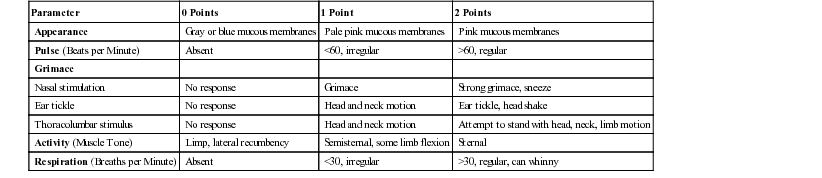
Guy D. Lester, Consulting Editor Jane E. Axon A normal foal should have righting reflexes and sufficient muscle tone to be able to right itself to sternal recumbency within 2 to 3 minutes of birth. By 5 minutes the foal should be bright, alert, and responsive to visual, auditory, and tactile stimuli. Over the next 20 to 25 minutes the normal foal will be restless, alternating periods of sternal recumbency with lateral recumbency before beginning lurching attempts to stand. During this period the foal will often vocalize in response to maternal sounds or contact. Once standing, the initial posture is an unsteady basewide rocking stance, but this slowly improves such that by 60 minutes the foal should be standing securely without assistance. The suckle reflex is present within minutes of birth in most foals and should be present in all foals by 30 minutes. Once standing, the foal will seek the udder, a process that is initially very clumsy but improves once the foal has successfully sucked. There will be repeated nudges of the udder in order to facilitate milk letdown. The normal foal should be nursing from the mare within 2 hours (mean time of 111 minutes; range, 35 to 420 minutes), and most have nursed twice by 2.5 hours.1 Sucking periods vary in duration between 1 and 5 minutes and are interspersed with periods of sleep that last around 7 minutes. It is important to watch the foal during sucking to confirm appropriate teat contact and swallowing movements. A foal that spends long periods at the udder may do so because of inability to nurse or inadequate milk from the mare. The daily milk consumption of most newborn foals is between 21% and 25% of their body weight.2 This equates to around 12 to 12.5 L/day for a 50-kg foal. Based on the caloric density of milk, this reflects a daily intake of 120 to 150 kcal/kg body weight; half of this is used for basal metabolism and thermoregulation and half for growth. Sleep periods first occur between 90 minutes and 4 hours after birth and last for about 7 minutes.3 The foal spends one third of its time lying down during the first 2 months of life—compared with 5% to 10% for adults, most of which occurs overnight. Foals do not learn to follow their dams to the exclusion of any other moving object for the first 1 to 2 weeks of life. Foals identify their dams by sight and smell, and during the first week of life, they spend 85% of the time within 1 m of the dam, 94% to 99% within 5 m, and only very rarely are more than 10 m away from the dam.4 Loss of affinity for the mare in a foal that seems otherwise healthy may be an early sign of the neurologic form of hypoxic-ischemic syndrome. Recommendations to clients as to when veterinary intervention should be sought vary from practice to practice. The “1-2-3” rule states that foals should be standing unassisted by 1 hour, sucking from the mare by 2 hours, and the mare should have passed her fetal membranes by 3 hours. Clients may adopt a similar “2-4-6” rule to seek veterinary attendance, in which intervention should be sought if the foal has not stood by 2 hours, not sucked by 4 hours, or the fetal membranes are still in place by 6 hours. These recommendations are only used as a rough guide and will obviously be influenced by peripartum conditions and client experience. A modified Apgar Score (Table 16-1) has been used in foals to semi-quantitate the severity of signs that occur in response to peripartum asphyxia.5 The acronym used in equine practice differs from that used in human medicine and refers to appearance, pulse, grimace, activity, and respiration. Appearance refers to oral mucous membrane color; pulse uses 60 beats/min as a cut off; grimace is assessed in response to stimulation of the nasal mucosa, inside of the pinnae, and over the thoracolumbar area adjacent to the spine; activity reflects the degree of muscle tone; and respiration refers to ventilation rate and rhythm with 30 breaths/min as the cut off. Each category is scored from 0 to 2 points with a score of 10 being optimal. A score of 0 to 3 indicates marked depression; 4 to 6, moderate depression; and 7 to 8, mild asphyxial injury. Normal foals have a score of 9 or 10. Ideally the modified Apgar calculation should be made within the first minute after birth, but certainly within 15 minutes of delivery. Repeating the score 4 minutes later is recommended. Foals with low scores typically require aggressive resuscitation, whereas mildly affected foals may respond to vigorous rubbing, stimulation of the nasal mucosa, and limb movement. TABLE 16-1 Apgar Score: Assessment of Neonatal Asphyxia19 The behavior of the mare is critical and must be closely monitored. A good dam will pay close attention to its foal avoiding stepping or lying on it, protecting it from real or perceived threats, and facilitating the nursing process. The mare and foal will be in close contact over the first few days of life, within 5 m of each other for more than 95% of the time. Signs of concern are mares that avoid their foal, do not allow the foal to nurse, or are outwardly aggressive toward the foal.6 It has been reported that maiden mares, older mares, mares with a history of rejecting foals, and Arabian mares of Egyptian lineage are at greatest risk of rejecting their foals.7 The health of either the foal or the mare can contribute to a failure to bond. For example, foals that are unable to stand or unable to suck are less likely to form a normal bond, and mares with painful mammary glands, or that are experiencing strong postpartum uterine contractions, are less tolerant of foals trying to suck. There are numerous factors that influence a foal’s body weight at birth, including breed, gender, gestational age, and intra-uterine environment. Estimates of body weight for newborn Thoroughbred foals for the purpose of drug calculation range between 40 and 55 kg, although many healthy foals may well exceed this range. The average daily weight gain for healthy foals is breed dependent but is typically between 1.3 and 1.7 kg/day for Thoroughbred-type foals.8 Daily weight gain in hospitalized foals is determined by disease, calorie intake, and a lack of exercise, and is almost always less than that of healthy, active foals. The degree of physical development should be considered in relation to the estimated gestational age. This assessment should be made in light of the variable gestational length in horses. Typically gestational length is calculated from the time of insemination through to birth—a figure that overestimates the true gestational period by as much as 7 days. The mean gestational period in Thoroughbreds is around 340 to 342 days, with 95% of mares foaling between 327 and 357 days.9 A number of factors influence this period, including breed, gender, and time of year. Colts on average have a gestational length that is approximately 1.5 to 2.5 days longer than that of fillies; they are slightly heavier, slower to stand, and have a heavier placenta.10 Mares that conceive early in the breeding season have pregnancies that may be up to 10 days longer than those that become pregnant late in the season.9,11 The role of dam, sire, and the dam’s sire in determining gestational period has been suggested in some, but not all, breeds.12 Physical characteristics of immaturity include low birth weight, small body size, short and shiny haircoat, doming of the head, periarticular laxity, and droopy ears. Foals with a shortened gestational period and signs of physical immaturity are termed premature, whereas foals that are physically immature in the face of an appropriate gestational length are termed dysmature. Foals born after 356 days should be regarded as post-term. This is distinguished from foals that are post-mature, a condition of increased morbidity as a consequence of failing placental function.12 Post-mature foals tend to have a lean and lanky physical appearance. Rectal temperature in normal foals ranges between 37.2° and 38.9° C (99° F and 102° F) during the first 4 days after birth.1 The upper end of the normal range, which is around 0.6° C (1° F) above the upper end of the adult range, is strongly influenced by environment and exercise. Temperature can be variable in foals with systemic sepsis; in the early stages of sepsis, the rectal temperature is commonly within the normal range or mildly elevated. Foals in septic shock will usually have a low rectal temperature, and those with localized infection will often be afebrile. The ears of a normal foal are typically erect at the time of birth. Drooping of the ear pinnae is most commonly associated with prematurity or dysmaturity, and as such, is often accompanied by other physical signs of immaturity, such as small body size, short silky haircoat, and a domed head. Practitioners should examine inside the ear pinnae for evidence of dermal hemorrhages, because these can be a manifestation of systemic sepsis (see Chapter 17) or thrombocytopenia caused by disseminated intravascular coagulation (DIC) or alloimmune thrombocytopenia. The neonatal foal may not be able to close its eyelids completely (lagophthalmos), has reduced production of tears, and lacks a menace response. The menace response is a learned one and is usually acquired in the first 14 days of life. The pupil is oval, and pupillary light reflexes are present from birth, but are slower. Other normal ocular findings include persistence of the hyaline artery remnants, the blood supply to the developing lens, and a pale pink to red optic disc with smooth margins. Newborn foals also have very prominent lens Y sutures. Lens suture lines are apparent in most foals and can persist into adulthood. In an ophthalmic survey of older foals (mean age of 9.4 weeks), suture lines were observed in 95% of animals.13 The anterior suture was predominantly Y-shaped, but the authors reported that posterior sutures were more variable, from “Y-shaped to sawhorse, to stellate.” Posterior lens sutures are reportedly more difficult to recognize in Thoroughbred foals. The suture patterns are not consistently symmetric between eyes. Prominent lens sutures can be confused with congenital cataracts. Congenital cataracts are amenable to surgery in the absence of uveal tract inflammation, a normal retina, and an appropriate demeanor. Other abnormalities that can occur include atresia of the nasolacrimal system, dermoids, retinal dysplasia, and optic nerve hypoplasia. The neonatal foal may have significant corneal ulceration without tearing, blepharospasm, or photophobia as a result of reduced corneal sensitivity when compared with older foals and adult horses.14 Consequently, special attention is required to monitor for ocular disease. A daily fluorescein stain of the cornea in sick recumbent neonatal foals is recommended. The combination of lagophthalmos, recumbency, and seizure predisposes foals with encephalopathy to a high incidence of corneal ulceration. Entropion (inward rolling of the eyelid margin) is the most common ocular problem of newborn foals. This usually occurs as a complication of dehydration and malnutrition and may lead to corneal abrasion and ulceration. Treatment is placement of vertical mattress sutures or staples to evert the offending lid while the primary condition is corrected. An alternative strategy is to inject procaine penicillin G subcutaneously into the lower lid to cause temporary eversion. Examine the conjunctiva and sclera for signs of hemorrhage. This is commonly associated with birth trauma, and affected foals should be monitored closely for development of more classical post-asphyxia complications. Episcleral injection (engorgement and proliferation of scleral vessels) is a prominent feature of systemic sepsis. Iridocyclitis is usually associated with systemic sepsis and can include hyphema, hypopyon, and fibrin. These changes are not uncommon in foals with in utero–acquired infection and may be present at birth. Iridocyclitis is also seen in older foals with Salmonella or Rhodococcus equi infection. Oral mucous membranes in healthy newborn foals should be pink, moist, and have a capillary refill time (CRT) of 1 to 2 seconds. Bright pink to red mucous membranes, accompanied with injected scleral vessels and hyperemia of the coronary bands, are consistent with the early stages of sepsis. During this early hyperdynamic phase the CRT may be shorter than normal. Darkening of mucous membranes with a delay in the CRT may indicate sustained sepsis. In severe cases, this is accompanied by petechial or ecchymotic hemorrhages. Icteric mucous membranes are most commonly associated with systemic sepsis, but are also a feature of neonatal isoerythrolysis (NI), liver disease, internal hemorrhage, meconium retention, or infection with equine herpesvirus type 1. Pale membranes suggest anemia and can occur with external umbilical cord hemorrhage, internal hemorrhage from torn umbilical vessels, fractured ribs, or hemorrhage within gastrointestinal or urinary tracts. Pallor with icterus would normally indicate NI or internal hemorrhage. Petechial or ecchymotic mucosal hemorrhages suggest advanced sepsis when associated with darkened membranes and a prolonged capillary refill time, or alloimmune thrombocytopenia when the membranes are pink (Fig. 16-1). Blue to gray discoloration of the membranes is consistent with hypoxemic circulatory shock. Overt cyanosis is uncommon and should prompt close examination of the cardiovascular and respiratory systems. In term foals, the central incisors usually erupt during the first 5 to 7 days of postnatal life. The middle incisors rise between 4 and 6 weeks of age, but the corner incisors do not erupt until around 6 to 9 months. In miniature horses and ponies, the eruption of the middle and corner incisors is delayed at 4 months and 12 to 18 months, respectively. The 12 temporary molars are present at birth or erupt within the first week of life. These teeth are replaced by permanent premolars at 2.5, 3, and 4 years of age. The three molar teeth do not erupt until 1, 2, and 3.5 years of age for molars 1, 2, and 3, respectively. Dental problems are uncommon in foals with the exception of those associated with facial deformities such as maxillary prognathism, mandibular prognathism, and campylorrhinus. Maxillary prognathism (parrot mouth; bird face; overbite; brachygnathism; brachygnathia) describes the condition in which the mandible is shorter than the maxilla, producing an overjet or overbite. The condition may affect the incisors, check teeth, or both, and is the most common congenital oral malformation of foals. The majority of foals with maxillary prognathism suffer little impact to their quality of life, and the defect simply represents a cosmetic problem. In moderate to severely affected foals, the lack of incisor contact results in excessive growth of the lower teeth and secondary soft-tissue trauma to the palate caudal to the upper incisors. The premaxilla and incisive bones tend to bend forward and downward as growth continues because of the lack of an opposing force, normally provided by the mandible. This can lead to difficulty in grazing. Mandibular prognathism (sow mouth; monkey mouth; brachygnathia superior; underbite) describes the condition in which the maxilla is shorter than the mandible, producing an underbite. The condition occurs much less commonly than the maxillary equivalent and is most frequently seen in pony and small horse breeds. The defect in its most severe form can be associated with deformity of the nasal passages and nares, and there may be difficulty in breathing and an inspiratory stridor. Campylorrhinus lateralis (wry nose; wry face) describes the condition in which the premaxilla and nasal septum are deviated laterally. It may occur singularly or in combination with other deformities, such as wry neck, cleft palate, and maxillary or mandibular prognathism. If the deviation is severe, the foal may have great difficulty in sucking from the mare. There may also be problems with breathing. In most foals the deviation is mild and represents a simple but obvious cosmetic defect. Close attention must be paid to dental wear as maxillomandibular malocclusion occurs commonly. Cleft palate is an uncommon congenital defect of foals that results from incomplete fusion of the lip and/or secondary palate during the early gestational period. Previous reports estimate the incidence at 0.1% to 0.2% of all horse births.15 Almost all clefts occur in the secondary palate, the horizontal partition dividing oral and nasal cavities. The secondary palate includes all of the soft palate and most of the hard palate, with the majority of the defects restricted to the soft palate. The basis of this congenital defect is not known but could include a heritable component and/or exposure of the developing fetus to infection, toxins, or nutritional disturbances. The diagnosis is usually straightforward and centers on an appropriate history and signalment. Confirmation is through palpation using the third finger of an upturned hand, or by direct inspection of the oral cavity. It is important that the hand is clean before direct palpation. Endoscopic examination of the nasal passages or through the oral cavity under anesthesia may be required to detect small defects. Oral palpation is recommended for all sick neonatal foals prior to commencing potentially costly treatment. A cleft in the secondary palate permits the oral contents to pass directly into the nasopharynx and nasal passages. Consequently, the most common complaint is nasal regurgitation of milk immediately after sucking. As the foal matures, feed particles will also appear at the nares. Foals with small palate defects may have intermittent milk drainage from the nostril and consequently escape diagnosis during the neonatal period. Rarely, cases are initially diagnosed in adult horses. Most will develop an aspiration pneumonia that can be difficult to identify in its early stages because of immaturity of cough receptors. Surviving foals will typically be poorly grown and ill-thrifty. The presence of milk at the nares after feeding does not definitively indicate that a cleft is present and is more commonly associated with pharyngeal/laryngeal weakness or incoordination. The tongue should be examined for evidence of candidiasis, appearing as small white plaques through to diffuse, thick, tan discoloration of the tongue. The condition can be local or systemic and is common in debilitated foals and those that have been on chronic antibiotic therapy. In severe cases the condition will cause reduced nursing and salivation. Hypertrophy of the thyroid gland (goiter) can occur in response to deficient or excess dietary iodine. One of the more common reasons for thyroid gland enlargement in neonatal foals is excess iodine supplementation during pregnancy.16 Reports exist regarding neonatal goiter when seaweed was incorporated into the diet of broodmares or when pellets were fed to mares that had been formulated with excessive iodine.17,18 Dysmature foals with thyroid hyperplasia and concurrent musculoskeletal problems have been identified in western Canada and the northwestern United States.19,20 The syndrome results in hypothyroidism and may be related to the feeding of diets that are high in nitrate or low in iodine to mares during pregnancy. Thyroid hormone is an important cofactor in maturation of the respiratory system, and hypothyroidism has been linked to respiratory failure in a newborn foal.21 In older foals, enlargement of the thyroid has been associated with dietary iodine deficiency and low circulating levels of T4.16 Newborn foals have baseline T3 and T4 levels that are considerably greater than that of adult horses.22 These levels decline over the first 12 days after birth. A number of congenital anomalies affect the alignment of the vertebral column. These include atlantoaxial malformations, scoliosis, kyphosis, lordosis, and combined anomalies, such as kyphoscoliosis. Atlantoaxial malformations may occur with or without cervical scoliosis or signs of spinal cord compression. Arabian foals are most commonly affected, and a familial predisposition has been suggested.23 There may be palpable abnormalities of the atlas and axis and altered head carriage. The diagnosis is confirmed using radiography where a range of abnormalities are seen, including atlantooccipital fusion, hypoplasia of the dens, and axis malformation. Prognosis is very poor because many have signs of ataxia and paresis involving all four limbs at birth. Some animals may have normal neurologic function. Foals with severe kyphosis or kyphoscoliosis often have underlying malformation of the thoracic vertebrae.24 Most foals display abdominal straining within a few hours of birth and pass most of the meconium within the first 1 to 4 hours after delivery, but passage may be delayed without concern for up to 12 hours. Differentiating straining to defecate from meconium impaction with straining to pass urine can be difficult in some foals. Typically foals straining to pass feces will have an arched appearance to their hindquarters (Fig. 16-2). A change in the color and consistency of the feces from a dark brown to black pasty material to a lighter brown, less tenacious material indicates that the meconium has been passed. The routine administration of an enema is performed commonly in healthy newborn foals in an attempt to reduce the straining associated with the passage of meconium. A variety of methods are used, with commercial glycerine phosphate–based products being the most common. These are relatively easy to administer, although care should be taken to avoid direct trauma to the rectal mucosa with the applicator tip. Many veterinary practices probably use gravity enemas, with 400 to 800 mL of warm soapy water delivered through a soft tube, such as a canine stomach tube or male urinary catheter. Acetylcysteine retention enemas are not administered routinely, but rather in foals with resistant meconium impactions. Auscultation of the abdomen can provide an indirect assessment of intestinal contractility. The technique should be interpreted with caution as the presence of borborygmi does not equate to propulsive motility or ingesta transit. The changes in gastrointestinal sounds over time may be more useful in determining a diagnosis. For example, a silent abdomen that progresses to a hyperactive one could be indicative of inflammatory intestinal disease, whereas an abdomen with normal sounds that change to silent could be consistent with a surgical lesion. Percussion and ballottement are used to differentiate abdominal distention caused by gas or fluid accumulation. A tympanic sound on percussion is consistent with intraluminal or free peritoneal gas, and ballottement can detect waves of free abdominal fluid. Progressive abdominal distention, irrespective of the underlying cause, can be monitored using a soft measuring tape repeatedly positioned over small clipper marks. Gastric distention can cause a “sprung rib,” a swelling that projects beyond the 18th rib. Firm structures can be detected using transcutaneous abdominal palpation, assuming the foal is suitably relaxed. It is possible to palpate bowel impacted with meconium, fecoliths, intussusceptions, the urinary bladder, or enlargement of the internal umbilical remnants caused by infection or hemorrhage. The external umbilicus should also be palpated for enlargement or herniation; in colts, the inguinal rings and scrotum should be assessed for bowel herniation. These are typically soft and fluctuant swellings that are easily reduced when the foal is placed on its back and are managed by manual reduction and strapping. Incarceration is rare but bowel integrity can be assessed using ultrasound; devitalized bowel lacks motility and has a thickened and edematous wall. In some colts the intestine can protrude through a rent in the parietal vaginal tunic and migrate subcutaneously in what is described as a direct inguinal hernia25 (Fig. 16-3). This is often associated with prepucial swelling and requires surgical intervention. Digital rectal examination is indicated in a colicky foal or in any foal in which meconium passage has not been observed. Distal meconium impaction is typically apparent on rectal examination but high impactions are not. Intestinal atresia should be suspected if there is no history of fecal passage and clear or white mucus appears on the glove. Passage of a nasogastric tube is an often overlooked diagnostic procedure in colicky neonatal foals. Removal of gastric fluid can reduce or eliminate colic signs as well as aid in the localization of disease. Gastric distention may also be present in sick neonates showing no signs of colic. The condition occurs with primary gastric outflow problems or mechanical or functional small intestinal obstruction. Functional obstruction caused by small intestinal ileus occurs more commonly in neonates as a result of a range of diseases, including hypoxic ischemic syndrome, sepsis, prematurity, enteritis, electrolyte derangements, and overfeeding. Coprophagy is observed in normal foals from birth through 5 to 6 months of age.26–28 Most foals demonstrate coprophagy by 7 days of age (Fig. 16-4). The consumption of feces is not driven by hunger, and foals have a selective preference to consume feces of their dams. The most likely basis for coprophagy is as a mechanism to populate the intestinal tract with bacteria, fungi, and protozoa essential for digestion of an herbivorous diet. Coprophagy precedes the passage of protozoa in foal feces and the development of the syndrome known as “foal heat diarrhea.” This is a benign diarrheal disease of newborn foals and should not require treatment. Ultrasound is a key component in the examination of a foal abdomen. Numerous conditions are recognized on ultrasound, including uroperitoneum, bacterial peritonitis, hemoperitoneum, strangulating intestinal obstructions, meconium impaction, gastric enlargement, enteritis, necrotizing enterocolitis, and hernias. The foal can be scanned in lateral recumbency or standing; the latter is preferred because thickened or heavy structures will move to the dependent region of the abdomen, gas-filled structures will migrate dorsally, and visualization of peritoneal fluid is improved. Clipping is not essential if the hair is dampened with alcohol. The stomach is identified in the mid to ventral abdomen on the left side between the 6th and 12th intercostal spaces (ICS) and lies medial to the spleen. In contrast to adults, the stomach is commonly in contact with the ventral body wall during the first week of life and the contents are readily imaged.29 Gastric wall thickness is typically around 2.0 mm during the first week of life. The duodenum is readily located in normal foals on the right side of the abdomen between the ventral and caudal aspect of the liver and the dorsal margin of the right dorsal colon, as well as ventral to the caudal pole of the right kidney. The remainder of the small intestine is also easily identified throughout the abdomen and should have a wall thickness less than 2.5 mm. The large intestine is differentiated from the small intestine by increased luminal diameter, bowel sacculations, and greater likelihood of gas. The colon wall should be less than 2.8 mm during the first week of life. The neonate with acute colic should be assessed with ultrasound for small intestinal intussusception. These are readily identified, are typically jejunojejunal, and are often located in the ventral abdomen when the foal is standing. They have a characteristic appearance with the intussusceptum surrounded by fluid and the intussuscipiens creating a “target” sign. Some will resolve spontaneously but most require surgical reduction. Meconium impactions have an echogenic ball or log appearance when in the small colon, or a more varied appearance when present in the large colon, a hypoechoic to hyperechoic mass that may be surrounded by fluid.30 Thickening of the wall with intramural gas echoes is consistent with a strangulated obstruction or necrotizing enterocolitis. Abdominal hemorrhage results in a classical “smoke swirl” appearance to the peritoneal fluid. Radiography has been displaced as the principal imaging modality of the foal abdomen but still can provide essential information.31 Contrast radiography remains an important technique to assess gastric outflow problems, intestinal transit, intestinal atresia, and high meconium impaction. The abdomen of most neonatal foals can be captured on a 35- × 43-cm cassette. A grid should be used to minimize film fogging. For a standing foal weighing around 50 kg, using a 400-speed film-screen system, a grid with a 10 : 1 grid ratio, and a focal spot-film distance of 100 cm, the appropriate technique should be in the range of 80 to 90 kV (peak) and 15 to 20 mA. This technique can be reduced slightly with lateral projections in the recumbent foal. The beam should be centered on the last rib. For upper GI contrast studies, 5 mL/kg of 30% wt/vol barium suspension is administered through a nasogastric tube; ideally foals are fasted for 4 hours before the procedure and should not be sedated. Barium typically empties rapidly from the stomach, allowing examination of the stomach and duodenum on initial films. The contrast should clear the small intestine by 3 hours and be completely cleared by 36 hours. The cecum should visible by 1 to 2 hours after administration. A barium enema can be used to evaluate the lower intestinal tract, specifically intraluminal obstruction and atresia. Sedation can be used because the procedure is not defining a dynamic problem. A 30-French Foley catheter with a 30-cm3 balloon is inserted 6 to 10 cm into the rectum, the cuff inflated, and 300 to 500 mL of 30% wt/vol barium sulfate suspension infused. Volumes up to 20 mL/kg have been described; colonic or rectal rupture is a rare, but fatal, complication of the procedure. Computed tomography (CT) is an underutilized tool in the assessment of the foal abdomen, with most applications involving examination of limbs, head, or neck.32 Peritoneal fluid can also be evaluated by abdominocentesis. The technique has a greater complication rate in neonates, and ultrasound should be used to identify pockets of fluid for sampling. Most complications arise as a result of a combination of hypodermic needles, a moving patient, and a relatively thin bowel wall. If no fluid is identified, the procedure should not be performed. For small volumes it is recommended to use a blunt, small bovine teat cannula; for larger volumes a hypodermic needle can be used. Peritoneal fluid–nucleated cell counts are lower in foals than in adult horses.33 Nucleated cell counts above 1.5 × 109/L may be considered abnormal in foals up to 4 months of age,34 although another study suggested a value of 3.0 × 109/L as a cutoff for foals less than 75 days of age.35 Cytologic evaluation is similar to adults with a predominance of large mononuclear cells (macrophages and mesothelial cells) with smaller numbers of lymphocytes and neutrophils. The relative percentage of neutrophils (15%) may be less than that seen in normal adult peritoneal fluid. The protein concentration of foal peritoneal fluid is similar to that of adults, below 20 g/L, and therefore values above this are considered abnormal. An increased total nucleated cell count, increase in the percentage of neutrophils with cell degeneration, and intra- and extra-cellular bacteria would be expected in foals with septic peritonitis. This would be accompanied by a low pH (<7.2), increased lactate concentration, and a discrepancy between serum and peritoneal glucose concentrations (>2.7 mmol/L).33 Physical assessment of the cardiovascular system includes examination of visible mucous membranes, palpation of peripheral arterial pulses, assessment of extremities for warmth, detection of limb or ventral edema, and cardiac auscultation. The heart rate in newborn foals in the minutes after birth is influenced by vagal tone and varies between 36 and 80 beats/min. As the foal becomes active and struggles to stand, the heart rate will increase to 120 to 150 beats/min before stabilizing in a range of 80 to 100 beats/min over the first week of life.36 Tachycardia is an important mechanism in neonates to improve cardiac output and blood pressure, and it is expected during periods of asphyxia and in response to hypovolemia, sepsis, anemia, or hypoxemia. A sustained increase in heart rate may also accompany pain or stress, or reflect a primary cardiac problem. Bradycardia can be due to hypothermia, electrolyte abnormalities, or hypoglycemia. Cardiac arrhythmias are rarely recognized but occur in most foals during the immediate postpartum period with supraventricular premature contractions and sinus arrhythmia predominating.37,38 Other arrhythmias include atrial fibrillation, ventricular premature contractions, ventricular and supra ventricular tachycardia, and idioventricular rhythm. These rhythm disturbances typically only last for 5 minutes and in most foals have disappeared by 15 minutes of age. Rarely they may persist up to 2 hours of age. The more severe arrhythmias are associated with a lower arterial oxygen concentration, suggesting a role for hypoxemia in the pathophysiology of these events. Arrhythmias that persist beyond this time frame should be investigated by electrocardiogram (ECG). Causes include electrolyte abnormalities, persistent hypoxemia, and sepsis. Cardiac murmurs are expected in the early neonatal period. A patent ductus arteriosus (PDA) can result in a continuous machinery murmur with a point of maximal intensity high over the left heart base in the 3rd intercostal space.39 These are typically audible up until 3 to 4 days of age.40 As the DA begins to close, the systolic component of the murmur often remains audible. Low-intensity left-sided systolic murmurs are commonly heard through the first months of postnatal life. It has been suggested that these are most likely due to turbulence created during left ventricular ejection, although others have suggested that flow through the DA may persist for weeks to months.41 Loud murmurs that persist beyond 7 days of age, or any murmur that is accompanied by signs of cardiac disease, such as poor growth, cyanosis, lethargy, or exercise intolerance, should be referred for echocardiography. Auscultation of both sides of the thorax is important because right-sided cardiac murmurs are a feature of several congenital cardiac anomalies. Occasionally serious cardiac defects may not be associated with audible murmurs. Although most congenital cardiac diseases are detected in foals or young horses, some defects do not become apparent until the horse is required to perform or may occur simply as incidental findings in older horses. Distal extremities should be free of edema and warm to the touch. Limb edema can occur for several reasons, but most commonly as a result of asphyxia or in response to inappropriate fluid therapy in oliguric or anuric foals. Limbs that are cool or cold are poorly perfused and will typically have weak arterial pulses. However, the relationship between peripheral pulse pressure and hypotension is not consistent; hypotension is not always associated with weak pulses and, conversely, weak pulses do not always indicate hypotension.42 Arterial thrombosis should be suspected if a single limb is cold, although an aortic thrombosis could result in decreased perfusion to both hindlimbs.43 Pulse quality can be assessed in the distal limbs using the great or dorsal metatarsal arteries on the lateral aspect of the hind cannon bone. In the forelimbs the brachial artery can be palpated at the level of the medial collateral ligament of the elbow joint. Several methods are available to assess arterial blood pressure. Direct blood pressure monitoring is ideal because it is accurate and continuous, but it is invasive and difficult to maintain, and it can be complicated by vessel thrombosis or sepsis. More commonly blood pressure is monitored indirectly using oscillometry or Doppler-based devices over the coccygeal, brachial, or great metatarsal arteries. An infant-sized inflatable cuff (bladder, 52 mm) placed snugly around the base of the tail yields data that are comparable to mean arterial measurements taken directly from a catheterized great metatarsal artery in a day-old foal weighing between 44 and 69 kg.44 The technique tended to underestimate systolic and overestimate diastolic values, although the differences were not large. The mean arterial pressure of a healthy Thoroughbred foal using an oscillometric device was reported to be 95, 100, and 101 mm Hg at days 1, 2, and 3, respectively.45 Other noninvasive methods to measure cardiac output, such as volumetric echocardiography, have shown good correlation with more robust but invasive techniques in anesthetized foals. The question remains if this correlation will be sustained in conscious, critically ill foals.
Assessment of the Newborn Foal

Neonatal Behavior
Parameter
0 Points
1 Point
2 Points
Appearance
Gray or blue mucous membranes
Pale pink mucous membranes
Pink mucous membranes
Pulse (Beats per Minute)
Absent
<60, irregular
>60, regular
Grimace
Nasal stimulation
No response
Grimace
Strong grimace, sneeze
Ear tickle
No response
Head and neck motion
Ear tickle, head shake
Thoracolumbar stimulus
No response
Head and neck motion
Attempt to stand with head, neck, limb motion
Activity (Muscle Tone)
Limp, lateral recumbency
Semisternal, some limb flexion
Sternal
Respiration (Breaths per Minute)
Absent
<30, irregular
>30, regular, can whinny
Maternal Behavior
Physical Assessment
Rectal Temperature
Ears
Eyes
Oral Cavity

Thyroid Gland
Neck and Back
Gastrointestinal System
Abdominal Ultrasound.
Abdominal Radiography.
Abdominocentesis.
Cardiovascular System
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Assessment of the Newborn Foal
Chapter 16



