23 Complicated corneal ulcer
CLINICAL EXAMINATION
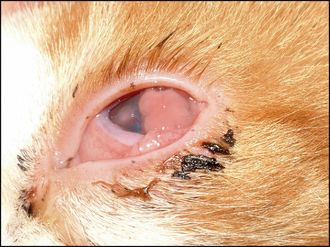
The ulcer should be obvious on clinical examination. However, the conjunctiva is likely to be hyperaemic, the nictitans membrane elevated and chemosis might also be present which could make visualization of the cornea difficult (Figure 23.1). Sometimes the ocular discharge will be extensive such that the eye is ‘glued’ shut. Gently bathing this away (and taking swabs for culture and sensitivity at the same time – but see below) will assist in examination. Overt ulceration might not initially be visible – there is likely to be significant vascularization (even granulation tissue) on the cornea, along with oedema, both of which obscure the actual ulcer. If areas of cornea appear gelatinous, and creamy or grey in colour, this could suggest keratomalacia or corneal melting (Figure 23.2).
CASE WORK-UP
The specific nursing for complicated corneal ulcers is similar to those for deep ulcers (see Chapter 22). Thus regular bathing of any discharge and the frequent application of topical medication are necessary. It is also important to alert the attending veterinary surgeon to any change in the condition of the patient, both of the eye itself and of the animal’s general demeanour – a sudden deterioration could require urgent surgical intervention.
EPIDEMIOLOGY
TREATMENT OPTIONS – MANAGEMENT
The first decision to be made should be: Is the eye salvageable? In some cases the cornea will be so severely compromised that the ulcer has ruptured, the iris has prolapsed and a panophthalmitis has resulted (Figure 23.3). If this is the case, then enucleation might be the best option for the patient. However, this is an irreversible decision and so one should be convinced that there is no alternative. If the eye has the potential for vision, enucleation is not advised. A positive dazzle response, together with a consensual pupillary light reflex (i.e. constriction of the fellow eye when a bright light is shone into the affected eye), are encouraging signs. If neither is present, then removing the eye might be indicated. If you are not sure whether the eye can be saved, referral should be considered. The welfare of the patient is paramount.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree