25 Corneal foreign body
CLINICAL EXAMINATION
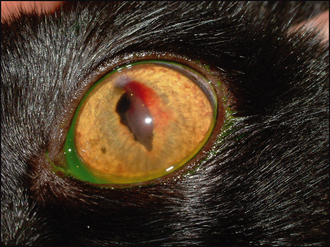
In addition to identifying the presence of the foreign body, it is important to check the rest of the eye. This will include examining beneath the nictitans membrane – fragments of plant matter can easily lodge here as well as in the cornea and should not be overlooked. A reflex uveitis is likely to be present such that the pupil is miotic. If the foreign body has perforated the cornea, then hyphaema and aqueous flare might be present (Figure 25.1). Viewing the patient’s eye from the side, and comparing it to the normal eye, will help to tell if the anterior chamber is of normal depth – it can be more shallow than usual if perforation has occurred and aqueous leakage has followed.
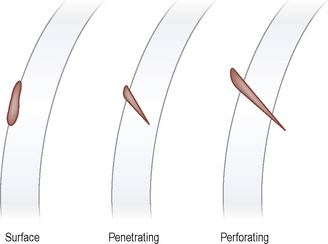
It will be clear from this description that it is important to assess the location of the foreign body within the cornea. This can be divided into surface, penetrating and perforating, in increasing order of seriousness (Figure 25.2). As the name suggests, a surface foreign body will sit on or in the epithelium. The eye is likely to be uncomfortable, rather than very painful, and only mild intraocular signs (such as slight miosis from a reflex uveitis) will be present. Penetrating foreign matter will be embedded within the stroma of the cornea. Some ulceration is likely around the entry site (check with fluorescein dye). If the foreign matter has broken off flush with the corneal surface, or is small and smooth in outline, the patient might be remarkably comfortable. Intraocular involvement will again be minimal.
CASE WORK-UP
Most foreign bodies are of plant matter – other items include paint flecks, metal filings and so on. Since plant matter can be a site of pathological bacterial (or even fungal) contamination, it is sensible to consider sampling for bacterial (± fungal) isolation and sensitivity testing. Doing this at the outset might result in a quicker resolution for the patient.