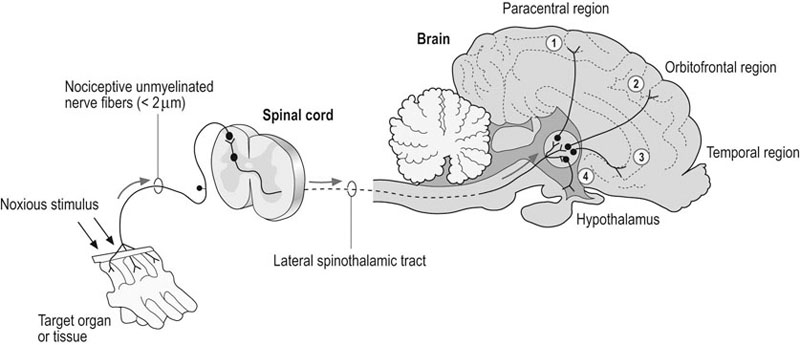
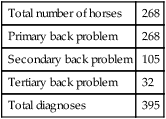
Historical reports of back disorders in horses provide few firm facts from the many lengthy accounts in old farriery and veterinary textbooks. In 1876 Lupton remarked that back injuries ‘are among the most common and least understood of equine afflictions’.1 In those days diagnosis was based simply on clinical observation (Fig. 21.1) and the opinions expressed were many and varied. These early writers were often excellent horsemen and were particularly knowledgeable on aspects of conformation. In relation to the incidence of spinal damage, Youatt believed that the short-backed horse showed less tendency to back problems and could be expected to carry more weight and possess greater endurance, but it did not have much potential for speed.2 The long-backed horse was built for speed but was much more prone to weakness when ridden. Conformationally correct horses should have a gentle ventral curve immediately behind the withers, followed by a straight line to the lumbar region. An increase in this ventral vertebral curvature (i.e. lordosis) would increase the tendency to weakness and strain. Dorsal curvature (kyphosis), however, was considered to be a more severe defect, which seriously impaired usefulness and performance. Back problems in horses cause a considerable degree of wastage and lost performance in almost all types of athletic horses. However, reports of their incidence are limited to a survey from general practice in the United Kingdom in the 1960s that showed an incidence of only 1% in 6588 horses.3 This is probably an underestimate and no breakdown of these cases into the specific diagnosis was made, but a later review of 443 horses with back problems did categorize cases further into osseous, soft tissue and miscellaneous disorders.4 Definitive diagnosis is often difficult due to vague clinical signs and the lack of good diagnostic imaging coupled with pathological reports.5,6 This has inevitably resulted in widespread controversy engendering many unsubstantiated opinions about the incidence and clinical significance of back problems, which only increase the state of confusion. Much of this controversy has resulted from the general dearth of knowledge of the functional aspects of the equine thoracolumbar spine and scientific studies on the pathogenesis of back problems in horses. It is also clear that many horses perform poorly without an underlying back problem and many other horses perform surprisingly well in spite of one. In recent years there has been an encouraging progression of studies and biomechanical research to improve this situation.7–12 There is also much more willingness for those involved with traditional methods of clinical medicine to work closely alongside those involved with spinal manipulative therapy and complementary medicine.13 The purpose of this chapter is to try and combine all these aspects for the benefit and treatment of suspected cases of back pain. 1. protection of the spinal cord and associated nerve roots (i.e. vertebral arch) 2. providing support for weight bearing and soft tissue attachment (i.e. vertebral body and vertebral processes) 3. maintaining movement for flexibility and locomotion (i.e. articulations, ligaments, and muscles). The equine thoracolumbar vertebral region consists of an average of 24 individual vertebrae, based on the typical vertebral formula (C7, T18, L6, S5, Cd15–21).14 However, variations in the number of vertebrae within the thoracolumbar vertebral region are common and are often compensated by a reduction or increase in the number of vertebrae in an adjacent vertebral region. The structural and functional unit of the vertebral column is the vertebral motion segment. A vertebral motion segment consists of two adjoining vertebrae and interposed soft tissue structures (Fig. 21.2). The typical vertebra is characterized by a vertebral body, vertebral arch and vertebral processes that vary in each vertebral region according to structural and functional demands. The vertebral body is a ventral cylindrical structure covered dorsally by the vertebral arch, which includes bilateral pedicles and laminae. Vertebral processes include one spinous process, two transverse processes and two pairs of cranial and caudal articular processes on each vertebra. Mamillary processes are additional vertebral processes found only in the thoracolumbar region that provide added paraspinal muscle attachment sites. Dorsally, the articular processes create bilateral synovial articulations (i.e. zygapophyseal joints) that provide segmental stability and mobility to the vertebral motion segment. Ventrally, the vertebral bodies and intervertebral disks form fibrocartilaginous joints that also provide segmental vertebral stability and mobility. Additional connecting soft tissues include both short and long spinal ligaments and muscles. The vertebrae, vertebral articulations and ligaments are innervated segmentally by sensory branches of the dorsal rami and recurrent meningeal nerves. These nerves mediate nociception and proprioception within the vertebral column. The vertebral bodies form the foundation on which the remaining vertebral structures are placed. The cranial vertebral body is convex in shape and the caudal vertebral body is concave (Fig. 21.2). Therefore, most equine intervertebral joints resemble a shallow ball-and-socket configuration, which provides stability without restricting mobility. Vertebral bodies provide support for weight bearing, connective tissue attachment and muscular attachment sites for the diaphragm and psoas muscles in the lumbar vertebral region. The intervertebral disks connect adjacent vertebral bodies and together are classified as fibrocartilaginous articulations. An intervertebral disk consists of an outer annulus fibrosus and central nucleus pulposus. The nucleus pulposus is rudimentary in the thoracolumbar vertebral regions compared to the cervical and caudal vertebral regions (Fig. 21.2). The dorsal and ventral longitudinal ligaments, and the costovertebral ligaments, provide additional reinforcement to the periphery of the intervertebral disk. The intervertebral disk is active in weight bearing, axial shock absorption and maintaining vertebral flexibility. The outer one-third of the intervertebral disk is innervated by both proprioceptive and nociceptive fibers. The spinous processes project dorsally from the vertebral arch and vary in size, shape and orientation in different vertebrae and vertebral regions (Fig. 21.3). The spinous processes function as a series of levers for muscle and ligamentous attachment that provide support and movement to the vertebral column. Spinal extension and rotation are produced by contraction of muscles attached to the spinous processes. The supraspinous ligament stabilizes the apex of the spinous processes and aids in resisting excessive spinal flexion. The spinous processes in the cranial thoracic vertebral region are angled caudally and elongated in the region of T2 to T12 to form the withers. The cranial thoracic vertebral region must provide a foundation for stability for and resist forces produced by the head, neck and forelimbs, whereas the caudal thoracic and lumbosacral vertebral region has to resist significant forces associated with the hind limbs and locomotion. The divergent spinous processes of the lumbosacral junction produce a wide interspinous space, compared with the adjacent interspinous spaces.15–17 The lumbosacral spinous process divergence supports an increased range of motion at the lumbosacral junction without the risk of spinous process impingement. Two pairs of cranial and caudal articular processes arise dorsolaterally from the vertebral arch. An articular surface on the articular processes contributes to the formation of bilateral synovial articulations (i.e. zygapophyseal joints). The articular surfaces in the thoracic vertebral region lie horizontally (i.e. dorsal plane) with the cranial articular surfaces facing dorsally and the caudal articular surfaces facing ventrally. Vertebral motion in the thoracic vertebral region is limited mostly to rotation and lateral bending. The lumbar vertebral region has articular surfaces that predominantly lie vertically (i.e. sagittal plane). Vertebral motion in the lumbosacral vertebral region is limited mostly to dorsoventral flexion. The articular processes function in support and movement of the vertebral arch. The amplitude and direction of segmental vertebral motion are related to the size, shape and orientation of the articular surfaces and functional status of the articulations.15,16,18 Regional and overall spinal motion is due to the cumulative effects of small amounts of segmental vertebral motion. The zygapophyseal joint capsule has a dense outer fibrous layer, vascular central layer and an inner layer consisting of the synovial membrane. The zygapophyseal joint capsule is richly innervated with sensory nerve fibers from the medial branch of the dorsal rami of several adjacent nerve roots. Proprioception and nociception are two important neurologic functions of the zygapophyseal joints.19,20 Multilevel spinal innervation of the zygapophyseal articulation produces non-localized pain patterns, which contribute to the difficulty of identifying and localizing back problems.21 The transverse processes provide support and movement to the vertebral column via muscular and ligamentous attachments. Transverse processes are used as lever arms by the deep spinal muscles to maintain posture and to induce rotation and lateral bending.21 In the thoracic region, the transverse processes contain articular surfaces that contribute to the costotransverse articulations. The lumbar vertebral region has elongated, horizontally flattened transverse processes that provide attachment sites for the large dorsal paraspinal muscles and ventral psoas muscle group. Species of the genus Equus have intertransverse synovial articulations between the transverse processes of the last two or three lumbar vertebrae and at the lumbosacral junction.15,16 Biomechanically, the intertransverse joints aid in the transfer of propulsive forces from the hindlimbs to the vertebral column and provide resistance to lateral bending and axial rotation of the spine. The pelvis articulates with the vertebral column at bilateral sacroiliac articulations, located at the junction between the ventral wing of the ilium and the dorsal wing of the sacrum (Fig. 21.4). Dynamically, the sacroiliac joints aid in locomotion via transfer of hind limb propulsive forces to the vertebral column.22 The articular surfaces of the sacroiliac joint are nearly flat and closely apposed to support small amounts of gliding movements. The sacroiliac joint is typically L-shaped with the convex border directed caudoventrally. The sacroiliac joint capsule is thin and closely follows the margins of the sacroiliac articular cartilage. The sacroiliac joint is supported by three bilateral sets of strong sacroiliac ligaments that act to support weight of the caudal vertebral column. The dorsal sacroiliac ligaments, consisting of a dorsal and lateral portion, connect the tuber sacrale to the sacrum. The interosseous sacroiliac ligaments are the most robust of the sacroiliac ligaments, spanning the space between the ventral wing of the ilium and the dorsal wing of the sacrum and function as a sling to support the entire mass of the caudal trunk. The ventral sacroiliac ligaments connect the ventral wings of the sacrum to the ilium. The sciatic nerve, cranial gluteal nerve and cranial gluteal artery and vein travel through the greater sciatic foramen, immediately ventromedial to the sacroiliac articulation, which need to be taken in consideration during caudal approaches for injecting the sacroiliac joint. A series of long and short spinal ligaments contribute to vertebral column stability. Three separate longitudinal spinal ligaments span the length of the vertebral column and provide regional vertebral stability. The nuchal ligament in the cervical vertebral region continues as the supraspinous ligament in the thoracolumbar vertebral region and joins the tips of the spinous processes. The dorsal longitudinal ligament connects the dorsal vertebral bodies within the vertebral canal and acts to reinforce the intervertebral disk (Fig. 21.2). The ventral longitudinal ligament attaches to the ventral vertebral bodies and blends with fibers of the intervertebral disk. The short spinal ligaments interconnect individual vertebral structures and function to protect the spinal cord and to provide segmental vertebral stability. Interspinous ligaments connect adjacent spinous processes. The ligamenta flava span the space between adjacent vertebral laminae and contain a high proportion of elastin. Specialized costovertebral and costotransverse ligaments provide additional stability to the thoracic vertebral region and ribs. The intertransverse ligaments connect adjacent transverse processes in the lumbar vertebral region and limit lateral bending. The intervertebral disk can be considered a specialized connective tissue structure that connects adjacent vertebral bodies. Muscles that attach only to the axial skeleton are considered intrinsic spinal muscles. The spinal musculature can be categorized into epaxial or hypaxial muscle groups based on their location relative to the transverse processes of the vertebral column. The epaxial muscles lie dorsal to transverse processes, are segmentally innervated by dorsal branches of spinal nerves and produce spinal extension and lateral bending. Hypaxial muscles lie ventral to transverse processes, are segmentally innervated by ventral branches of spinal nerves and produce spinal flexion and lateral bending. The thoracolumbar fascia is an aponeurosis that serves as an attachment site for many spinal and proximal limb muscles. The thoracolumbar fascia is strong and attaches to the thoracolumbar spinous processes and the cranial edge of the ilial wing. At the lumbosacral junction, the thoracolumbar fascia consolidates along the dorsal midline to form bilateral robust tendons that insert onto the cranial aspect of the tubera sacralia. The largest group of epaxial muscles is organized into three parallel columns. These include (from lateral to medial) the iliocostalis, longissimus and spinalis muscle groups (Fig. 21.3). The iliocostalis muscles are a thin muscle group that attaches to the angle of the ribs and the tips of the lumbar transverse processes. The longissimus muscles are by far the largest and longest group of back muscles. These muscles primarily attach to the dorsal spinous and transverse processes of the thoracolumbar vertebral region and the wing of the ilium and help to support the weight of saddle and rider. The spinalis muscles cover the lateral aspects of spinous processes of the withers and may be compromised by a narrow saddle. The transversospinalis muscle group is the deepest and most medial muscle group (Fig. 21.3) and is largely composed of multifidi muscles in the thoracolumbar vertebral region. The multifidi muscle group is a series of short musculotendinous units that originate from transverse, articular and mamillary processes and insert on adjacent spinous processes. These short muscles span 2–4 vertebrae and are segmentally innervated by dorsal spinal branches. The epaxial muscles produce spinal extension when activated bilaterally, and lateral bending and rotation when activated unilaterally. Superficial muscle groups usually span one or more vertebral regions, whereas deep spinal muscles usually only span a few vertebrae.22 The spinal musculature is important for movement, posture and flexibility. The superficial spinal muscles are usually more dynamic and play a role during regional vertebral motion, energy storage and force redistribution during locomotion.22 Deep, short spinal muscles have more of a static function and are active in segmental stabilization, proprioception and posture. Muscles that have attachments on both proximal limbs and the axial skeleton can be considered extrinsic spinal muscles (or shoulder girdle or pelvic girdle limb muscles). The general function of the extrinsic spinal muscles is to induce proximal limb movements required in locomotion or to assist vertebral mobility, depending on whether the vertebral column or limbs are held stationary relative to each other. The shoulder girdle muscles can be categorized into dorsal or ventral muscle groups.23 The dorsal muscles of the shoulder girdle act to suspend the forelimbs from the neck and trunk. The dorsal shoulder muscles include the brachiocephalicus, omotransversarius, trapezius, rhomboideus, cutaneous trunci and latissimus dorsi. The ventral muscles of the shoulder girdle function in suspending the neck and trunk from the forelimbs. The ventral shoulder muscles include the subclavius, superficial pectoral, deep pectoral and serratus ventralis. The pelvic girdle muscles are best characterized as cranial-caudal and lateral-medial muscle groups.23 The cranial muscles of the pelvic girdle function in hind limb protraction and hip flexion. Muscles in this group include the sartorius, iliopsoas, tensor fasciae latae and rectus femoris. The caudal muscles of the pelvic girdle produce hind limb retraction and hip extension. Muscles in this group include the biceps femoris, semitendinosus and semimembranosus. The lateral muscles of the pelvic girdle mostly cause hind limb abduction and include the superficial, middle and deep gluteal muscles. The medial muscles of the pelvic girdle produce hind limb adduction and include the gracilis, pectineus and adductor muscles. The hypaxial or sublumbar muscles include the psoas minor, psoas major and iliacus. The psoas minor and psoas major originate on the ventral vertebral column (T16 to L6) and insert on the pelvic inlet and lesser trochanter of the femur, respectively. Together, the psoas major and iliacus form the iliopsoas, the largest flexor of the coxofemoral joint (Fig. 21.4). If the hindlimb is stabilized, then the iliopsoas muscle induces flexion of the lumbar spine and pelvic flexion about the sacroiliac articulations. Quantifying the degree of pain in horses and establishing the precise site of pain has always been difficult24 and horses with back pain are no exception. The situation is further complicated as the major clinical sign recognized by owners in many horses with a back problem is impaired or poor performance and not overt thoracolumbar pain. On the other hand, many horses apparently perform satisfactorily in spite of some low-grade back pain. To add to this confusion, some horses appear to be naturally sensitive or ‘thin-skinned’ and resent being groomed or palpated along the back. In these patients, both owners and clinicians may interpret an evasive response to innocuous stimuli (i.e., allodynia) as a sign of back pain. Another difficulty in the assessment of back pain involves the condition known as ‘cold back’ in which there is apparent hypersensitivity over the back with a transient stiffness and extension (lordosis)) of the trunk as the rider gets into the saddle. There are usually no other demonstrable clinical signs, although in severe cases the horse may buck and rear when first mounted and ridden. In some instances the thoracolumbar spine is notable flexed (kyphosis) and the epaxial muscles are severely hypertonic. The initial stiffness from being saddled or mounted usually subsides within a few minutes and thereafter no effect on performance is noted. Whether this condition is actually painful, associated with some previous back pain or illi-fitting saddle or is merely a matter of temperament is unclear. Many of the difficulties in clinical diagnosis of back problems would be solved if some meaningful criteria for the assessment of pain and an objective system of quantifying it could be established. The origin of primary back pain is irritation of the dorsal nerve roots and the branches of the spinal nerves. The back, like most tissues of the body, is innervated nerve endings that are particularly sensitive to tissue dysfunction (Fig. 21.5). Nociceptive receptors include plexiform and free ending arrangements of unmyelinated nerve fibers. Nociceptive fibers are distributed throughout the skin and subcutaneous tissues, adipose tissues, fasciae and ligaments, periosteum, dura mater, adventitia of blood vessels and fibrous capsules of interneural articulations and sacroiliac joints. In normal circumstances this receptor system is relatively inactive but it is activated when chemical, mechanical or other damaging factors are applied to the tissues containing the unmyelinated nerve endings. Primary back pain therefore results from trauma or irritation of these nociceptive receptor nerve endings. Various other pain syndromes are recognized in humans and include secondary, referred and psychosomatic low back pain, but their importance in the horse is unproven as yet. Another important factor to be considered is the marked variation in response to pain. Even in humans a meaningful measurement of ‘pain threshold’ is unrealistic as patients can vary in the intensity of their experience of pain from day to day and even at different times during the day. In horses, temperament is considered an important factor in the assessment of both acute and chronic pain. It is suggested that the reduced performance is sometimes due to the horse attempting to guard its back even though the clinical signs of pain have abated some time previously. Some credence has been given to this idea by the induction of back pain in trotting horses and recent research into motor learning and compensatory gait mechanisms.25 The principal sign of primary induced back pain is not lameness, but stiffness and reduced performance. There have been no systematic pathological studies on a large series of back cases in horses. There have been a number of studies on congenital deformities26,27 and reports on diskospondylitis.28,29 Some investigations on acute and chronic sacroiliac disease have been reported.30,31 Much has been written about the clinical and surgical treatment of over-riding or impinged dorsal spinous processes (i.e. kissing spines),32 but very little research has been done on its etiopathogenesis. The widespread use of ultrasonography to diagnose soft tissue injuries of the epaxial structures has dramatically increased the ability to diagnose desmitis within the supraspinous and dorsal sacroiliac ligaments, but no pathological studies have been completed to confirm these clinical findings.33–35 Many back problems in horses are associated with chronic or long-standing injuries. It is also common for there to be more than one spinal lesion that contributes to the clinical signs and poor performance. A breakdown of diagnoses of one of the authors’ cases (LBJ) from 1992 to 1997 shows a total of 395 diagnoses made from 268 cases presented for examination of the back to a referral clinic (Box 21.1). It is particularly common for cases of over-riding or impinged dorsal spinous processes to be associated with injury of the supraspinous ligament, sacroiliac disease or low-grade hock lameness. Therefore confirmation of such secondary lesions can have important implications for the management and prognosis of horses with primary back problems. Opinions vary as to whether horses genuinely suffer from back problems at all or whether the signs exhibited are referable to damage elsewhere in the skeleton. In our experience genuine back problems do occur, but in a variety of forms (Table 21.1). First, there are those with identifiable lesions in the thoracolumbar spine or epaxial structures (i.e. primary back problems). A second important category are those due to secondary back problems that occur as a result of the pressure or strain exerted from lesions in the appendicular or axial skeleton (i.e. particularly fore- or hind limb lameness). Finally, there is a category of apparent or alleged back problems which, despite popular opinion, have limited anatomic or pathophysiologic evidence to support their occurrence (Table 21.2). This group of ‘back problems’ forms the basis of much controversy between veterinarians and other professionals (e.g. chiropractors) or non-professionals (e.g. lay practitioners). These difficulties are exacerbated by the fact that many horses suffer low-grade and chronic lesions. Malalignment or displacement of the caudal thoracic or lumbar dorsal spinal processes is reputed to be a common cause of back trouble in horses.36 One or more spinous summits are said to become laterally displaced (i.e. ‘out of place’) and these can apparently be replaced by sharp pressure at the appropriate site (i.e. ‘put back into place’). From an anatomic point of view this claim is not acceptable; these structures are not moveable like this either in life or at post-mortem. In spite of the tendency for intervertebral disks to degenerate with age in the thoracolumbar spine, they do not appear to cause any clinical signs similar to those seen so commonly in humans and in dogs. Nerve ‘pinching’ and peripheral nerve lesions are often claimed to be important causes of back problems, but as yet there has been no scientific evidence to substantiate this belief in horses. However, anecdotal necropsy evidence does support the existence of spinal nerve compression at the lumbosacral junction (i.e., L6 ventral spinal nerve) due to bony proliferation and osteophytosis at the associated intervertebral foramen adjacent to the medial aspect of the L6-S1 intertransverse joints, which would be expected to produce similar clinical signs to ‘sciatica’ or lumbar spinal nerve compression in humans. Table 21.1 Differential diagnoses to consider for a horse with potential back problems Table 21.2 Conditions alleged to cause back problems in horses for which there is currently no definitive scientific evidence Many of the problems causing poor performance in horses are long-standing (i.e. many weeks or months in duration) and there is a tendency for these cases to recover spontaneously. In a survey of cases followed over two years, a 65% recovery rate was reported irrespective of the diagnosis and the treatment or management regime.5 The prevalence of spontaneous recovery therefore can hamper elucidation of diagnosis and make evaluation of treatment regimes difficult. Lameness is not a typical feature of horses suffering primary back problems. However, secondary back pain is often associated with lameness as the underlying condition causing poor performance. Most primary back cases exhibit only low-grade hind limb lameness, which is often bilateral and most commonly associated with hock injury. A study in which back pain was induced using lactic acid injections into the longissimus muscles did not produce any signs of hindlimb lameness.25 However, in other studies that evaluated naturally-occurring clinical cases of thoracolumbar or sacroiliac pain, the prevalence of limb lameness varied from 35% up to 74–85%.37–39 Conversely, in horses presented for primary limb lameness, the prevalence of back problems varied between 23–32%.38,39 Therefore, it appears that a large percentage of horses with back pain have concurrent lameness versus a smaller proportion of horses with lameness also have back pain. The clinical significance of this is that practitioners that focus solely on back problems (e.g., equine chiropractors) are likely not addressing concurrent lameness issues if they are not collaborating with limb lameness specialists. Conversely, practitioners that focus solely on limb lameness without considering the potential adverse effects on spinal function are likely not providing comprehensive treatment of musculoskeletal pain and poor performance. Causes of sacroiliac joint pain or injury have been postulated to be the result of sacroiliac or lumbosacral osteoarthritis, sacroiliac desmitis or sprain, sacroiliac subluxation or luxation, pelvic stress fractures, complete ilial wing fractures or sacral fractures.40 Additional differential diagnoses include thrombosis of caudal aorta or iliac arteries, exertional rhabdomyolysis, trochanteric bursitis and impinged dorsal spinous processes in the lumbar vertebral region.41 Horses with presumed thoracolumbar vertebral problems may also have concurrent chronic sacroiliac joint injuries. In a report on 443 horses with back problems, chronic sacroiliac joint problems were identified in 15%.4 Clinical signs of lower hind limb lameness may overlap and mimic signs of presumed sacroiliac joint pathology. It is important that a thorough and complete lower limb lameness evaluation is completed prior to or in conjunction with a proximal hind limb or sacroiliac joint work-up. A standardized protocol should be used to systematically examine horses with potential back problems (Box 21.2). The value of obtaining a thorough clinical history cannot be overestimated, as the clinical signs and behavioral changes of thoracolumbar disorders are many and varied.42 Details dating back to the time when the owner first acquired the horse are extremely helpful in deciding whether or not one is dealing with a genuine back problem. In this regard, information on management, tack and performance should always be sought. There also seems to be an association with the type of back injury and the type of work the horse is involved in. Jeffcott reported that the differences in incidence of specific back problems varied quite noticeably according to whether the horse jumped at speed, jumped competitively or was not used for jumping at all.5 Acute sacroiliac strain or subluxation was more prevalent in horses jumping at speed, whereas impinged or over-riding dorsal spinous processes were most common in showjumpers. The incidence of soft tissue damage was much the same in both of these groups and age was not nearly such an important factor in equine back disorders as it is in humans. Spondylosis appeared more frequently in mares, whereas over-riding dorsal spinous processes was most often seen in short-backed Thoroughbred geldings. Query into the size and the time spent in stalls, paddocks, or turnout in pasture is indicated for any horse with back problems. In humans, a primary contributing factor for recurrent back problems is bed rest and inactivity.43 Horses that are stalled for the majority of the day or large portions of the year do not have the opportunity to maintain back flexibility, which may contribute to back stiffness and dysfunction. In addition, horses that are turned out in paddocks with knee-deep mud, large rocks, poor footing or steep hills may aggravate pre-existing back problems. The conformation and intended use of the horse can have an important bearing on the injury involved. For example, specific spinal malformations (e.g. lordosis and scoliosis) tend to predispose to injury through the inherent weakness of the thoracolumbar spine.5
Back and pelvis
Introduction and historical perspectives
Anatomic and functional considerations
Thoracolumbar vertebral column
Vertebral motion segment
Vertebral body and intervertebral disk
Spinous processes
Articular processes
Transverse processes
Sacroiliac joint
Spinal ligaments
Intrinsic spinal muscles
Extrinsic spinal muscles
Diagnostic challenges
Back problems – a syndrome
Back pain perception
Dearth of appropriate pathological studies
Frequency of multiple lesions at multiple sites
Types of back problems
TYPE OF BACK PROBLEM
GENERAL CATEGORY
SPECIFIC LESION OR PROBLEM
Primary back problem
Soft tissue injury
Longissimus muscle strain
Supraspinous ligament sprain or desmitits
Dorsal sacroiliac ligament sprain or desmitits
Exertional rhabdomyolysis (tying up)
Non-specific soft tissue injury
Osseous injury
Conformational or developmental abnormality
Over-riding or impinged dorsal spinous processes
Osteoarthritis (e.g. articular processes)
Vertebral fracture
Spondylosis
Diskospondylitis
Spinal neoplasia (primary and secondary)
Neurologic disorders
Equine protozoal myeloencephalitis (EPM)
Equine degenerative myeloencephalopathy (EDM)
Equine herpesvirus myeloencephalitis (EVH-1)
Equine motor neuron disease (EMND)
Tack associated
Poor saddle fit or excessive pressure
Idiopathic
No clinical abnormalities detected
Secondary back problem
Hindlimb lameness (e.g. spavin), Forelimb lameness
Neck problem (e.g. stenotic myelopathy)
Acute sacroiliac injury
Chronic sacroiliac disease
Pelvic fracture
Presumed back problem
Bad temperament
Lack of ability (rider or horse)
Lack of fitness
Improper tack fit or use
Dental problems
GENERAL CATEGORY
SPECIFIC LESION OR PROBLEM
Vertebral subluxation
Subluxation of thoracolumbar vertebral bodies or articular processes
Misalignment of thoracolumbar dorsal spinous processes
Intervertebral disk injury
Intervertebral disk prolapse or herniation
Peripheral neuropathy
Compromise of thoracolumbar spinal nerves at the intervertebral foramen
Frequency of spontaneous recovery
Relationship of back pain to lameness
Diagnostic protocol to assess back problems
History
Use of the horse
Management and training ability
Predisposing factors
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Back and pelvis