22 Deep corneal ulcer
CLINICAL EXAMINATION
The ophthalmic examination should include measuring aqueous tear production. If the eye is very painful, or the ulcer is very deep and you are concerned about corneal rupture, then perform the Schirmer tear test on the fellow eye only. Acute keratoconjunctivitis sicca is an under-recognized cause of sudden onset, deep corneal ulceration in the dog (see Case example 16.2). The eye is assessed for vision, and the pupil should be checked – often some miosis is present representing a reflex uveitis and this should be addressed when formulating a treatment plan. A frank uveitis with aqueous flare or even hypopyon can be present in conjunction with deep corneal ulceration, especially if bacterial infection is present. Careful evaluation of the conjunctival sac, including behind the third eyelid, should be undertaken since foreign bodies can be retained here. Intrinsic factors causing the ulcer, such as ectopic cilia or entropion, should also be looked for (Figure 22.1).
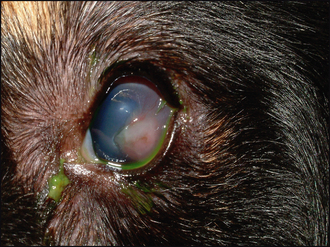
The ulcer is usually obvious as a defect or crater in the cornea (Figure 22.2). It can be assessed for depth both before and after staining with fluorescein. It is important to flush out excess dye with sterile saline to prevent pooling in the defect which can confuse the interpretation of the test. The exposed stroma will retain fluorescein, while Descemet’s membrane does not. Thus a deep ulcer which does not stain is likely to suggest a descemetocoele which should be treated as an ocular emergency. If the ulcer is actually healing, then the bottom of the lesion might not take up dye if the epithelium has fully covered all the stroma. The stromal edges are likely to be more gently sloped toward the depth of the lesion rather than being almost vertical when recently ulcerated.
The depth of the ulcer is important when formulating a treatment plan. Also of importance is the presence or absence of blood vessels. These grow from the limbus towards the damaged cornea at the rate of about 1 mm per day. This can be used to determine the length of time the lesion has been present. If the blood vessels are getting close to the ulcer, then medical management might be a feasible option. Some corneal oedema is often present around deep corneal ulcers so a grey ring to the lesion is commonly seen. This should be differentiated from the keratomalacia seen in melting ulcers (see Case example 23.2). In this instance the cornea will be grey and gelatinous in appearance, and when examined from the side the outline of the cornea will be distorted (keratoconus). Blinking and tear film distribution should be evaluated in all cases of deep corneal ulcer. Brachycephalic breeds often have some degree of lagoph-thalmos, and corneal exposure combined with poor or incomplete blinking can compromise healing.
CASE WORK-UP
Only limited case work-up is usually required for deep corneal ulcers since the diagnosis is easily made on ophthalmic examination, and unless multiple trauma has occurred (e.g. dog fights or road traffic accidents), further systemic evaluation is not normally required. As mentioned in the section above on the clinical examination, Schirmer tear test readings should always be taken. This is particularly important if a central descemetocoele is present since acute keratoconjunctivitis sicca is an important, and often forgotten, cause for these (see Chapter 16). If there is a mucopurulent or purulent ocular discharge, a swab should be taken for bacterial culture and sensitivity. Samples for cytology should also be considered. Treatment plans can be drawn up once the specific cause of the ulcer is identified.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree