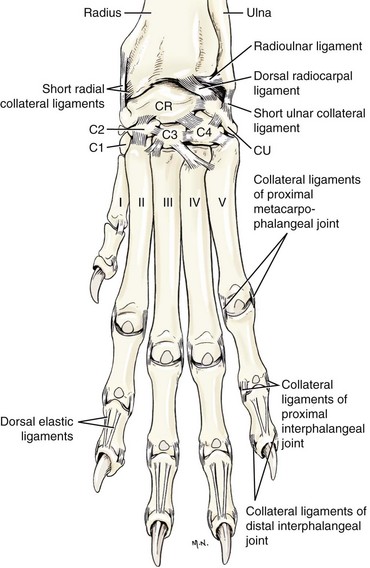
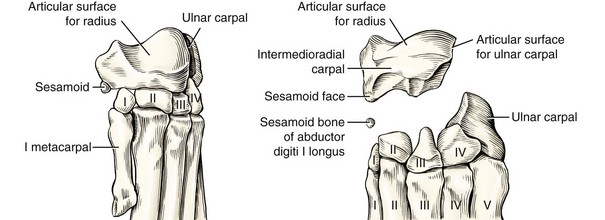
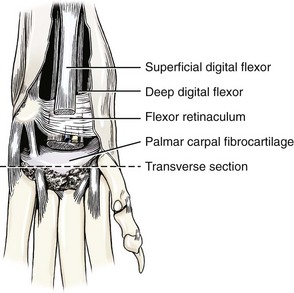
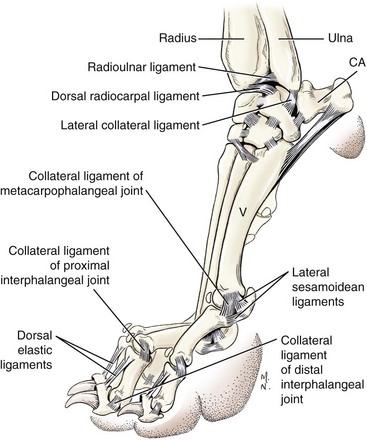
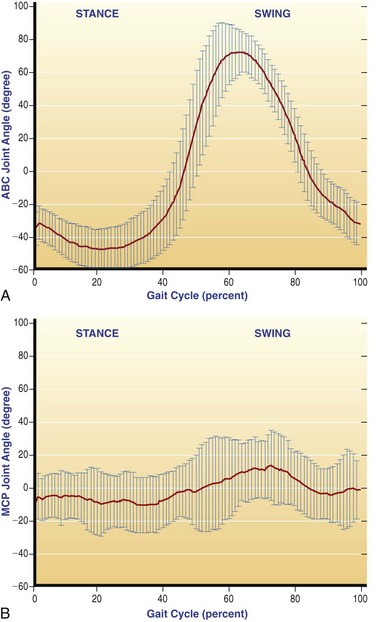
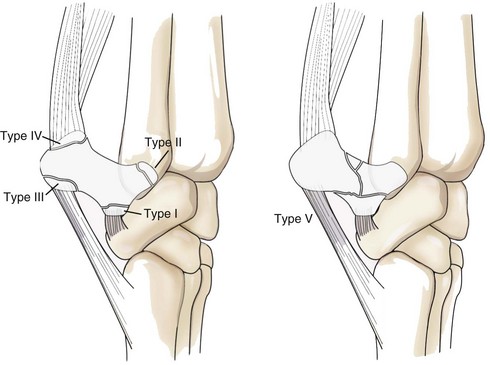
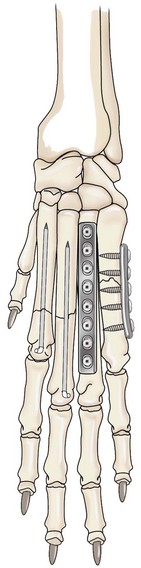
Chapter 56 The manus of the canine thoracic limb consists of the carpus, metacarpal bones, phalanges, and associated sesamoid bones.29 The manus has a complex anatomy that is well documented and studied. Yet the mechanism of injuries to these structures and best treatment options for those injuries in the dog and cat are poorly understood. The scientific literature regarding treatment options consists primarily of observational studies and biomechanical laboratory studies. Although these studies highlight diverse treatment options and theorize causation of the injuries, many questions remain regarding the best clinical approach for treating many of these conditions. In general, fractures that involve joint surfaces, ligament injuries that cause significant instability, and shearing injuries are approached surgically using the same principles applied when those injuries occur in other parts of the skeleton. General fracture repair techniques are presented in other chapters, but techniques unique to the carpus, metacarpus, and digits will be addressed in this chapter. The carpal bones are arranged in two rows.29,35,64,67,72 The radial carpal bone is the most medial bone of the proximal row. It is the largest of the carpal bones (it is the end result of the fusion of the radial, central, and intermediate carpal bones), and it articulates proximally with the radius, laterally with the ulnar carpal bone, and distally with all four of the numbered carpal bones. The ulnar carpal bone is the lateral bone of the proximal row. It articulates proximally with both the ulna and the radius, distally with the fourth carpal bone and the fifth metacarpal bone, medially with the radial carpal bone and with the accessory carpal bone on the palmar side. The accessory carpal bone is located at the caudal or palmar aspect of the ulnar carpal bone. It articulates with the styloid process of the ulna and the ulnar carpal bone (Figure 56-1). The distal row consists of the numbered carpal bones. The first carpal bone is the most medial and the smallest of the row, with a progressive increase in size of the second, third, and fourth carpal bones as they are located from medial to lateral. The first, second, and third carpal bones articulate proximally with the radial carpal bone alone, and the fourth carpal bone articulates proximally with the ulnar and radial carpal bone. Distally the first, second, and third carpal bones articulate with their corresponding metacarpal bones (metacarpal I, metacarpal II, and metacarpal III), and the fourth carpal bone articulates with metacarpals IV and V (Figure 56-2). The sesamoid bone located in the tendon of insertion of the abductor pollicis longus muscle on the medial side is considered the smallest bone of the carpus (although it is not counted as one of the seven bones that make up the carpus). It is located proximal and medial to the first metacarpal bone (see Figure 56-2). The carpus is a composite joint composed of all the articulations to which the seven carpal bones contribute.29 The antebrachiocarpal joint occurs between the distal radius and ulna and the proximal row of carpal bones. The middle carpal joint exists between the proximal and distal rows of carpal bones. The metacarpophalangeal joint exists between the distal row of carpal bones and the joint surface of the base of the metacarpal bones. The intercarpal joints exist between the individual bones of each row. The carpal joints as a whole act as a ginglymus (hinge) joint stabilized by short extra-articular and intra-articular ligaments, an articular disc (sometimes known as the radioulnar ligament that connects the radius to the ulna), palmar fibrocartilage, and the joint capsule. Antebrachial muscles and tendons cross all three joints of the carpus, but the carpal ligaments themselves do not.64,67 The ligaments present on the dorsal surface of the carpus are the radioulnar ligament (articular disc), the dorsal radiocarpal ligament, the short ulnar collateral ligament, and the short radial collateral ligament. The short ligaments that attach the radial carpal bone to the ulnar carpal bone, the radial and ulnar carpal bones to the numbered carpal bones, and the numbered carpal bones to each other and to the corresponding metacarpal bones are also visible (see Figure 56-1).29,72 On the palmar side, the short radial collateral ligament, the palmar radiocarpal ligament, and the palmar ulnocarpal ligament are the major deep ligaments of the carpus. The accessory carpal bone is attached distally to the proximal aspect of metacarpals IV and V by two separate ligaments (accessorometacarpal ligaments), and to the fourth and ulnar carpal bones by separate ligaments. Multiple short intercarpal ligaments unite the numbered carpal bones, and the numbered carpal bones to the metacarpal bones (Figure 56-3).29,64,72 The flexor retinaculum extends from the medial aspect of the accessory carpal bone to the radial styloid process, and distally to the radial and first carpal bones. The palmar fibrocartilage is attached to all the proximal carpal bones with the exception of the accessory carpal bone, to all the numbered carpal bones, and to the proximal palmar aspect of the base of metacarpal bones III through V (Figure 56-4).29 The five metacarpal bones are numbered from medial to lateral. Each metacarpal bone has a proximal base, a middle body, and a distal head.29 Metacarpal I is usually present, but it is not weight bearing because it is shorter than the level of the second metacarpophalangeal joint. Metacarpals II through V are all weight bearing, but metacarpals III and IV are longer than metacarpals II and V. Each metacarpal bone articulates with the proximal phalanx of the corresponding numbered digits and two palmar sesamoid bones. The metacarpophalangeal joint sesamoid bones are numbered from I through VIII from medial to lateral. Metacarpal I has one small palmar sesamoid that is not numbered. A dorsal sesamoid bone articulates with the head of the metacarpal bone at metacarpophalangeal joints II through V.29 Metacarpal I has its epiphysis at the proximal end, and metacarpals II through V have a single epiphysis at the distal end. Ossification is usually complete at 5 to 6 months of age.29,35,72 The intermetacarpal joints are joints between the proximal ends of adjacent metacarpal bones. The synovial membrane from the carpometacarpal joint contributes to uniting the bases of adjacent metacarpal bones.29 Distal to the carpometacarpal joint, the metacarpal bones are united for a variable distance by fibrous tissue known as the interosseous metacarpal ligaments. The five metacarpophalangeal joints are located between the distal metacarpal bones and their corresponding proximal phalanges and their palmar sesamoid bones. The metacarpophalangeal joint is united by a joint capsule and two collateral ligaments. The paired palmar sesamoid bones associated with metacarpals II through V are joined by the intersesamoidean ligament. The lateral and medial sesamoidean ligaments are attached to both the distal metacarpal bone and the proximal phalanx. The distal sesamoidal ligament is attached to the distal end of each palmar sesamoid to the proximal phalanx. Each sesamoid pair has two cruciate ligaments on the palmar aspect; the sesamoid on the palmar aspect of metacarpal I has only one.29 The dorsal sesamoid bones are attached by the tendons of the common digital extensor and interosseous muscles proximally and by a ligament to the dorsal surface of the second phalanx distally (Figures 56-1, 56-3, and 56-5).29,72 The interdigital ligaments hold the digits together and are the major supportive structures of the pad. They originate from the second and fifth tendons of the superficial digital flexor muscle proximal to the metacarpophalangeal joints. The interdigital ligaments insert at the proximal annular ligaments of the second through fifth digits, and after they conjoin, they cover the flexor tendons (see Figures 56-1, 56-3, and 56-5).29 Two anatomic differences have been noted between the dog and cat in the distal thoracic limb. First is the absence of a straight medial collateral ligament of the carpus in the cat. The medial collateral ligament of the canine carpus has both a straight and an oblique part, and the two parts are separated by the abductor pollicis longus muscle tendon.29 It is proposed that this anatomic difference accounts for feline palmar antebrachiocarpal luxation with only partial disruption of the medial collateral ligament.77,81 It is suggested that, because of this anatomic difference, antebrachiocarpal luxation in the cat is not nearly as devastating an injury as it is in the dog.77,81 The cat claw is retractable because of the dorsal elastic ligament and anatomic and structural differences in the middle and distal phalanx.37 The cat, similar to the dog, has two dorsal elastic ligaments. The larger dorsal elastic ligament extends from the lateral aspect of the head of the middle phalanx to the dorsal surface of the ungual crest. The smaller dorsal elastic ligament originates at the dorsal surface of the middle phalanx base and inserts on the medial surface of the ungual crest. The dog’s two dorsal elastic ligaments attach proximately to the dorsal surface of the middle phalanx base (similar to the cat’s smaller dorsal elastic ligament), and they insert close together on the dorsal aspect of the ungual crest (similar to the insertion of the large dorsal elastic ligament of the cat). The dog lacks a dorsal elastic ligament attachment to the head of the middle phalanx, and the shape of the head of the medial phalanx different from that of the cat, and it does not provide clearance for retraction.37 The cat uses the claws for holding prey (in comparison with the dog, which uses the jaws for holding prey), and this may be the functional reason for the anatomic differences of the claw.37 Kinematics of the Distal Thoracic Limb Several kinematic studies published in the veterinary literature can help to elucidate the function of the normal distal thoracic limb. The carpus has been studied during a walking and trotting gait in both heterogeneous and homogeneous breed populations.2,19,46 Additionally, the metacarpophalangeal joint has been evaluated at a walk in dissimilar breeds.66 In these studies, the methods used to calculate joint angles are varied. When dynamic joint motion is recorded in three dimensions (≥2 cameras), the joint angles can be calculated as vectors in true three-dimensional space or as projected motion onto a two-dimensional plane,66 most commonly, the sagittal plane (i.e., flexion and extension). Differences in marker placement have been shown to affect kinematics and may benefit from a normalization procedure.19 If a single camera is used to capture dynamic gait data, only two-dimensional data are obtained. The effect of using different calculation methods on resulting angles is unknown. Joint motion is often reported graphically as a waveform. This is commonly represented as joint angle versus (%) gait cycle. Furthermore, singular peak values have been reported. Static joint angles of the distal limb have also been reported during a standing load, as determined by forelimb radiography.82 These data show that the static carpus extension angle while standing is less than the dynamic joint angle at a walk or trot. What is unclear is whether the static standing angle or the maximum dynamic angle of the antebrachiocarpal or the carpometacarpal joint is a more important surgical consideration. This may prove clinically relevant when applied to pathologic conditions of these joints (osteoarthritis, joint laxity, ankylosis, and arthrodesis). Application of these data clinically can prove challenging because of sources of variability during data acquisition. Dog morphology, limb measurement techniques, gait speed (walk or trot), marker placement, skin movements, and the ability of the recording system to accurately identify the markers can affect data acquisition and data output. In the forelimb, these variances seem to be greatest in the antebrachiocarpal and metacarpophalangeal joints. The variance of the antebrachiocarpal joint angle has been shown to be 42.5 degrees between trials and 52.4 degrees between dogs compared with a mean variance of 12.6 degrees between trials and 6.2 degrees between dogs in proximal forelimb and hindlimb angles.2 To provide for ease of comparison between studies, joint angles will be described in this chapter as negative in flexion and positive in extension where 0 degrees is defined as when the bones about the joint form a straight line. The antebrachiocarpal joint at a walk has been reported to be approximately 18 degrees throughout most of the stance phase.46 At the end of the stance phase, rapid flexion occurs and is followed by rapid extension during the swing phase. Another study found that the antebrachiocarpal joint angle ranged from −12.4 degrees at the start of the stance phase to a peak of 26 degrees at 75% stance.66 The metacarpophalangeal joint angle at the walk changed little during stance phase. At the initiation of the stance phase, the metacarpophalangeal joint angle was 47.3 ± 27 degrees. This angle changed <5 degrees by 50% stance. However, a steady increase to 35.2 ± 40 degrees was noted at the termination of stance phase and the initiation of swing phase. Recent kinematic work was done at the University of California, Davis Gait Lab. Video and force plate data were collected from 7 dogs at a trot (velocity, 1.86 m/sec ± 0.13) for four trials each. The mean peak ground reaction force on forelimbs was 108% body weight. The joint angles were calculated by translating three-dimensional (3D) angles into a two-dimensional sagittal plane. The peak antebrachiocarpal joint angle was 47.3 ± 6.0 degrees and occurred at 50.9% of stance. Upon initiation and termination of the stance phase, the joint angle was 10 ± 12 degrees. The peak metacarpophalangeal joint angle was 19.2 ± 6.1 degrees and occurred at 62.6% of stance. Upon initiation and termination of the stance phase, the metacarpophalangeal joint angle was approximately −3 ± 11 degrees) (Figure 56-6).* In a study conducted to evaluate restricted carpal range of motion, joint kinematics was evaluated bilaterally while the carpus was unilaterally restricted with tape. Following restriction, a significant decrease in flexion of the carpus was noted during the swing phase. Minimal changes to the extension of the restricted carpus occurred in stance, yet the method of restriction was not equivalent to a joint arthrodesis or splint. Significant change was noted in the ipsilateral shoulder joint and the contralateral stifle joint.30 The bones and joints of the distal thoracic limb play intricate roles in distal limb injury. Clinically, it is recognized that many of the injuries of the manus result from hyperextension of the affected joint. Hyperextension occurs as the result of excessive loading of the limb, whether this is associated with a fall, with running, or with a twisting motion at the limb. Fractures are often intra-articular and involve concurrent ligament injuries and subluxations/luxations. Because of this, many simple carpal bone fractures fit the classical criteria for internal fixation.53 The mechanical properties of six canine carpal ligaments have been evaluated in an effort to model the distal thoracic limb for a finite element model. Ligaments studied included the accessorometacarpal IV, accessorometacarpal V, palmar radiocarpal, palmar ulnocarpal, and medial and lateral collateral ligaments of the carpus. Results indicate that the accessorometacarpal ligaments had the highest elastic modulus, which may be associated with their function to prevent hyperextension. Palmar radiocarpal and palmar ulnocarpal ligaments had a higher elastic modulus the medial collateral and lateral collateral ligaments; the palmar radiocarpal and palmar ulnocarpal ligaments are intra-articular and restrict cranial and caudal instability. The medial and lateral collateral ligaments support the joint in valgus and varus deviation, respectively, and had the lowest elastic modulus of the ligaments examined. The mode of failure of all six carpal ligaments tested showed that 58.3% failed at mid-ligament, 22.9% had an avulsion fracture, and 18.8% failed at the bone-ligament interface. Although this study highlighted the fact that the carpus has other supporting structures, such as palmar fibrocartilage and flexor retinaculum, along with limitations with testing in vitro, it was a first step for carpal function modeling.78 Carpal bone fractures can be difficult to diagnose on standard radiographic projections. Oblique, skyline, and stress radiographic views are indicated if the patient has clinical signs of injury to the carpus. Comminuted fractures of the carpal bones, articular fractures, and fractures associated with degloving wounds and infection are likely to result in osteoarthritis of varying severity. In instances of severe injury, this is likely to result in the development of severe osteoarthritis; arthrodesis of the carpus should be considered.53 A majority of radial carpal bone fractures, as reported in case series in the literature, occur in active dogs that have not sustained significant trauma.36,57,79 The three studies were similar in that some of the dogs had bilateral radial carpal bone fractures, a male predilection and a breed predilection (Boxer, English Springer Spaniel, Setters, and Pointers) were noted, and in most cases, a history of chronic lameness with waxing and waning signs was reported. The fracture configurations were mostly dorsal slab fractures, midbody sagittal (dorsoproximolateral to palmarodistomedial oblique) fractures, or comminuted T-shaped fractures. It is proposed that these fractures may result from incomplete fusion of the three centers of ossification of the radial carpal bone.36,53,57,79 The traumatic type of radial carpal bone fracture occurs in the right radial carpal bone of racing Greyhounds. These are often oblique midbody fractures and can be incomplete and difficult to diagnose.53 Chip fractures or avulsion fractures at the attachment of the palmar carpometacarpal ligament or the attachment of the oblique part of the short radial collateral ligament on the palmar prominence of the radial carpal bone are also reported.20 Physical examination findings include variable degrees of lameness, with soft tissue swelling (acute) or chronic joint thickening around the carpus. Manipulation of the carpus may elicit a pain response and may reveal a decreased range of motion caused by chronic degenerative joint changes. If standard radiographic projections for radial carpal bone fractures are inconclusive, a computed tomography (CT) scan is indicated.36 Clinical outcome is most likely related to restoration of radial carpal bone joint surfaces and the severity of secondary degenerative change. Osteoarthritis is an expected outcome even after anatomic repair of a joint surface.11,31,38 Methods of surgical repair include lag screw fixation or Kirschner wire fixation if the fragment is large, but small fragments are often excised.48,72 If implants are used to stabilize the fragments, it is important that they do not interfere with the articular surface. A dorsal surgical approach70 is best for repairing small dorsal slab fractures, and if combined with opening the tendon sheath of the extensor carpi radialis muscle proximally, the approach is good for large dorsal slab fractures. The palmaromedial approach allows exposure to repair midbody radial carpal bone fractures.70 A combination of the palmaromedial approach and the dorsal approach increases exposure, facilitates fracture reduction, and allows better orientation for placing the lag screw to repair midbody fractures. The lag screw should be placed from the palmaromedial aspect of the radial carpal bone obliquely in the dorsolateral direction.53 Radial carpal bone fractures that are incomplete or nondisplaced are sometimes treated with external coaptation splints or casts. Review of multiple case series studies reveals that many dogs have various degree of lameness after conservative treatment. However, the result of this treatment is difficult to interpret from these studies because many of the dogs included in these reports had no history of significant trauma, the fractures were somewhat chronic, and all dogs had varying degrees of osteoarthritis, making it impossible to speculate about the true outcome with conservative management.36,57,72,79 The methods of repair presently used for radial carpal bone fractures are not rigid enough to allow full weight bearing immediately after surgical repair. Because it is impossible to restrict the dog enough to limit these weight-bearing forces early on in the fracture healing process, it is generally accepted to add a coaptation device, typically a splint or cast, for 6 to 8 weeks following surgery, and to severely limit patient activity. Bone healing will vary within individual patients; therefore, the clinician has to assess both physical examination and radiographic findings over time to determine the optimal time to remove the external coaptation and to initiate range of motion and weight-bearing exercises.52,72 Rarely would the coaptation be needed longer than 8 weeks if it was used as an ancillary device to the fracture repair. Studies of accessory carpal bone fractures have all focused on the racing Greyhound. These fractures usually occur in the right carpus (80%) in dogs that race on elliptical tracks in a counterclockwise direction.50,51,72 The proposed mechanism of injury is full weight bearing on the right carpus at the racetrack turn when the accessory carpal bone is acting as a fulcrum for the palmar carpal ligaments and the flexor tendons to prevent hyperextension of the carpus.52 Accessory carpal bone fractures were classified into five types in an effort to study the incidence, best treatment methods, and prognosis of these fractures (Figure 56-7).51 Type I fracture, avulsion fracture of the distal margin of the articular surface at the attachment of the ligament from the accessory carpal bone to the ulnar carpal bone, accounted for 67% of accessory carpal bone fractures in a study of 50 racing Greyhounds.50 Type I fractures are further classified into type Ia, palmarolateral, and type Ib, palmaromedial.53 Types I, II, and III are considered sprain avulsion fractures, but only types I and II are intra-articular. Type II (13%) fractures occur at the proximal margin of the articular surface of the accessory carpal bone at the origin of the ligaments that connect the accessory carpal bone to the distal radius and ulna. Type III fracture (3%) is classified as an avulsion at the distal surface at the caudal end of the accessory carpal bone. This is the origin of the two accessorometacarpal ligaments that insert on metacarpals IV and V. Type IV (12%) is an avulsion at the tendon insertion of the flexor carpi ulnaris muscle at the caudoproximal surface of the accessory carpal bone. Type V (5%) is described as a comminuted fracture of the accessory carpal bone.50,51,53 In a large clinical study, all type II and III fractures were viewed in combination with type I fractures. Although this fracture combination is likely to cause long-term disability, 91% of the 11 dogs followed in the study returned to racing after successful surgical repair.52 Patient selection was biased in the study toward valuable racing dogs and those with large fracture fragments, yet this study highlights that some dogs can go back to a racing career if patient selection and surgical approach and repair are handled well.52 The clinical history of accessory carpal bone fracture is known only in racing Greyhounds. Most fractures occur at the time of racing, but a few were reported during training. The typical history reported was that the injury occurred at a turn, and another dog may have bumped the injured dog. The injured dog finished the race, but in last place. Lameness, carpal swelling, and carpal pain progressively worsened over the following few days.50 The accessory carpal bone is best visualized on a lateral radiograph of the carpus in extension, yet the dorsopalmar view is always taken because other injuries could be present. Oblique or stress radiographs of the carpus may be indicated in some cases. A palmarolateral approach to the carpus is recommended for surgical repair.70 Repair of accessory carpal bone fracture may occur as fragment removal or internal fixation, usually with a 1.5 or 2.0 mm lag or positional screw. It is important to preserve the paired accessorometacarpal ligaments and the accessoroulnar carpal ligaments during the repair. For type I and type II accessory carpal bone fractures, it is advisable to examine the articular surface through an arthrotomy to inspect the number of fragments and the condition of the joint surface. Type V accessory carpal bone fractures are considered nonsurgical because of the small fragments and inability to reconstruct the articular surface.52,53 External coaptation is used postoperatively, and radiographic fracture healing is reported to occur by 5 to 8 weeks after surgery. Osteoarthritis of the accessoroulnar carpal joint was a factor that contributed to poor outcome.52 Data is insufficient to predict long-term outcome after accessory carpal bone