Blood-Modifying, Antineoplastic, and Immunosuppressant Drugs
Learning Objectives
After studying this chapter, you should be able to
1. Explain the role of erythropoietin in red blood cell formation.
2. Describe the significance of iron in the hemoglobin molecule.
3. Give an example of iron deficiency anemia that occurs in veterinary medicine.
4. List the potential indications for and limitations of hematinics and oxygen-carrying solutions.
5. Describe the clotting mechanism in general terms.
6. List four anticoagulants and discuss their methods of action.
7. List examples of topical hemostatics.
8. Name the antagonist for heparin overdose.
10. Define fibrinolysis and name a fibrinolytic agent.
11. Describe the phases of the cell cycle.
12. List six categories of antineoplastic drugs and give an example of each.
13. Define biologic response modifier (BRM) and list two examples of BRMs.
14. List indications for the use of immunosuppressive drugs and provide five examples.
15. Discuss the safety precautions involved in the use of antineoplastic drugs.
Key Terms
Alkylation
Cell cycle–nonspecific
Cell cycle–specific
Cytotoxic
Disseminated intravascular coagulation (DIC)
Endothelial layer
Erythropoietin
Fibrinolysis
Hybridoma
Metastasis
Myeloma
Myelosuppression
Thrombocytopenia
Thromboembolism
Thrombus
Vesicant
Introduction
In the first section of this chapter, drugs or agents that influence blood formation or its processes (e.g., clotting and fibrinolysis) such as hematinics, anticoagulants, anticoagulant antagonists/hemostatics, and fibrinolytic agents are discussed. Because anticoagulants are used routinely in veterinary practice, veterinary technicians should have a complete working knowledge of their applications and their potential misuse.
The second section covers antineoplastic and immunosuppressant drugs. Antineoplastic drug categories include alkylating agents, antimetabolites, mitotic inhibitors (vinca alkaloids), antibiotics, hormones, and miscellaneous agents. Safe handling techniques for these potentially dangerous agents are listed. Select immunosuppressant drugs and their clinical applications are discussed at the conclusion of this section.
Blood-Modifying Drugs/Agents
 Hematinics
Hematinics
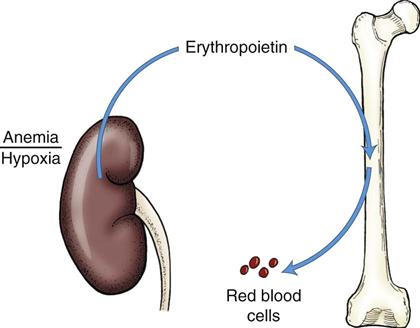
Red blood cells are formed in the bone marrow in response to stimulation by erythropoietin, a chemical released by the kidneys when hypoxia is present in this organ (Ganong, 2003) (Figure 16-1). Their primary function is to carry oxygen to the tissues. This activity is greatly enhanced by the hemoglobin component of red blood cells. Only a small portion of oxygen is carried in solution in the plasma.
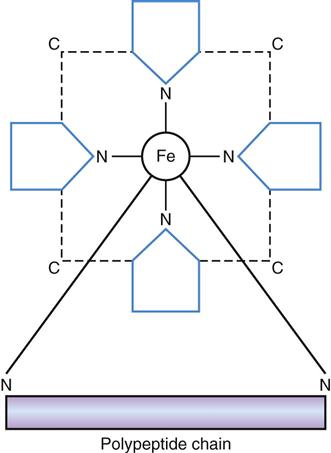
Hemoglobin is made up of a protein and an iron-containing pigment (Figure 16-2). The iron in hemoglobin must be in the ferrous (Fe2+) state to combine with oxygen in the most efficient way. If the iron in hemoglobin is in the ferric (Fe3+) state, hemoglobin cannot combine with oxygen and is called methemoglobin. Adequate amounts of iron, cobalt, copper, B vitamins, trace minerals, and protein are needed for normal hemoglobin and red blood cell formation.
Anemia can result from excessive loss of red blood cells, formation of inadequate numbers of red blood cells, or inadequate amounts of hemoglobin in the red blood cells. Iron deficiency anemia, a relatively common form in humans, is rare in animals that consume balanced diets. One exception, however, is baby pig anemia, a condition that results from inadequate assimilation of iron from the placenta of the sow for future hemoglobin formation by the piglet. The piglet is born without adequate stores of iron for its rapid growth phase, and sow’s milk is relatively low in this element. Baby pig anemia is a problem of pigs raised in confined environments (concrete or slatted floors) because those raised outdoors usually obtain adequate iron from the soil.
Hematinics are substances that tend to promote an increase in the oxygen-carrying capacity of the blood. Hematinics are used to prevent or treat anemia, and the primary ingredient in most of these products is iron, a vital component of hemoglobin. Some also contain copper and B vitamins to enhance red blood cell formation. The response to hematinic administration is relatively slow, and this factor makes use of hematinics ancillary to whole blood transfusion in acute anemia.
Iron Compounds
Many injectable and oral iron preparations are available for veterinary use under generic and proprietary labels. The form of iron in these products may be iron dextran, ferrous sulfate, peptonized iron, gleptoferron, ferric hydroxide, and others, and the form apparently has little effect on use. Copper, B vitamins, liver fraction (an iron source), and palatability enhancers often are also added to the oral products. Injectable forms are labeled for intramuscular injection and contain only iron. They may cause discoloration of muscle tissue at the site of injection.
Clinical Uses
Iron compounds are used for prevention or treatment of baby pig anemia or as a nutritional aid, depending on the form.
Dosage Forms
Adverse Side Effects
These are rare but may include muscle weakness, prostration, or muscle discoloration.
Erythropoietin
Erythropoietin, a protein produced in the kidneys, stimulates the division and differentiation of committed erythroid precursors in the bone marrow. A synthetic product, Epogen, has the same properties as erythropoietin and is available commercially. It is approved for human use and is produced by recombinant DNA technology. It is labeled for the treatment of anemia related to chronic renal failure or for that associated with azidothymidine treatment in patients with human immunodeficiency virus infection. No veterinary-approved product is available.
Clinical Uses
Erythropoietin is used in dogs and cats for the treatment of anemia associated with chronic renal failure or other causes.
Dosage Forms
Adverse Side Effects
In humans, adverse side effects may include hypertension, iron deficiency, polycythemia, and seizures. The use of human-coded proteins in dogs or cats could potentially cause allergic reactions.
Androgens
The treatment for anemia associated with chronic renal failure has traditionally been androgen therapy. Results obtained with the use of androgens for chronic anemia have been inconsistent.
Clinical Uses
Androgens are used for the treatment of chronic (nonregenerative) anemia.
Dosage Forms
Adverse Side Effects
These have included enlargement of the prostate, hepatic toxicity, and sodium and water retention.
Blood Substitutes
Researchers have looked for an oxygen-carrying substitute for red blood cells practically since it was learned that the hemoglobin in those cells was the transporting vehicle.
Oxyglobin is a red blood cell substitute that consists of a polymerized bovine product with a hemoglobin concentration of 13 g/dL in a modified lactated Ringer’s solution. This solution has obvious benefits over blood products that include availability, a long shelf life, universal compatibility, and freedom from disease-producing agents.
This hemoglobin solution picks up and distributes oxygen in a manner similar to red blood cells, but the oxygen-carrying function is shifted to cross-linked hemoglobin molecules in the plasma. Because oxygen is carried by molecules in the plasma, diffusion of this gas across cell membranes occurs more efficiently than when it is carried by red blood cells because one fewer membrane must be crossed.
This product is stable for 3 years when unwrapped at room temperature or in the refrigerator but it should not be frozen. Once the wrapper has been removed, the product must be used within 24 hours. It is compatible with any other IV fluid, but other solutions should not be mixed in the same bag. A separate line should be used for these other solutions. No consideration is needed regarding blood typing or crossmatching when this product is used.
Oxyglobin also has osmotic properties similar to dextran 70 and hetastarch.
Clinical Uses
This product is labeled for the treatment of anemia in dogs regardless of the cause. It has been used in cats and foals but is not labeled for such use.
Dosage Form
Adverse Side Effects
Potential side effects include pulmonary edema, discolored urine, discolored membranes, ventricular arrhythmias, fever, and coagulopathy. Oxyglobin can cause volume overload or vasoconstriction and should not be used in patients with cardiac or renal disease.
 Anticoagulants
Anticoagulants
Blood coagulation is an obviously essential process that is designed to inhibit the loss of vital blood constituents from the circulatory system. Two separate systems or pathways may initiate the clotting mechanism—the intrinsic (intravascular) and extrinsic (extravascular) systems.
The intrinsic pathway is activated by injury to the endothelial layer of a blood vessel, which disrupts blood flow and causes a chain of chemical reactions leading to a thrombus, or clot. This process helps to repair damage to blood vessel walls that occurs from routine wear and from pathologic processes.
The extrinsic pathway is activated by injury to tissue and vessels, which release tissue thromboplastin. Thromboplastin stimulates the clotting mechanism. Vasoconstriction occurs in damaged blood vessels, causing a slowing of blood flow and facilitating clot formation. Platelet aggregation and adherence are also important steps in the clotting process.
The intrinsic and extrinsic pathways converge into a common pathway in the final steps of clot formation (Figure 16-3). At least 13 clotting factors participate in this series of reactions (called a cascade) in which the product of the preceding reaction promotes the next reaction (Table 16-1). The final step in the process is the conversion of fibrinogen to fibrin by thrombin. If any of the clotting factors in the cascade are deficient or missing, clotting does not occur.
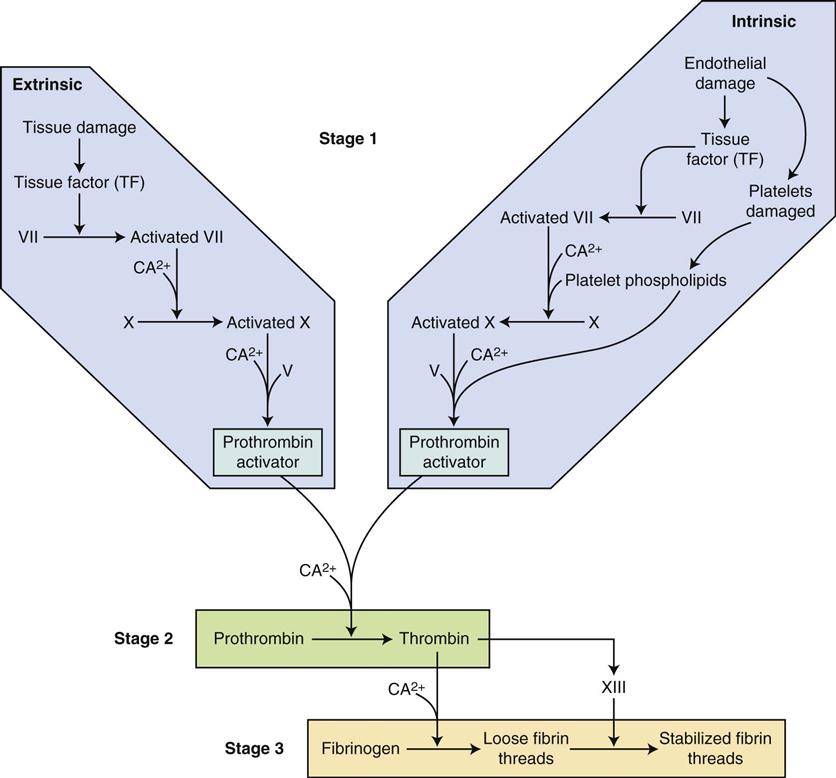
TABLE 16-1
| COAGULATION FACTOR | SYNONYM |
| I | Fibrinogen |
| II | Prothrombin |
| III | Tissue factor (thromboplastin) |
| IV | Calcium ions |
| V | Proaccelerin, labile factor, or accelerator globulin |
| VI | Activated factor V |
| VII | Serum prothrombin conversion accelerator (SPCA), stable factor, or proconvertin |
| VIII | Antihemophilic factor (AHF), antihemophilic factor A, or antihemophilic globulin factor B |
| IX | Christmas factor, plasma thromboplastin component (PTC), or antihemophilic factor B |
| X | Stuart-Prower factor, thrombokinase |
| XI | Plasma thromboplastin antecedent (PTA) or antihemophilic factor C |
| XII | Hageman factor, glass factor, or contact factor |
| XIII | Fibrin-stabilizing factor (FSF) or fibrinase |
A balance must be maintained in the body between clot formation and clot breakdown. Destruction of clots—fibrinolysis—occurs through the action of an enzyme called plasmin. Plasmin digests fibrin threads and other clotting products to cause clot lysis and the release of fibrin degradation products into the circulation.
Anticoagulants inhibit clot formation by tying up or inactivating one of the clotting factors to interrupt the cascade reaction. They are used clinically to prevent coagulation of blood (or other body fluid) samples that are collected for testing, to preserve blood for transfusions, to inhibit clotting in intravenous catheters, and to prevent or treat thromboembolic disorders (e.g., thromboembolic cardiomyopathy in cats).
Heparin may be used paradoxically to treat the bleeding disorder disseminated intravascular coagulation (DIC).
Heparin
Heparin is an anticoagulant that is found in many tissues of the body and is thought to be stored in mast cells. It is obtained from pig intestinal mucosa, and its strength is expressed in terms of heparin units. Heparin acts as an anticoagulant by preventing the conversion of prothrombin (factor II) to thrombin. Without thrombin, fibrinogen is not converted to fibrin and a clot does not form. Heparin does not break down clots but can prevent clots from increasing in size. It is administered therapeutically by intravenous or subcutaneous injection.
Clinical Uses
Heparin has various uses in veterinary medicine. It is used in vitro as an anticoagulant to preserve blood samples for testing by heparinizing (drawing heparin into the syringe and then forcing all visible quantities out) a syringe before the blood sample is drawn. It also is diluted in saline or sterile water for injection to form a flush solution for preventing clots in intravenous catheters. Heparin is sometimes used to preserve donated blood for transfusions when small quantities are needed (e.g., for cats or small dogs). It is used in vivo to aid in the treatment of DIC and thromboembolism and has been advocated for the treatment of laminitis in horses.
Dosage Forms
Forms approved for use in humans are used in veterinary medicine:
Adverse Side Effects
These usually manifest as bleeding or thrombocytopenia.
Ethylenediaminetetraacetic Acid
Ethylenediaminetetraacetic acid (EDTA) is an anticoagulant that prevents clotting by chelation of calcium (factor IV). With calcium ions tied up by EDTA, clotting cannot occur. It is used in vitro to preserve blood samples and is the anticoagulant of choice when a differential count is needed (it preserves white cell morphology well). EDTA is prepared in lavender-topped collection tubes.
The calcium salt of EDTA (calcium disodium versenate) is also used in vivo as a chelating agent to treat lead poisoning. This function does not involve the clotting mechanism (see Chapter 18).
Coumarin Derivatives
Coumarin derivatives such as dicumarol and warfarin are oral anticoagulants that bind vitamin K, therefore inhibiting the synthesis of prothrombin (factor II) and factors VII, IX, and X. These compounds are indicated for long-term treatment of thromboembolic conditions. They are used clinically to a greater extent in human medicine than in veterinary medicine.
Dicumarol may be found in moldy sweet clover and has been associated with fatal hemorrhagic disease in cattle. Warfarin and related compounds are used in many rat poisoning products.
Clinical Uses
Coumarin derivatives are used for the long-term management of thromboembolic conditions.
Dosage Form
Adverse Side Effects
Adverse side effects are related to hemorrhages.
Acid Citrate Dextrose Solution and Citrate Phosphate Dextrose Adenine
Acid citrate dextrose (ACD) solution contains dextrose, sodium citrate, and citric acid and prevents clotting by chelating calcium. It is prepared in bottles or plastic bags for blood collection under both veterinary and human labels. Bottles are available for collecting 250 and 500 mL of blood. ACD solution preserves blood for 3 to 4 weeks.
Citrate phosphate dextrose adenine (CPDA-1) solution is available in plastic bags for collection of 450 mL of blood. CPDA-1 also prevents clotting by chelating calcium and preserves blood for as long as 6 weeks.
Eight milliliters of ACD or CPDA-1 can be drawn into a syringe to collect 50 mL of blood when small quantities are needed (Norsworthy, 1992).
Antiplatelet Drugs
Antiplatelet drugs such as aspirin appear to impair clotting through inhibition of platelet stickiness and clumping. This activity is thought to be mediated through inhibition of the proaggregatory prostaglandin called thromboxane (Pugh, 1991).
Aspirin has been used both to prevent thromboembolism associated with heartworm treatment in dogs and to treat cardiomyopathy in cats.
 Hemostatics/Anticoagulant Antagonists
Hemostatics/Anticoagulant Antagonists
Substances that promote blood clotting—hemostatics—may be divided into two categories: (1) those applied topically and (2) those given parenterally.
Topical Agents
Topical agents act by providing a framework in which a clot may form or by coagulating blood protein to initiate clot formation. Framework substances used in topical hemostatics include gelatins and collagens, whereas styptics, hemostatic powders, and solutions are substances that initiate clotting through coagulation. The framework substances are absorbed after clot formation. Topical hemostatics are used to control capillary bleeding or bleeding from other small vessels.
Clinical Uses
These include the control of capillary bleeding at surgical sites or in superficial wounds.
Dosage Forms
Adverse Side Effects
These are usually minimal but may include delayed wound healing.
Parenteral Agents
Parenterally administered hemostatic agents act as anticoagulant antagonists because they do not directly activate clotting. These substances promote the synthesis of clotting factors that have been depleted through poisoning or disease, or they tie up (inactivate) anticoagulants that have been overdosed. These drugs are not used to control surgical or traumatic bleeding.
Protamine Sulfate
Protamine sulfate is a protein that is produced from the sperm or testes of salmon or related species (Plumb, 2011). Protamine has a strongly basic pH, and heparin has a strongly acidic pH. Protamine combines with heparin to form inactive complexes (salt).
Clinical Uses
Protamine sulfate is used for the treatment of heparin overdose. Slow intravenous administration is recommended.
Dosage Form
Adverse Side Effects
Hypotension and bradycardia can occur if given too rapidly.
Vitamin K1 (Phytonadione)
Phytonadione is a synthetic substance that is identical to naturally occurring vitamin K1. Vitamin K is necessary for the production (in the liver) of active prothrombin (factor II), proconvertin factor (factor VII), plasma thromboplastin component (factor IX), and Stuart factor (factor X). It is used clinically for treating cases in which vitamin K has been tied up or destroyed and in bleeding disorders associated with poor formation of vitamin K–dependent clotting factors. Immediate coagulant effect should not be expected after administration of vitamin K because several hours may pass before synthesis of new clotting factors occurs.
Clinical Uses
In veterinary medicine, vitamin K1 is used for the treatment of rodenticide toxicity, for bleeding disorders related to faulty synthesis of vitamin K–dependent clotting factors, and for unknown anticoagulant toxicity.
Dosage Forms
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree