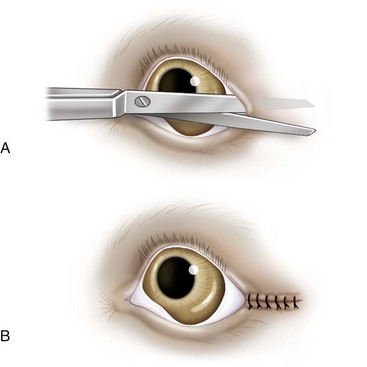
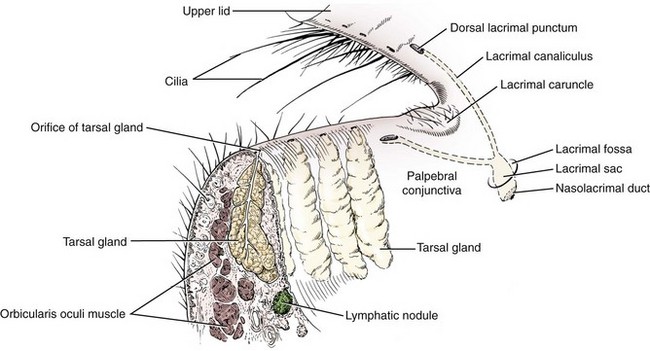
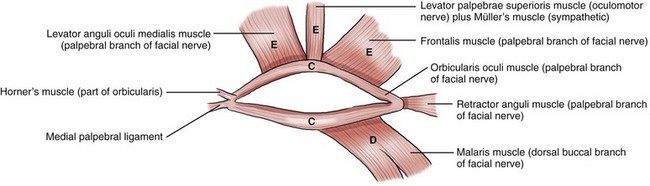
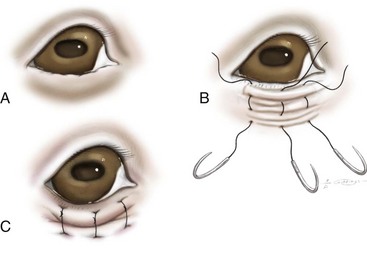
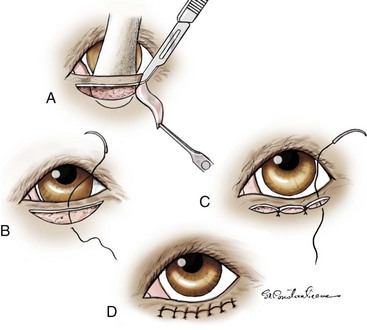
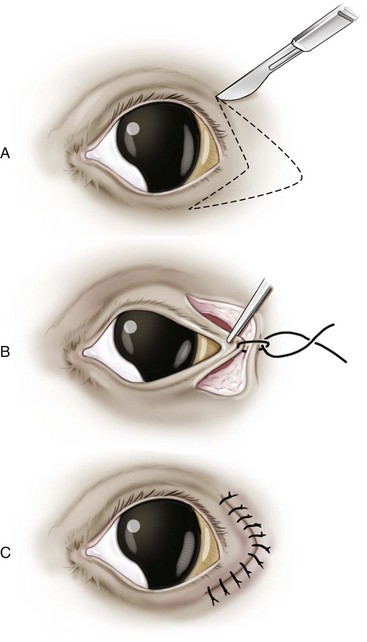
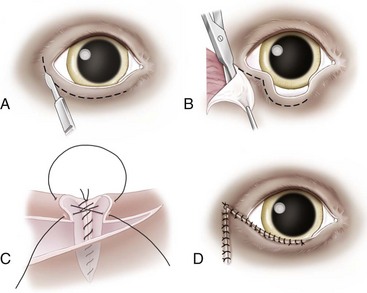
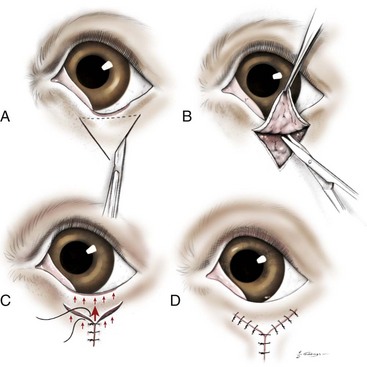
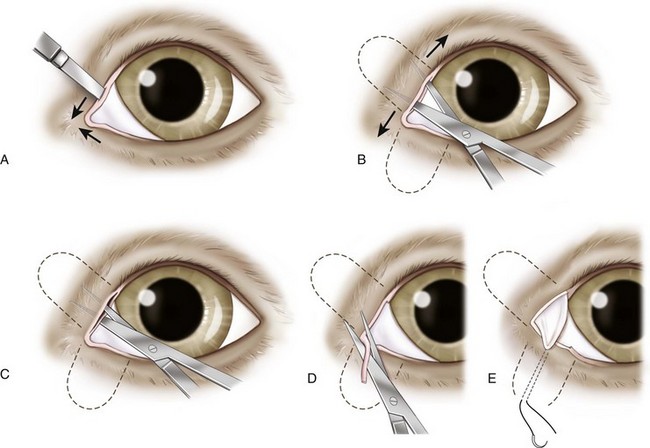
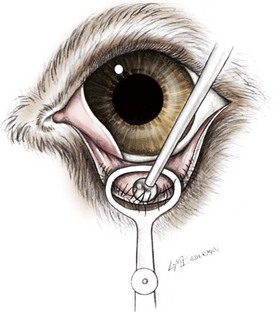
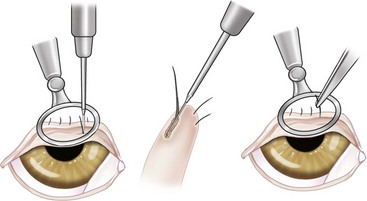
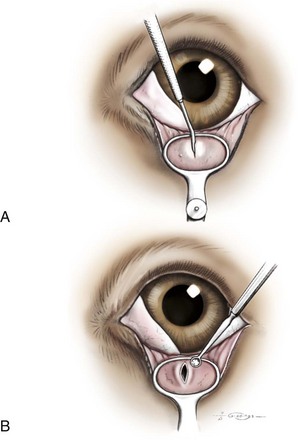
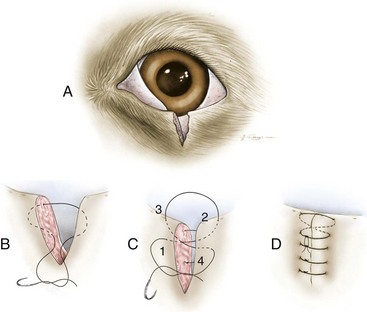
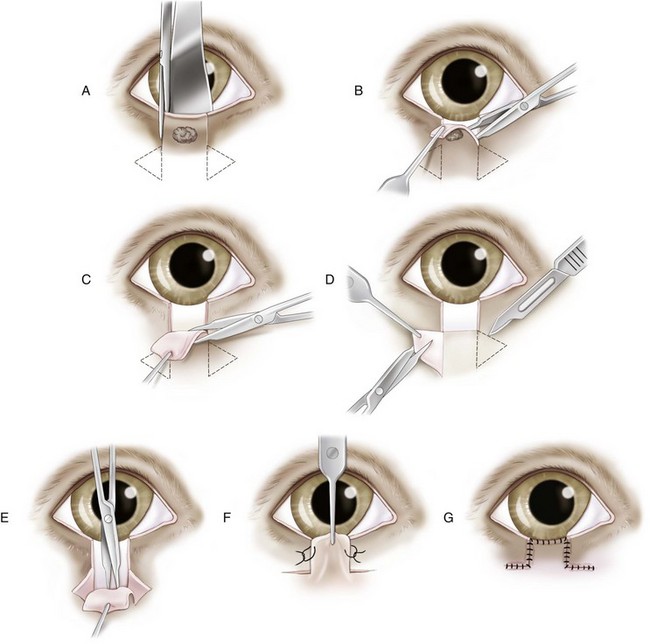
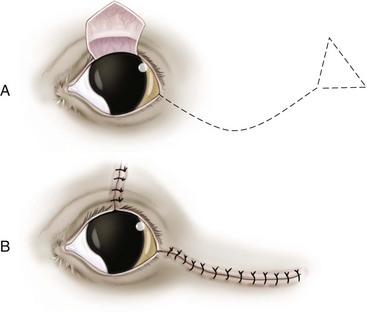
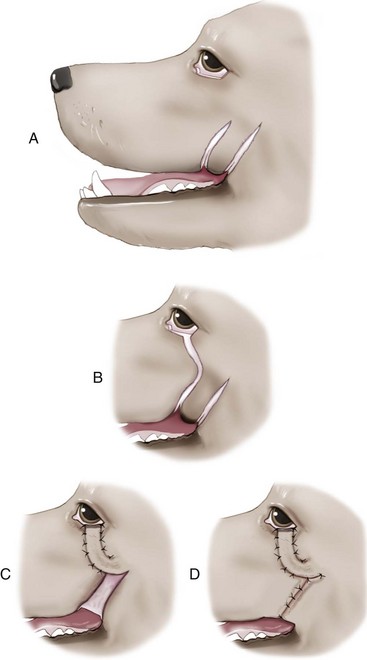
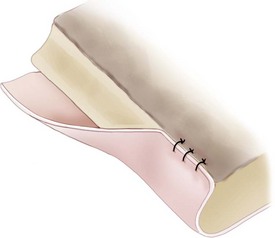
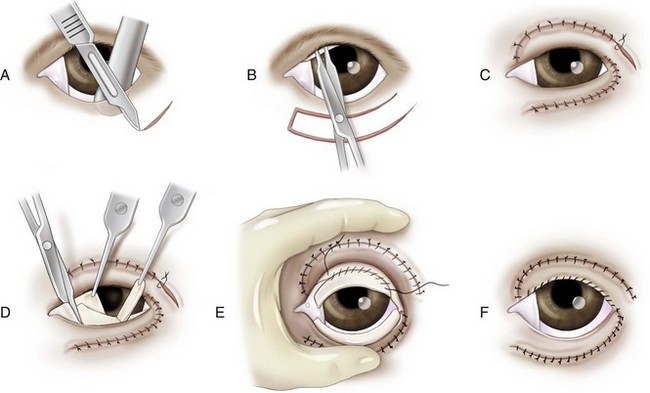
Chapter 124 The purpose of this chapter and Chapter 125 is to describe the most common adnexal and extraocular procedures done on dogs and cats. Although some clinical diseases are described, ophthalmic texts should be referenced if additional information is needed to become familiar with the disease processes. Intraocular procedures are not described here except for some information in the emergency procedure chapter (Chapter 125) because advanced training is required to master those techniques. General anesthesia is required for all but the most minor surgical procedures. Modern anesthetic protocols are acceptable for general anesthesia for patients undergoing ophthalmic procedures. Just as with all other patients requiring general anesthesia, a blood cell count, serum chemistry panel, and thorough general physical examination should be obtained. Thoracic radiographs, urinalysis, and other diagnostics may also be indicated. For most ophthalmic procedures, a quiet induction and smooth recovery are tremendously important to prevent ocular trauma. Paralysis with neuromuscular blocking agents such as atracurium can render optimal eye position for corneal and intraocular surgery, prevent increases in intraocular pressure from extraocular muscle contraction, and aid in prevention of the oculocardiac reflex.19 Ocular lubrication is a necessity during general anesthesia. When the cornea is exposed and artificial tear ointment cannot be used, an ophthalmic balanced salt solution should be dripped on the cornea every 5 to 10 seconds to maintain corneal moisture and prevent corneal desiccation and ulceration. Sedatives and analgesics should be on hand during the postoperative period in case there are signs of a rough recovery. Retrobulbar blockade is used by some; however, studies on its clinical effectiveness are rare. Two studies evaluated retrobulbar blocks for the purpose of negating the use of neuromuscular blocking agents in dogs undergoing phacoemulsification; both found the procedure to be safe and to provide good globe position.1,51 More frequently, blocks are used with enucleation to provide additional analgesia and slightly exteriorize the globe. Retrobulbar blocks are usually unnecessary and may result in complications such as retrobulbar hemorrhage, globe rupture, intravenous injection, and optic nerve injection and damage. Retrobulbar blocks should not be performed when local infection or neoplasia is present or when anesthetic monitoring is insufficient. Instruments used in ophthalmic surgery vary tremendously depending on the surgical procedure. Although some general surgical instruments are used with adnexal and orbital surgeries, additional finer instruments are also necessary. To perform many of the procedures described in this chapter, the surgeon should have one pack that includes a Barraquer eyelid speculum, Jaeger eyelid plate, fine-toothed Bishop-Harmon forceps, curved Steven’s tenotomy scissors, and small Derf needle holders (Figure 124-1). Additional instruments are mentioned in the text as needed. Lateral canthotomies that extend through the lateral canthus and terminate anterior to the lateral canthal ligament can be used to increase globe exposure (Figure 