repair. To date, no data have been reported on the incidence, treatment, or outcome after fracture of any of the ulnar or numbered carpal bones. Accurate diagnosis can be difficult because of small fragmentation of the bones. Dogs reportedly have lameness, swelling, and pain at the carpus. Standard orthogonal and oblique views are recommended for radiographic evaluation. CT used to locate the site of small fragments or fractures may prove to be the best diagnostic tool. Treatment recommendations include fragment removal and external coaptation.72 Metacarpal and Metatarsal Fractures Few studies on metacarpal or metatarsal fracture have been conducted in the dog and the cat, and the largest studies are retrospective.54,60,65 Published guidelines for treating metacarpal or metatarsal fractures originate from early human literature on metatarsal fracture. Those surgical guidelines have been modified so that surgical correction is recommended in the dog and cat (1) if more than two metacarpal or metatarsal fractures are present in the same manus, (2) if the fractures involve both of the primary weight-bearing bones (metacarpals or metatarsals III and IV), (3) if the fractures are articular fractures, (4) if the fracture fragments are displaced by >50%, (5) if the fracture involves the base of metacarpal/metatarsal II or V, and (6) if the dog is a large-breed or athletic working or show dog.83 No evidence indicates that these guidelines are true if it is assumed that the outcome measurement is fracture healing without lameness. Three retrospective studies used clinical patients for which the owner chose the treatment after clinician consultation. One study included 37 dogs,65 one had 43 dogs,60 and one had 25 dogs54; no study had strict inclusion criteria or subgroups that depended on clinical conditions. All used owner nonvalidated subjective questionnaires and radiographic analysis and veterinary clinical assessment when available. Although surgical fixation with bone plates may have improved alignment of the fractures radiographically,65 no study could show that any single treatment was better than another. All treatments (conservative or surgical) had a high complication rate. One study60 showed that fractures with a high degree of fragment displacement and articular fractures had higher complication rates than others. Because of the level of evidence of these studies, the clinician must rely on his or her intuition as to whether or not the patient would benefit from any one treatment over another. A confounding factor in all published studies is that all methods of internal fixation for metacarpal or metatarsal fractures use implants that are not rigid. Therefore, patients have external coaptation regardless of the method used, making it difficult to weigh the benefits of internal fixation with external coaptation against external coaptation alone.54 Metacarpal and metatarsal fractures in the pet (nonracing Greyhound) population usually occur as the result of trauma. In one canine study, metacarpal fractures were more common than metatarsal fractures, and 41% of the metatarsal fracture group had four bones fractured. This study also found that most fractures occurred in the middle or distal region of the bones.65 Clinically, dogs and cats present with various degrees of lameness and swelling over the area. The clinician should look for wounds over the area because soft tissue coverage is minimal over the bones.22,72 In racing Greyhounds, metacarpal fractures are considered stress or fatigue fractures.7 They occur most commonly in young racing Greyhounds on metacarpal V of the left thoracic limb or metacarpal II of the right thoracic limb. Most likely, this distribution has to do with how the metacarpal bones are loaded around the racetrack turns.3 These fractures are classified by Dee and Dee into three types, depending on the degree of lameness and cortical bone disruption. Type 1 injuries have endosteal and cortical bone thickening on radiographs, and patients are clinically lame on the day of the race and the day after the race. Treatment for type I injuries consists of rest for 3 months with a slow return to activity. Type 2 injures are described as minimally displaced hairline fractures. External coaptation for 6 to 8 weeks is