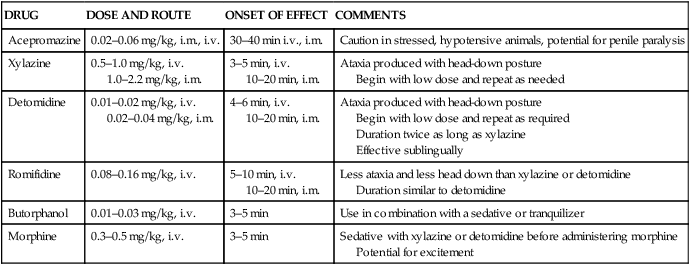
The initial question when discussing anesthesia of the equine athlete is ‘Are there any horses that aren’t athletes?’ Compared with many other species, such as cows and cats, the answer is probably no. Having answered this initial question, there are suggestions in the literature that ‘fit’ horses, particularly ‘fit’ Thoroughbred horses, are more difficult to anesthetize than other horses.1,2 Anecdotally, this increased level of difficulty seems to center on lower respiratory rates in ‘fit’ horses and issues of temperament. A search of the literature reveals few differences in respiratory and cardiovascular function in horses at rest, whether untrained, trained, or detrained. Training increases peak oxygen uptake without changing peak minute ventilation; thus the ratio of minute volume to oxygen uptake (the ventilatory equivalent for oxygen) decreases.3 A reduction in the ventilatory equivalent indicates that a fit horse exchanges a smaller ventilatory volume to maintain a given oxygen uptake than the same horse when detrained. Further, the respiratory pattern in trained and untrained horses is similar, implying increased efficiency of oxygen extraction at the pulmonary level. This increased efficiency of oxygen extraction may partially account for the decreased respiratory rates observed in anesthetized ‘fit’ horses. Alveolar tensions of anesthetic gases rise at a slower rate in horses with slow respiratory rates, potentially delaying the attainment of brain anesthetic gas tensions sufficient for anesthesia. The potential decreases in respiratory function could be further exacerbated by the effects of anesthetic drugs and body position on the function of respiratory muscles and interruption of the normal, unique breathing strategy seen in this species.4 Training does not alter resting heart rate, stroke volume, or cardiac output in the resting horses, but total red cell volume increases and plasma volume increases as much as 29%.5–7 The increase in plasma volume may increase pre-load and enhance cardiac output in exercising ‘fit’ horses.8 Other changes potentially pertinent to anesthesia include an apparent increase in muscle glycogen, muscle capillarization, and muscle mitochondrial density in ‘fit’ horses.9 These questions should be asked of the responsible party prior to anesthesia: 1. Has the horse been anesthetized previously? If so, what were the circumstances and were there any problems associated with the anesthetic period? Many athletic horses have been previously anesthetized, most without incident. Potential problems that could be uncovered by this question include untoward reactions to drug administration, excitement during induction or recovery, prolonged recovery, or rhabdomyolysis. 2. Is the horse tolerant of exercise? Horses that are intolerant of exercise may not tolerate anesthesia. Potential causes of exercise intolerance include ataxia, respiratory insufficiency, upper airway obstruction, and cardiac insuffciency, including atrial fibrillation or other arrhythmia, or rhabdomyolysis or other muscle diseases. 3. Has the horse recently experienced any respiratory disease? Anesthesia compromises resistance to respiratory disease in a number of ways including depression of mucociliary and immune function, loss of the cough reflex, drying of the airway, and inhibition of nasal and laryngeal function. In normal animals these changes are short-lived, but in horses incubating respiratory disease, anesthesia may predispose to worsening signs and exacerbation of disease. 4. Does the horse make a respiratory noise at rest or during exercise? Anesthetic agents, notably the alpha2-adrenoreceptor agonists, cause relaxation of the upper airway including the larynx.10–12 This relaxation may augment a pre-existing condition resulting in partial or full respiratory obstruction. Such obstructions can be overcome with endotracheal intubation but may be problematic during recovery. 5. Has the horse ever tied up (rhabdomyolysis)? There is considerable evidence of genetic, gender, and breed predisposition for rhabdomyolysis.13 Anesthesia can be a triggering event. 6. How does the horse react to new experiences? There is considerable variation amongst equines in their ability to adapt to new situations and experiences. Some horses are apparently calm despite being placed in stimulus-intensive environments while others become agitated without apparent provocation. The demeanor of the patient potentially affects the required doses of sedatives and may change preparations for anesthesia and recovery. 7. Is the horse receiving any medication? When was the last time the horse was medicated? Some individuals utilize long-acting tranquilizers and other drugs as part of their training regimens. The administration of drugs such as acepromazine, fluphenazine and reserpine can affect the required doses of anesthetic agents and the resultant pharmacologic response. The cardiovascular system is easily evaluated by palpating the pulse of a peripheral artery, checking the color of mucous membranes, measuring the capillary refill time, assessing skin turgor, and ausculting the heart. Normal pulse rates in quiet adult horses range from 25 to 45 beats per minute. Interruptions in the regular rhythm (pauses) are not uncommon in fit horses and are usually the result of sinus arrhythmias or second-degree atrioventricular blockade. A brief period of exercise should stimulate an increase in heart rate and resolve the arrhythmia. The most common pathologic arrhythmia in horses is atrial fibrillation.14 Presumptive diagnosis of atrial fibrillation can be made on physical examination by palpating pulses of unequal strength occurring at irregular intervals and by ausculting variable-intensity heart sounds at varying intervals. An electrocardiogram should be obtained if pauses in the pulse rhythm do not respond to exercise or if there are pulses of variable intensity occurring at variable intervals. Heart murmurs can be ausculted in the majority of race horse.15 Most are systolic murmurs, heard best at the heart base. Murmurs of grade II (out of VI) or less are interpreted as innocent flow murmurs if there is no other evidence of heart disease. Murmurs of potential significance include those that result from mitral valve insufficiency, aortic insufficiency or congenital ventricular septal defects, but they comprise less than 0.1% of the population. Additional information can be obtained via electrocardiography and echocardiography. Pre-anesthetic medications in the horse include anticholinergics, tranquilizers/sedatives, and analgesics (Table 57.1). The administration of the anticholinergic agents atropine and glycopyrrolate is not recommended for routine use prior to anesthesia in horses. Anticholinergics decrease salivation and increase heart rate, but neither excessive salivation nor bradycardia is a frequent problem in the horse. The potential disadvantages (postoperative ileus, tachycardia, and increased myocardial oxygen consumption) are significant; thus anticholinergic administration should be limited to those cases where it is specifically indicated. Common cardiac arrhythmias that respond to anticholinergic agents include atrioventricular conduction disturbances, interference dissociation, and sinus bradycardia (heart rate less than 25 beats/min) with hypotension. Table 57.1 Drug used for standing chemical restraint and as pre-anesthetics Alpha2 adrenoreceptor agonists produce sedation, muscle relaxation and analgesia when administered intravenously or intramuscularly to horses.16–19 Horses that have received alpha2 agonists assume a ‘head-down’ or ‘sawhorse’ stance and may frequently shift their weight from side to side (Fig. 57.1). Arterial blood pressure is initially increased due to drug-induced increases in peripheral vascular resistance. Hypertension may be sustained (20 to 60 minutes), particularly when detomidine or romifidine is used. Decreases in heart rate, sinus arrhythmia, and first- and second-degree atrioventricular blockade are common. These decreases in heart rate result in significant decreases in cardiac output, often to levels 50% of pre-drug values. Respiratory rate is usually decreased, but tidal volume increases. Relaxation of the muscles of the upper airway can predispose the horse to stridor. The administration of an alpha2 agonist decreases salivation, gastric secretions, and gastrointestinal motility and increases urine volume. Other incidental effects of alpha2 agonist administration include increases in intrauterine pressure, hyperglycemia and hypoinsulinemia.
Anesthesia of the equine athlete
Introduction
History
Physical examination
Cardiovascular system
Pre-anesthetic medications
DRUG
DOSE AND ROUTE
ONSET OF EFFECT
COMMENTS
Acepromazine
0.02–0.06 mg/kg, i.m., i.v.
30–40 min i.v., i.m.
Caution in stressed, hypotensive animals, potential for penile paralysis
Xylazine
0.5–1.0 mg/kg, i.v.
1.0–2.2 mg/kg, i.m.
3–5 min, i.v.
10–20 min, i.m.
Ataxia produced with head-down posture
Begin with low dose and repeat as needed
Detomidine
0.01–0.02 mg/kg, i.v.
0.02–0.04 mg/kg, i.m.
4–6 min, i.v.
10–20 min, i.m.
Ataxia produced with head-down posture
Begin with low dose and repeat as required
Duration twice as long as xylazine
Effective sublingually
Romifidine
0.08–0.16 mg/kg, i.v.
5–10 min, i.v.
10–20 min, i.m.
Less ataxia and less head down than xylazine or detomidine
Duration similar to detomidine
Butorphanol
0.01–0.03 mg/kg, i.v.
3–5 min
Use in combination with a sedative or tranquilizer
Morphine
0.3–0.5 mg/kg, i.v.
3–5 min
Sedative with xylazine or detomidine before administering morphine
Potential for excitement

![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Veterian Key
Fastest Veterinary Medicine Insight Engine
