular orifices and sinus tracts; external lacerations; asymmetry and facial swellings; presence of exophthalmos or enophthalmos; ability to retropulse the eye globes (by gently pushing them into their orbits); and swelling or atrophy of masticatory muscles. The jaws, intermandibular tissues, zygomatic arches, and neck should be palpated for pain, asymmetry, discontinuity, crepitus, and emphysema. The range of mouth opening is assessed, which also provides information about abnormalities of the temporomandibular joints and muscles of mastication.21,32 The skin and mucocutaneous areas should be examined before opening the mouth. The labial and buccal mucosa of the lips and cheeks is examined by lifting the animal’s upper and lower lips. The oral mucosa should be moist, intact, and nonpainful on touch. It may or may not be pigmented. The mucogingival junction separates the alveolar mucosa from the gingiva as a visible line. Whereas the alveolar mucosa is elastic and movable, the gingiva is very dense and cannot be moved from the underlying bone. The color, size, location, thickness, surface characteristics, and symmetry of any oral lesions should be noted.21,32 Opening the mouth is greatly facilitated when the animal’s head is rotated dorsally. In the dog, the muzzle is held with one hand, and the examiner places the thumb of that same hand just caudal to the maxillary canine teeth, while rotating the head dorsally. In the cat, one hand holds the entire head (in the area of the zygomatic arches), then rotates it dorsally. The other hand then opens the mouth by pushing the lower jaw ventrally. The ventral surface of the tongue and sublingual tissues can be inspected by carefully pushing the thumb of the second hand into the intermandibular area. This raises the tongue. The examiner may also push the tongue ventrally with one or two fingers of that same hand to examine the dorsal surface of the caudal tongue portions, the soft palate, tonsils, and pharynx. The hard palate can be inspected and palpated with a finger. The brave examiner may extend that same finger caudally onto the soft palate (most animals will open the mouth even farther rather than close it) to assess any abnormalities of the nasopharynx.21,32 Obvious lesions such as fractured teeth, moderate to severe periodontal disease, stomatitis, and oral masses can often be identified in the conscious patient. However, sedation or general anesthesia is usually required for a thorough intraoral examination and application of more sophisticated diagnostic tools. The structural integrity of teeth is assessed with a dental explorer, whose pointed tip can detect irregularities of the crown surface. It may also be used to determine whether pulp exposure has occurred in a fractured tooth. The alveolar mucosa over the roots of the teeth should be inspected and palpated for the presence of swellings and sinus tracts, which may indicate endodontic disease or neoplasia.21,32 The periodontal probe is one of the most important hand instruments in veterinary dentistry and is invaluable for an accurate periodontal examination. The probe is gently inserted into the space between the tooth and the gingiva (gingival sulcus), and measurements are obtained around the entire circumference of each tooth (Figure 66-1). The gingival sulcus of cat teeth should not be deeper than 0.5 mm, and in dog teeth it should not be deeper than 3 mm. Deeper measurements indicate the presence of a periodontal pocket or, in the case of gingival enlargement, a pseudopocket. Other periodontal parameters include plaque and calculus (tartar) accumulation, gingival index, gingival recession or enlargement, total attachment loss, tooth mobility, and missing teeth.32,55 Any other abnormalities should be recorded, including persistent (retained) deciduous teeth, supernumerary teeth, dental or skeletal malocclusion, circumscribed ulcers, widespread oral inflammation, oral masses, lacerations, and other signs of trauma. Dental and oral charts represent legal documents and should be included as essential parts of every patient’s medical record.25 Knowledge of deciduous and permanent dentition in the cat and dog is helpful during verbal or written communication between veterinary health care providers (Boxes 66-1 and 66-2). Using the modified Triadan system, each jaw quadrant is numbered as follows: • Right maxillary quadrant = 100 (500 when referring to deciduous teeth) • Left maxillary quadrant = 200 (600 when referring to deciduous teeth) • Left mandibular quadrant = 300 (700 when referring to deciduous teeth) • Right mandibular quadrant = 400 (800 when referring to deciduous teeth) Each tooth is assigned a number within each quadrant. Beginning with 01 for the first incisor, teeth are consecutively numbered from mesial (the surface of the tooth that faces the midline of the dental arch) to distal (the surface of the tooth that faces away from the midline of the dental arch). Because the dog has a full set of permanent premolars, tooth numbering is consecutive from 01 to 10 on the upper jaw and from 01 to 11 on the lower jaw (Figure 66-2). When quadrant and tooth number are taken into consideration, three numbers are used to identify a specific tooth. For example, the permanent right maxillary canine is referred to as tooth 104. The deciduous right maxillary canine is tooth 504.32 Several premolars and molars have been evolutionarily lost in the permanent dentition of the domestic cat. The “rule of 04 and 09” refers to the fact that the canine (04) and the first molar (09) are present as reference teeth to allow counting forward or backward when numbering teeth. For example, the permanent mandibular first (05) and second (06) premolars are absent in the cat. Knowledge that the mandibular first molar (09) is the largest cheek tooth of the mandible allows one to count forward and identify the mandibular premolar closest to the canine as the 07 tooth (Figure 66-3). As an example, the permanent left mandibular third premolar is tooth 307. The permanent right maxillary second premolar is tooth 106.32 Dental radiographs should always be obtained before tooth extraction is performed, to assess alveolar bone health and variations in root anatomy and to determine the presence of dentoalveolar ankylosis or replacement resorption of roots that could complicate the extraction procedure. Furthermore, radiographs are an extremely important part of every endodontic procedure and are essential in assessing treatment outcome at follow-up visits. In addition to dental-related conditions, most jaw pathology can be satisfactorily assessed with size 2 and 4 dental film and intraoral imaging technique. Size 4 dental film can also be utilized to evaluate diseases of the nasal cavity, orbit, zygomatic arch, mandibular ramus, temporomandibular joint, and tympanic bulla in cats and small dogs.12,41 Dental radiography machines can be portable or wall-mounted and have extension arms that allow vertical, horizontal, and rotational movement of the tube head without changing the patient’s position. Exposure time often is the only adjustment to be made and depends on the size of the patient and the tissue thickness to be imaged. Dental films can also be used with a standard radiography machine using a technique of 100 mA, a film focal distance of 12 inches, and an exposure time of Dental radiography film is a nonscreen film that provides greater detail than the screened film typically utilized with standard radiography machines. It is available in several sizes and speeds, with sizes 0, 2, and 4 as D film (ultra speed) most commonly utilized. The films are stored within a moisture-resistant packet, and black paper is present on either side of the film. A layer of lead foil is located at the back of the packet next to the tab opening; this protects the film from secondary radiation (which may cause the film to fog). A dimple is located in one corner of the film packet. The convex (raised) surface of the dimple must face the radiographic beam during exposure. The dimple is used to distinguish on processed radiographs the images obtained from left and right sides of the mouth. Dental rapid developer and fixer are utilized for film processing. These solutions are placed in small containers within a chairside film processor. The containers contain the following solutions (from left to right): developer, water, fixer, and water.12,13,22,41 It is best to briefly leave the room while radiographs are exposed. If this is not possible, one should stand at least 6 feet from the radiographic cone and at a 90 to 135 degree angle to the tube head. Gauze may be utilized to hold the films in proper position within the mouth of an intubated animal. The parallel technique is relatively easy to accomplish, with the film placed parallel to the tooth and the radiographic beam directed perpendicular (90 degrees) to the film and tooth (Figure 66-4). Anatomic limitations make this technique useful only for imaging the mandibular molars, the caudal mandibular premolars, and the nasal cavity. The bisecting angle technique is utilized to minimize distortion when obtaining radiographs of all maxillary teeth and mandibular canines, incisors, and rostral premolars (Figure 66-5). The film is placed as close to the teeth as possible. The angle that is formed between the long axis of the teeth and the plane of the film is bisected by an imaginary line. The tube head is positioned perpendicular to this imaginary line.12,13,22,41,45,46 The operator should ensure that the lid of the chairside film processor is closed. One hand holds the film, the other hand a film clip. Both hands are slid through the front windows of the processor. The exposed film is removed from the packet and placed in the film clip. First, the film is placed into developer for about 30 seconds; then, it is briefly rinsed in water and is placed in fixer for at least 60 seconds before viewing. After another brief water rinse, the film may be viewed using a dental view box. After initial viewing, the film should be placed for another 15 minutes in the fixer solution. This is followed by thorough rinsing under running water for 20 minutes before drying on air. Films dried overnight can be stored in a labeled envelope and kept as part of the patient’s medical record.12,13,41,49 To view dental radiographs in labial mounting, the processed film is placed on the view box so that the raised dot is facing the viewer.43 It is determined whether the image is of the upper or lower jaw and of the left or right side. All three-rooted teeth are located in the upper jaw. The palatine fissure is also located in the upper jaw. The ventral mandibular cortex or mandibular canal is often visible on lower jaw films. Films of teeth of the left jaw are placed on the right side of the view box, and those of the right jaw on the left side of the view box. Each film should be rotated so that the crowns of the maxillary teeth face downward and those of the mandibular teeth face upward. The following components of the tooth and its supporting structures should be evaluated: enamel, dentin, cementum (visible radiographically only when thickened), alveolar margin, periodontal ligament space, lamina dura, and pulp cavity (Figure 66-6). The mandibular canal is visible as a radiolucent tubular structure in the mandible. Mental foramina and palatine fissures may sometimes be mistaken for periapical pathology.12,22,41 Local and regional anesthesia is commonly performed in cats and dogs with oral disease and is an effective measure in minimizing medical expenses. It allows reduction in the concentration of an inhalant anesthetic, which minimizes complications from hypotension, bradycardia, and hypoventilation. Patients maintained on lower anesthetic concentrations consequently recover more quickly and with fewer complications. Furthermore, local and regional anesthesia continues to provide analgesia in the postoperative period, thus enhancing patient comfort and decreasing the need for systemic administration of analgesics.1,17,28,61 Local anesthesia (infiltration anesthesia) refers to the injection/application of a local anesthetic solution into/onto tissues at a surgical site, for example, along planned incisions. Topical anesthetic gels may provide temporary relief from superficial pain, but their effects are short-lived. Splash block (wound irrigation) refers to dropping a local anesthetic solution directly onto an incision or wound, for example, into the nasal cavity after a maxillectomy before closure of the surgical site. Regional anesthesia (nerve block) refers to injection of a local anesthetic solution around a major nerve utilizing 27-gauge, Commonly used local anesthetics include bupivacaine 0.5% (effective for 6 to 10 hours), mepivacaine 2% (effective for about 4 hours) and lidocaine 2% without epinephrine (effective for less than 2 hours). The onset time for analgesia is longer with longer-acting local anesthetics (a few minutes for lidocaine, up to 30 minutes for bupivacaine). The total maximum dosage for bupivacaine in cats and dogs is 2 mg/kg, and for lidocaine in the dog 5 mg/kg and in the cat 1 mg/kg.25,28 A total of 5 mg of bupivacaine is present in 1 mL of a 0.5% solution (bupivacaine 0.5%). The infraorbital nerve block is given at the infraorbital foramen or inside the infraorbital canal (Figure 66-7). Areas blocked include the incisive bone and maxilla, maxillary incisors, canine, and premolars/molars (depending how far the needle is advanced into the infraorbital canal) and adjacent soft tissues. The inferior alveolar (mandibular) nerve block can be given intraorally (at a relatively flat angle through the alveolar mucosa at the lingual surface of the mandible) or extraorally (through the skin at an unnamed notch at the ventrolingual surface of the mandible) (Figure 66-8). Areas blocked include the mandibular body and all mandibular teeth and adjacent soft tissues. Periodontal disease affects most adult cats and dogs and refers to inflammation and infection of the periodontium (gingiva, periodontal ligament, alveolar bone, and cementum) caused by plaque bacteria and the host’s response to the bacterial insult. Its systemic effects have been well documented in human beings (heart disease and stroke, diabetes, respiratory disease, and increased risk of premature delivery and low-birthweight infants) and are being increasingly investigated in cats and dogs.8,50 Gingivitis is reversible, affecting the gingiva only. As inflammation continues, the gingiva detaches from the tooth, creating a periodontal pocket, and a shift occurs in the gingival flora from a Gram-positive aerobic to a Gram-negative anaerobic spectrum. Periodontitis is the more severe form of periodontal disease, affecting all periodontal tissues and resulting in attachment loss, gingival recession, periodontal pocket formation, and alveolar bone loss. Bone loss is usually irreversible, causing the tooth to become mobile and ultimately to exfoliate.19,20 The goal of periodontal therapy is elimination of supragingival and subgingival plaque and reduction of periodontal pockets. Medical therapy includes the use of topical rinsing solutions (e.g., dilute chlorhexidine) or systemic antimicrobials (e.g., amoxicillin/clavulanic acid, clindamycin, spiramycin/metronidazole, doxycycline). Because of potential side effects and/or the possibility of bacterial resistance, systemic antimicrobials should be used only in selected cases to serve as an adjunct to local treatment.10 Mechanical therapy can be categorized as two different concepts: closed and open treatment. Closed treatment (professional dental cleaning) is indicated when periodontal pocket depths do not exceed 4 to 5 mm in the dog 1 and 2 mm in the cat. First, the teeth are scaled with power scalers. Then, hand scalers are used to remove residual calculus in pits, fissures, and developmental grooves of the crowns. Subgingival scaling (cleaning and planing of the root surface) is performed with hand curettes (Figure 66-9), which can also be used for gingival curettage that removes the inflamed and infected soft tissue lining of the periodontal pocket. Once scaling is completed, the tooth surfaces are polished with fine polishing paste and a rubber cup on a prophy angle that is attached to a low-speed handpiece. Debris and polishing paste are rinsed from the tooth surface with water from an air/water syringe or a dilute chlorhexidine solution. Low-dose doxycycline gel may be inserted into cleaned periodontal pockets larger than 4 mm after root planing and gingival curettage.19,20 Open treatment is indicated when pocket depths exceed 5 to 6 mm in the dog and 2 to 3 mm in the cat and is performed following reflection of a gingival or periodontal flap. The modified Widman flap procedure utilizes an internal bevel incision slightly apical to the gingival margin and down to the alveolar bone. However, no vertical incisions are made. The partially mobilized gingival flap is not reflected beyond the mucogingival junction with this flap design. Greater visibility in the surgical site is achieved by elevation of a periodontal flap beyond the mucogingival junction. This usually requires that one or two vertical releasing incisions are made into gingiva and alveolar mucosa. Osseous surgery and placement of implants are possible with this flap design. The flap is repositioned at various locations (original, coronal, or apical).19,20 Some variation exists in the use of procedural terminology. Human periodontal texts refer to gingivectomy as excision of gingiva to eliminate periodontal pockets (including pseudopockets in patients with gingival enlargement) and include reshaping as part of the technique. In comparison, gingivoplasty is reshaping of the gingiva to create physiologic contours, with the sole purpose of recontouring the gingiva in the absence of pockets.67 At least one veterinary text refers to excision of gingiva to remove gingival pockets as gingivoplasty, stating that gingivectomy is an inappropriate term because gingiva is never removed in its entirety.21 Excision of gingiva can also be performed in crown-lengthening procedures and exposure of subgingival dental defects. Gingivectomy and gingivoplasty are contraindicated when less than 2 mm of gingiva is attached, and when horizontal or vertical bone loss extends beyond the mucogingival junction. The depth of the pocket is marked on the outer gingival surface using a periodontal probe or a pocket marker to create bleeding points. An external bevel incision is made slightly apical to the bleeding points with the blade held at a 45 degree angle to achieve a natural gingival contour (Figure 66-10). At least 2 mm of attached gingival tissue must be preserved after the procedure is completed.34 Lateral sliding flaps and free gingival graft techniques are available for treatment of gingival clefts.52
Dentistry for the Surgeon
Oral Examination
History and Clinical Signs
Extraoral Examination
Intraoral Examination
Tooth Formula in Dogs and Cats
Dental Radiography
Equipment
 second, with the kVp varying from 60 to 70, depending on patient size. Dental radiography films, a chairside film processor, and a view box complete the needed equipment. Digital imaging utilizes sensor pads or phosphor plates instead of films that transfer the image to a computer. The digital system requires less radiation to produce an image, which may be modified with software programs.12,13,41,44,47
second, with the kVp varying from 60 to 70, depending on patient size. Dental radiography films, a chairside film processor, and a view box complete the needed equipment. Digital imaging utilizes sensor pads or phosphor plates instead of films that transfer the image to a computer. The digital system requires less radiation to produce an image, which may be modified with software programs.12,13,41,44,47
Obtaining Radiographs
Processing Radiographs
Interpreting Radiographs
Local and Regional Anesthesia
 inch needles on 1 mL syringes (22-gauge needles when going through the skin). This procedure is most commonly performed in dentistry and oral surgery for the maxillary nerve, infraorbital nerve, major palatine nerve, inferior alveolar nerve (mandibular nerve), and middle mental nerve.25,28,61
inch needles on 1 mL syringes (22-gauge needles when going through the skin). This procedure is most commonly performed in dentistry and oral surgery for the maxillary nerve, infraorbital nerve, major palatine nerve, inferior alveolar nerve (mandibular nerve), and middle mental nerve.25,28,61
Local Anesthetics
Specific Nerve Blocks1,25,28,61
Periodontal Disease
Periodontal Therapy
Gingival Surgery
< div class='tao-gold-member'>
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Dentistry for the Surgeon
Only gold members can continue reading. Log In or Register to continue