usually described for type 2 fractures. Type 3 fractures are described as complete fractures with fracture displacement. Clinically, the dogs are lame, and surgical fixation with external coaptation is recommended for an optimal chance of return to racing. In general, the prognosis in racing Greyhounds for type 1 and 2 metacarpal fractures is good, and for type 3 injuries is guarded.3 The successful outcome measurement for racing Greyhounds is when they return to racing and successfully win races. Recommendations for the racing Greyhound cannot necessarily be extrapolated to the pet population. Most surgeons who work on racing Greyhounds recommend internal stabilization with external coaptation for optimal outcome. The one study that published case outcomes in racing Greyhounds had 16 of 23 dogs returning to training; 6 retired because of poor performance, 2 had additional fractures, and 4 raced in fewer than 10 races each.7 Only 4 dogs returned to race in more than 10 races with some success. This study grouped all the different types of fractures and treatments together; 3 dogs were treated with screw fixation and 1 was treated with a cast.7 Classical conservative treatment of metacarpal or metatarsal fractures involves casting materials or modified Robert Jones–type bandages with a splint material applied to the palmar/plantar aspect of the lower limb. Bandaging and splinting is discussed in Chapter 45. As with all fractures that are managed using this modality, the clinician should strive to improve the alignment and apposition of fractures before placement of the coaptation.22,72 The medial surgical approach is typically used for a metacarpal II fracture, as is a lateral surgical approach for a metacarpal V fracture repair. Otherwise, a dorsal approach directly over the metacarpal or between two metacarpals is recommended. The extensor tendons can be retracted to either side to gain access to individual bones. A tourniquet (see Chapter 19) can be used to minimize hemorrhage during surgery.22 The size of the fragment may dictate the technique chosen for all surgical repairs of metacarpal/metatarsal fractures. If the fragment is too small for repair, and the fracture does not heal or heals with pain associated with callus or osteoarthritis, the entire digit can be amputated if only one metacarpal is affected.22 Methods described for metacarpal or metatarsal diaphyseal fractures include intramedullary Kirschner wires placed in normograde fashion, starting on the dorsal surface proximally or distally to avoid the joints. Following placement, the pins typically are bent at the insertion site and cut short.22,49,72 “Dowel” pinning techniques are described wherein the Kirschner wire is placed retrograde into the longer fragment and is cut to the approximate length of the other bone fragment; then the distal fragment is distracted sufficiently to allow insertion of the cut Kirschner wire into the distracted fragment.8,23,89 Small bone plates can be used on the dorsal surface of metacarpal/metatarsal bones. Because of the small size of the bone, 1.5 or 2.0 mm screws are used to secure the plate of corresponding size. It is unclear whether the plates interfere with the extensor tendons. Some surgeons prefer to plate metacarpal/metatarsal II medially and metacarpal/metatarsal V laterally to avoid this possible complication.22 External skeletal fixation with small pins and epoxy putty bars or via connecting bars with traction is described in the literature. Clinical outcome with external skeletal fixation for metacarpal fracture is similar to that described with other techniques described for metacarpal fractures (Figure 56-8).18,75
Carpus, Metacarpus, and Digits
Anatomy
Carpal Joints and Ligaments
Metacarpal Bones and Joints and Sesamoid Bones
Phalanges, Phalangeal Joints, and Associated Ligaments
Specific Anatomic Differences in the Cat
Function
Mechanisms of Antebrachiocarpal and Metacarpophalangeal Injuries
Carpal Fractures
Radial Carpal Bone Fractures
Accessory Carpal Bone Fractures
Ulnar Carpal and Numbered Carpal Bone Fractures
Fractures—Distal Limb
< div class='tao-gold-member'>
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Carpus, Metacarpus, and Digits
Only gold members can continue reading. Log In or Register to continue