124-2). Hemorrhage is minimal if the incision is made while the eyelid speculum is in place. Alternatively, a small mosquito forceps can be used to gently crush the tissue before incision. The incision can be closed in a single (usual method) or double layer. If the deep tarsoconjunctival layer is closed, 5-0 or 6-0 simple interrupted absorbable sutures are placed, taking care to ensure that the suture does not contact the corneal surface. The eyelid skin and eyelid margin are closed in a simple interrupted pattern with nonabsorbable or absorbable 4-0 to 6-0 sutures. Occasionally, a figure of eight suture will be placed. Suture tags from the margin suture can be incorporated into the skin sutures. The typical arrangement of the muscles, cilia, and glands and location of the lacrimal puncta within the canine eyelid is depicted in Figure 124-3. In dogs, the tarsus, a fibrous tissue thickening surrounding the tarsal glands, is poorly developed or absent. The eyelids are therefore unstable and need to be in contact with the ocular surface to maintain conformation. The superior eyelid is elevated by the levator anguli oculi medialis, levator palpebrae superioris, Müllers, and frontalis muscles. The inferior eyelid is lowered by the malaris muscle. The superior and inferior eyelids are brought toward each other by the sphincter-like orbicularis oculi muscle. All eyelid muscles are innervated by the branches of the facial nerve except for the levator palpebrae superioris (oculomotor nerve) and Müllers (sympathetic) muscles (Figure 124-4). Sensation to the eyelids and corneal surface is provided by branches of the trigeminal nerve, which constitutes the afferent branch of the blink reflex.34,89 Medial and lateral canthal ligaments stabilize the eyelid commissures and prevent the palpebral fissure from becoming circular. The medial ligament is a distinct fibrous band originating from the frontal bone near the nasomaxillary suture. The medial ligament serves as the origin and insertion of the orbicularis oculi muscle. The lateral ligament is a poorly developed thickening of the orbital septum that originates from the zygomatic arch and ventral orbital ligament and terminates by blending into the fibers of the upper and lower tarsi. Function of the lateral palpebral ligament is supplemented by the retractor anguli lateralis muscle, which lies anterior to the ligament.34,89 Congenital absence of a portion of the eyelid margin is most common in cats and usually involves absence of a portion of the lateral superior eyelid. In dogs, the defect more commonly affects the lateral or central inferior eyelid. Small defects may be treated medically with topical petroleum-based lubricants. Defects that result in keratitis should be treated surgically. This condition can be associated with lacrimal gland agenesis, keratoconjunctivitis sicca, persistent pupillary membranes, cataract, retinal dysplasia, and optic nerve coloboma in cats.7 Defects smaller than one third of the eyelid margin may be treated by removing the edges of the defect; the edges of the resulting wedge defect are apposed with a simple two-layer closure (see section on simple two-layer closure below). Larger defects require more extensive reconstructive procedures and are typically repaired using the procedure first described by Roberts and Bistner108 and then modified by Dziezyc and Millichamp.27 Many other reconstructive techniques have been adapted to correct this defect;11,29,131 the technique used is therefore based on surgeon preference and the characteristics of the defect. Temporary Correction.: Temporary correction may be pursued in very young dogs if there is significant keratitis and skull development is not complete. Ideally, permanent correction should be postponed until skull conformation has reached adult size. In some breeds, such as Shar-Peis and Chow Chows, temporary correction is all that is needed because entropion resolves when facial maturity is attained. Temporary correction is achieved by placing vertical mattress sutures perpendicular to the eyelid margin in the area of the entropion. The first bite is placed 2 to 3 mm from the eyelid margin. The distance between the inner aspects of the first and second bites should correspond to the estimated amount of correction. Bites extend through the skin only and not through the conjunctiva because this would cause corneal irritation. The sutures are tied and knots positioned as far away from the eyelid margin as possible (Figure 124-5). A 3-0 to 5-0 nonabsorbable monofilament is typically recommended. Alternatively, polyglactin may be used. Inflammation associated with breakdown of absorbable suture may sometimes result in mild scarring that prevents entropion recurrence. An alternative to skin sutures that is quick, effective, and lasts longer is the use of skin staples. Staples are placed so a furrow forms within the staple, everting the eyelid. Permanent Correction.: Permanent correction is most commonly accomplished by removal of a crescent-shaped section of skin from the entropic region of the eyelid (Hotz-Celsus procedure). The eyelid is supported by a Jaeger eyelid plate or Desmarres entropion forceps. A skin incision parallel to and 2 mm from the eyelid margin, extending just beyond (2 to 3 mm) the rolled-in portion of the eyelid, is made with a #15 Bard-Parker or a 6400 Beaver blade. A second skin incision that arches away from the eye, beginning at one end of the first incision and ending at the other, is made. The distance between the first and second incisions, at its widest point, should correspond to the previously estimated correction amount. The crescent-shaped section of skin is sharply excised with tenotomy scissors; it is not necessary to remove any of the underlying orbicularis oculi muscle. If there is medial and lateral entropion but the central margin is normal, two crescents should be excised, one medially and one laterally. The defect is closed with simple interrupted 4-0 or 5-0 nylon or polyglactin sutures. The first suture should join the center of the first and second incisions. The second and third sutures should be placed so they bisect the remaining defects and so on until there are sutures every 3 to 4 mm. Sutures should be tightened only to the point where there is perfect apposition of skin margins (Figure 124-6). Suture tags should be cut short enough to ensure that they will not contact the cornea. In large-breed dogs that have concurrent upper and lower eyelid entropion laterally, an arrowhead-shaped section of skin is removed (Figure 124-7). Transection of the lateral canthal ligament improves the success of this procedure in breeds with large, broad skulls (e.g., Rottweilers, retrievers, and great Danes) in which the lateral canthal ligament causes inversion of the lateral canthus.109 Transection of the ligament is accomplished by grasping the lateral canthus and pulling it anteriorly and nasally so as to tighten the ligament. The ligament is localized by gently “strumming” across the conjunctival surface. An incision through the conjunctiva just over the ligament is made with tenotomy scissors. The ligament is relocalized by strumming and is then blindly transected with scissors. The conjunctival incision is not sutured. The eyelids, because of the poorly formed tarsus, are unable to maintain their conformation without resting on the corneal surface. When enophthalmos from orbital fat pad shrinkage (secondary to inflammation or cachexia) or an increase in orbital volume (e.g., chronic masticatory myositis) occurs, the eyelids tend to roll inward, resulting in involutional entropion. Correction of this type of entropion is difficult; the procedures outlined above are not ideal for its treatment because they do not address the position of the globe within the orbit. The eyelids will continue to roll in unless the corneal surface can be brought anteriorly to support the eyelids. Although poorly described in the veterinary literature, ideally, the enophthalmos should be corrected. Temporary success has been achieved in sighted humans with an intraconal injection of stabilized hyaluronic acid gel.70,124 There are many procedures designed to correct ectropion, and they are discussed extensively elsewhere.34,79,119 Wedge Resection.: The majority of cases of simple ectropion from an excessively long palpebral fissure can be corrected with a wedge resection or Munger and Carter modification of the Kuhnt-Szymanowski procedure.87 The wedge of tissue to be removed can be positioned anywhere along the eyelid margin. In cases with uniform eversion all along the eyelid margin, it may be wisest to excise the wedge close to the lateral canthus to diminish the consequences of notching that may occur if margin apposition is not perfect. In some breeds, such as mastiffs and Saint Bernards, there is a crease in the central portion of the eyelid; positioning the wedge to remove the creased portion of the eyelid can be advantageous. The length of eyelid margin that is removed should be slightly shorter than the amount of correction needed because fibrosis and wound contraction provide an additional 0.5 to 1.0 mm of correction (see section on wedge and pentagonal resection below). The wedge is closed using a simple two-layer closure (see section on simple-two layer closure below). Margin-Sparing Techniques.: The modified Kuhnt-Szymanowski procedure avoids splitting the eyelid as described in the original Kuhnt-Szymanowski procedure. An incision through the skin and orbicularis muscle, 3 mm from and parallel to the margin, starting at the lateral boundary of the medial third of the eyelid and ending 1 cm lateral to the lateral canthus is made. A second skin–orbicularis incision is continued ventrally from the lateral end of the first incision for approximately 1.5 cm. The skin and muscle flap is undermined with small tenotomy scissors. Two wedges with the same base width—one from the lateral extent of the skin muscle flap and one from the medial extent of the tarso-conjunctival flap—are removed. The wedges should be slightly smaller than the needed correction. The tarsoconjunctival margins are apposed with 4-0 or 5-0 simple interrupted absorbable sutures, taking care to not penetrate through conjunctiva, which could leave suture rubbing against the cornea. The eyelid margin is apposed with a figure of eight suture. The skin is apposed with simple interrupted sutures, with the first suture placed at the junction of the horizontal and vertical skin incisions and subsequent sutures bisecting the remaining incisions (Figure 124-8). The V–Y-plasty begins with two converging skin incisions on each side of the scarred tissue or ectropic margin. The V-shaped skin flap is elevated and underlying scar tissue resected, if present. The incisions are closed in the shape of a Y with simple interrupted 4-0 or 5-0 sutures. The length of the base of the Y should be about 2 to 3 mm longer than the amount of correction needed (Figure 124-9). Euryblepharon refers to a symmetric enlargement of the palpebral aperture secondary to longer than normal eyelids (macroblepharon). In brachycephalic breeds, this condition may be associated with medial canthal trichiasis and lagophthalmos, leading to chronic keratitis and progressive pigmentary infiltration (with or without corneal ulceration). Temporary relief can be achieved with topical lubricant ointments; however, definitive correction involves surgical reduction of the palpebral fissure. This is best accomplished by a permanent medial canthoplasty. Although several different procedures have been described, the pocket technique provides the greatest closure stability. In large-breed dogs such as Neapolitan mastiffs, bloodhounds, Newfoundlands, and Clumber spaniels, the exaggerated palpebral fissure and conformational enophthalmia may result in combined central ectropion with lateral entropion. A combination of a wedge resection to shorten the fissure and a Hotz-Celsus procedure to evert the entropic areas may be enough in some cases. However, when there is marked canthal instability, a procedure such as described by Bigelbach may be more appropriate.9 Pocket Technique for Permanent Medial Canthoplasty.: The lower lacrimal punctum is cannulated with 0-0 to 2-0 nonabsorbable monofilament suture. The upper and lower eyelids are split with a 6400 Beaver blade and small tenotomy scissors to a depth of about 10 mm, starting 2 to 3 mm medial to the upper and lower puncta. The eyelid margin is freshened by removing a small strip of eyelid margin in the area of the pocket. An incision in the conjunctiva, perpendicular to the eyelid margin, at the lateral aspect of the pocket in the upper eyelid is made to create a triangular flap; this sacrifices the upper lacrimal punctum. If there is extensive medial aberrant dermis or caruncular trichiasis, the offending tissue is sharply excised at this point. A horizontal mattress of 4-0 nonabsorbable suture is used to secure the tip of the conjunctival flap to skin at the bottom of the pocket of the lower eyelid. The new canthus is apposed with a figure of eight suture with 5-0 polyglactin, and the skin is closed in a simple interrupted pattern with the same material (Figure 124-10). If the lower nasolacrimal duct is inadvertently damaged during the procedure, the monofilament suture should be left within the duct and secured so that it remains in place for 3 to 4 weeks as the duct reepithelializes. The nonabsorbable mattress suture should be removed in 10 to 14 days. Placing a temporary tarsorrhaphy temporal to the surgical closure for 10 to 14 days helps to prevent stretching of the surgical site. Although many strictly surgical techniques have been described for permanent treatment of distichia,6,34 noninvasive techniques such as cryo- and electroepilation have the advantage of preserving the eyelid margin and usually do not result in scarring, which distorts and adversely affects eyelid function.127 All techniques aim to destroy the meibomian gland, thereby preventing hair regrowth. Destruction of a large percentage of the meibomian glands may result in qualitative tear deficiencies because of a lack of the lipid portion of the tear film. This can be treated medically by applying a topical petrolatum-based artificial tear ointment three or four times a day. Cryoepilation.: Because cryodestruction is best accomplished with a rapid freeze and slow thaw, a chalazion clamp is placed to decrease blood flow to the area. Cryoepilation is accomplished by placing a 4-mm cryoprobe over the base of the meibomian gland from the conjunctival side. When the ice ball reaches the eyelid margin, freezing should be stopped and the eyelid margin allowed to thaw. The process is repeated for a total of two freeze–thaw cycles (Figure 124-11). Nitrous oxide and liquid nitrogen probes are equally effective; because liquid nitrogen probes become much colder, however, excessive freezing is more likely with this medium. Immediately after treatment, there is usually severe eyelid and conjunctival swelling, which resolves in 48 to 72 hours. Marginal eyelid depigmentation is an expected sequela to freezing and usually resolves completely in 6 months.129 Overzealous freezing (tissue temperatures below −30° C) has been associated with eyelid scarring, necrosis, and permanent pigment loss. Thermocouples can be used to monitor and avoid excessively low tissue temperature; in practice, close observation of the ice ball and stopping freezing when it reaches the eyelid margin accomplishes the same objective. Electroepilation.: Electroepilation can be accomplished with a direct current electrocautery unit equipped with a fine cilia-epilating needle or specialized electroepilation unit. The goal is to thread the needle down into the meibomian gland and deliver enough energy to destroy the gland but not so much as to damage the rest of the eyelid. Because specialized electroepilation units are designed specifically for this purpose, they are preferable. Delivery of energy to the gland is done best by guiding the needle alongside the hair shaft down to a depth of 3 to 4 mm. Positioning of the needle and energy delivery is confirmed by meibum bubbling out of the meibomian gland orifice (Figure 124-12). Destruction of the gland is confirmed when the cilia can be manually epilated as if no attachment remains. Treatment should be repeated or the power setting increased until easy manual epilation is possible. A starting setting of 0.5 is recommended for electrocautery units.79 Complications are uncommon and recurrence rates are low when a specialized electrolysis unit is used.95 Hairs, usually originating from the meibomian glands, that break through and exit the palpebral conjunctiva are termed ectopic cilia. They abrade the cornea directly and predictably cause severe pain and keratitis. Ectopic cilia are most commonly seen in young adult dogs. The treatment of choice is to remove the offending cilia and the meibomian gland from which they originate. This is most easily accomplished by placement of a chalazion clamp and excision en bloc of an approximately 1- to 2-mm2 section of tissue (down to the muscular layer) surrounding the cilia. This can be done “freehand” with a #11 Bard-Parker blade or a 6500 Beaver blade or by centering an appropriately sized dermal biopsy punch over the cilia.24 The resulting defect is not sutured. Postoperative bleeding is minimal and can be decreased by the application of 2% phenylephrine. In dogs, meibomian gland tumors, squamous papillomas, melanomas, and histiocytomas make up more than 80% of all eyelid tumors. Of these, the most common is meibomian gland adenoma. Most eyelid tumors (73%) in dogs are benign.61 In cats, the most common eyelid tumor is squamous cell carcinoma. Even though some tumors have distinctive clinical characteristics, definitive diagnosis should be reached by microscopic evaluation in all cases. Chalazia are treated by surgical removal of inspissated material. A Francis chalazion clamp is placed. The conjunctival surface over the chalazion is incised with a #11 Bard-Parker blade or a 6500 Beaver blade, and all contents are removed with a chalazion curette (Figure 124-13). Alternatively, the contents are gently expressed through the incision. The wound is left to heal by second intention; conjunctival sutures should not be placed to avoid corneal abrasion. Some advocate performing two freeze–thaw cryotherapy cycles over the affected gland because the obstruction may be caused by formation of microscopic neoplasia occluding the gland. Topical corticosteroid ointment should be applied postoperatively for 5 to 7 days. When the length of the excised margin is less than one third of the length of the eyelid margin, the defect can be closed by apposition of the cut edges. Resection should be performed in the form of a wedge or a pentagon. Then, the tarsus and orbicularis muscle layer is apposed with a horizontal mattress suture such that the plane of the bites is parallel to the eyelid margin, the knot is away from the margin, and neither the knot nor the suture is exposed through the palpebral conjunctiva. This step can be skipped with very small (i.e., 1 to 2 mm) resections and may even hinder perfect apposition in these situations. Next, the eyelid margin is apposed with a figure of eight suture. Suture tags are left long and pulled away from the eye by incorporating them into the simple interrupted sutures that are used to appose the skin distal to the eyelid margin (Figure 124-14). This technique should also be used to appose lacerations that involve the eyelid margin. Defects that involve more than one third of the eyelid margin can be reconstructed using this technique. If this technique is to be used, a rectangular excision should be performed. If the tumor does not involve the conjunctiva, the conjunctiva should not be excised so that it can be used to line the bulbar aspect of the graft. After excising the affected tissue, two slightly diverging skin incisions, two times the height of the excised defect, are made, starting at the base of the defect. Two identical triangles of skin (Burrow’s triangles), with bases approximately 20% longer than the height of the defect, are removed to accommodate shifting of the skin into the defect. The skin flap and skin surrounding the Burrow’s triangles are liberally dissected from the underlying muscle. Undermining should continue until the graft lies tensionless within the defect. A simple interrupted 5-0 or 6-0 suture is placed to join the distal corner with the proximal corner of each triangle. The flap is then positioned with a simple interrupted suture so that its leading edge sits 0.5 to 1 mm beyond the normal eyelid margin. The remaining skin incisions are apposed with simple interrupted sutures every 3 mm (Figure 124-15). The bulbar aspect of the graft can be lined with the conjunctiva from the adjacent eyelid, conjunctiva from the anterior surface of the third eyelid, a free conjunctival graft from opposite eyelid, or a free buccal mucosa graft after it has been mobilized avoid placing tension on the graft. The mucosal graft should be sutured with 6-0 to 8-0 absorbable material so sutures do not contact the cornea. This can be accomplished by beveling the leading edge of the skin graft so that the conjunctiva, when sutured to the border of the cut margin, is pulled away from the cornea (Figure 124-16). Figure 124-16 Beveling the skin margin and suturing the conjunctiva to the cut edge of the skin can help decrease trichiasis. Some advocate letting conjunctival cells spontaneously line the posterior aspect of the graft, arguing that spontaneous conjunctival healing is very rapid and may be less likely to result in traction bands in the grafted area and donor areas that could result in leading-edge entropion.119 This technique is ideal for reconstruction of defects of the upper eyelid that involve large portions of the eyelid margin and are of limited height (e.g., eyelid agenesis or squamous cell carcinoma affecting the eyelid margin). In this manner, the entire margin can be reconstructed if necessary. To create a recipient bed in cases of eyelid agenesis, an incision at the junction between the skin and the conjunctiva is made to create a fresh wound margin. A laterally based single-pedicle conjunctival flap is harvested from the palpebral surface of the third eyelid. It is rotated 180 degrees, positioned within the defect so that the underside faces outward, and sutured to the incised conjunctival edge with 7-0 or 8-0 polyglactin in a simple continuous pattern. A rectangular pedicle of skin, hinging at the lateral canthus and slightly (1 mm) larger than the recipient bed, is created by making incisions through skin and orbicularis muscles of the lower eyelid. The incision closest to the lower eyelid margin should be parallel to and about 5 mm from the margin. A lateral canthal incision is then made to allow the pedicle to be rotated into place. The leading edge of the pedicle is sutured to the edge of the normal eyelid margin with a figure of eight suture. The rest of the pedicle is then apposed routinely with simple interrupted 5-0 or 6-0 sutures. To decrease the likelihood of trichiasis from the transposed pedicle (because the hairs will now point toward the eye), the edge of the graft that will constitute the new eyelid margin can be beveled so that the conjunctiva is pulled around the edge of the new eyelid margin to reach the edge of the cut margin (see Figure 124-16). The transposed conjunctiva and skin graft are then apposed with 7-0 or 8-0 simple interrupted or continuous polyglactin sutures (Figure 124-17). If there is significant trichiasis after the site has healed, offending hairs can be removed with cryotherapy or electroepilation, as for distichiasis.129 Figure 124-17 Myocutaneous pedicle graft as described by Dziezyc and Millichamp27 for the repair of eyelid agenesis. The conjunctiva can be harvested from the anterior surface of the third eyelid as depicted or the graft can be lined with mucosa from a different site, buccal mucosa, or not lined at all. (From Moore CP, Constantinescu GM: Surgery of the adnexa. Vet Clin North Am Small Anim Pract 27:1011, 1997.) An alternative to harvesting the skin pedicle from below the lower eyelid is to harvest it from skin above the upper eyelid.75 By doing this, trichiasis should be less of a problem. Because skin from this location does not contain a section of the orbicularis muscle, mobility may be decreased after repair of large defects. Some surgeons note successful outcomes with myocutaneous flaps without concurrent conjunctival transposition.75 This technique is suitable for large upper or lower eyelid defects, regardless of their height.99 The lesion is excised in the shape of a pentagon. The skin is incised in a semicircle with a radius equal to or slightly larger than the eyelid, arching in the opposite direction of the eyelid to be repaired. A Burrow’s triangle, with base length equal to the eyelid margin defect, is removed so that the apex of the triangle points in the same direction as the arch of the incision. The skin flap is liberally undermined and transposed to cover the defect. The eyelid margin is apposed with a two-layer closure. The skin is apposed with simple interrupted sutures (Figure 124-18). The transposed skin that makes up the new eyelid margin can be lined with conjunctiva harvested from the adjacent eyelid. A lip-to-lid flap uses a portion of the upper lip for the reconstruction of large defects of the lower eyelid, providing a mucocutaneous junction that approximates the eyelid margin. Its successful use has been described in dogs98 and in cats54 as a sole procedure or as one step in the multistep reconstruction of the upper eyelid.29 An appropriate width flap to repair the defect is created so the angle of the flap is at 45 to 50 degrees to the line between the medial and lateral canthi. The incisions defining the flap should be slightly divergent to provide a wider base. The buccal mucosa is incised at least 5 mm proximal and parallel to the lip margin. The flap is then elevated so as to include the platysma muscle. Dissection should be cautious to avoid damage to the parotid salivary gland duct, facial vein, or buccal nerve. The buccal mucosal defect is apposed with 3-0 or 4-0 absorbable monofilament with buried knots. A bridging incision is then made from the rostral edge of the flap base to the eyelid defect. The flap is turned into the defect, and the mucosal surfaces are apposed with 6-0 or 7-0 polyglactin. The two margins of the transposed lip margin are apposed to the recipient eyelid margins with a simple two-layer closure (Figure 124-19). Puckers or dog ears in the skin are not removed until approximately 6 weeks after surgery, when the flap has healed completely. A right angle or T-shaped extension of the mucocutaneous lip junction can be created for repair of lateral portions of the upper eyelid in addition to the lower eyelid.
Basic Ophthalmic Surgical Procedures
Perioperative Considerations
Instrumentation and Hemostasis
Globe Exposure
Eyelids
Anatomy and Physiology
Developmental or Congenital Defects
Eyelid Agenesis
Entropion
Ectropion
Euryblepharon
Distichia
Ectopic Cilia
Acquired Disorders
Chalazion
Eyelid Reconstruction
Simple Two-Layer Closure
Sliding Pedicle Advancement Flap
Myocutaneous Pedicle Graft
Semicircular Flap
Lip-to-Lid Flap
< div class='tao-gold-member'>
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Basic Ophthalmic Surgical Procedures
Only gold members can continue reading. Log In or Register to continue