31 Chronic feline keratitis
CLINICAL EXAMINATION
In recurrent cases of FHV-1 systemic signs are usually absent but a full clinical examination should still be performed. Ocular signs of mild blepharospasm, increased lacrimation and some conjunctival hyperaemia are usually present. Schirmer tear tests should be performed before any discharge is cleaned away or samples taken. These can be elevated, normal or reduced. Conjunctival hyperaemia is normally present but chemosis is variable. Careful examination for evidence of ocular trauma or other inciting causes should be undertaken. Small corneal opacities, which may or may not stain positive with fluorescein dye, and fine vascularization are common findings. Larger superficial ulcers with irregular outlines and under-run edges are encountered and readily identified on careful examination (Figure 31.1).
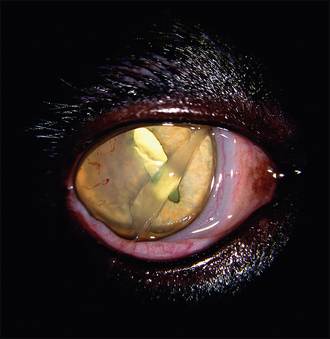
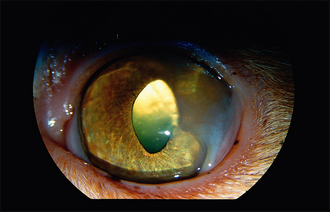
However, if FHV-1 is suspected as the cause for the keratitis then staining with rose Bengal should be considered. This is more sensitive than fluorescein at highlighting the small areas of epithelial devitalization and the demonstration of these dendritic ulcers is considered pathognomonic for FHV-1 keratitis (Figure 31.2). Careful evaluation of limbus is advised since acute herpetic infec tions in young cats will often result in limbal damage such that the neat dark line present between the clear cornea and white sclera is disrupted. Similarly, examination of the conjunctiva, especially around the nasolacrimal punctae and fornices, might reveal evidence of symblepharon (Figure 31.3), which is another frequent complication of FHV-1 and contributes to both chronic epiphora and corneal ulceration via reduced ocular and third eyelid motility as a result of the adhesions.
CASE WORK-UP
Thorough clinical examination will lead to the suspicion of FHV-1 and should rule out other causes of keratitis such as primary keratoconjunctivitis sicca or corneal sequestrum. However, as these are often associated with FHV-1, attempts at viral isolation or polymerase chain reaction (PCR) from both conjunctival and oropharyngeal swabs are advised since the treatment protocol might be changed if positive laboratory results are obtained. Corneal scrapes can be used for PCR and are probably more sensitive than conjunctival swabs since the samples are from the area most likely to be infected with virus. Cytology can be useful to rule out differentials such as proliferative keratoconjunctivitis. Some cats with herpetic keratitis are immunosuppressed and so screening for feline leukaemia virus (FeLV) and feline immunodeficiency virus (FIV) is sensible.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree